memo ���ſ�
������롥
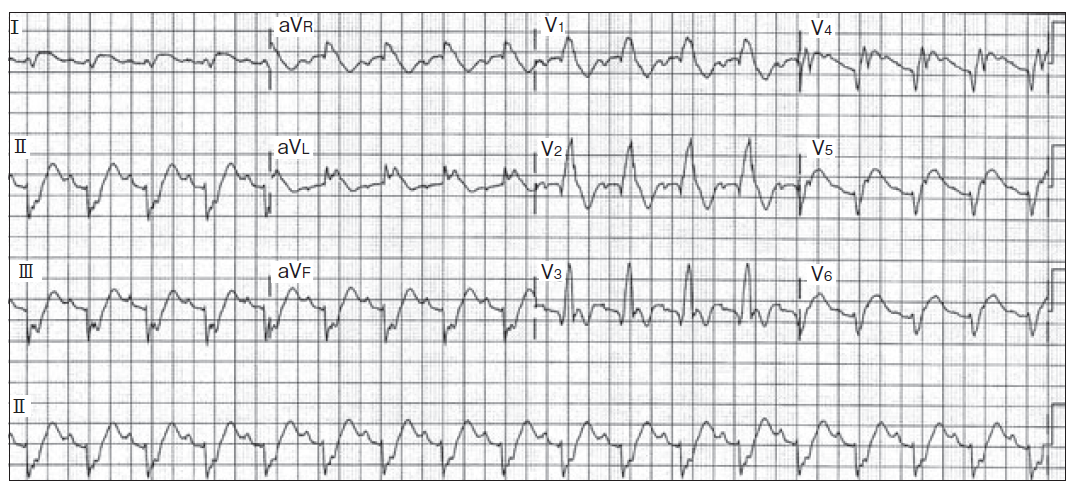
GE #71, GE #260
�������2013ǯ�����Ҳ���
Utah ECG outline
100 ECGs in the Fast Lane
ECG library A-Z
index.php
Google
�ز�Ƚ����
minesota2005.pdf
���ܿ��ſز��Ѹ콸
final.pdf
Luna Basicd ECG
code1.pdf
ECG.pdf
Channel.pdf
 II < 0 �ʤ� -30��ʲ�
III <0 �ʤ� 30��ʲ�
II < 0 �ʤ� -30��ʲ�
III <0 �ʤ� 30��ʲ�
�� ��ʸ��̾����ɽ���ſޤο��������
2019ǯ 7�� 10�� ������ 08:26:05 JST
�� ���ڹ��ɤǤΰ۾�Q�Ȥ�ȯ����ͳ���狼��ʤ���
2019ǯ 5�� 24�� ������ 08:12:33 JST
�� R�ˤ�F�ˤ��Ű̺���ECG�������Ǥ���Τʤ顤IͶƳ���R�Ȥ��Ṳ̋�
�����������L�ˤ��Ṳ̋����н����Ϥ��Ǥ��롥�����R�ˤ�F�ˤ�
����κ�����Ψ��ɽ���Ǥ����������
�� ���ɹ��ɤ�ȯ������ȡ�V1��V2��R�Ȥ����⡤ST�㲼����������оΤ�T�Ȥˤʤ롥
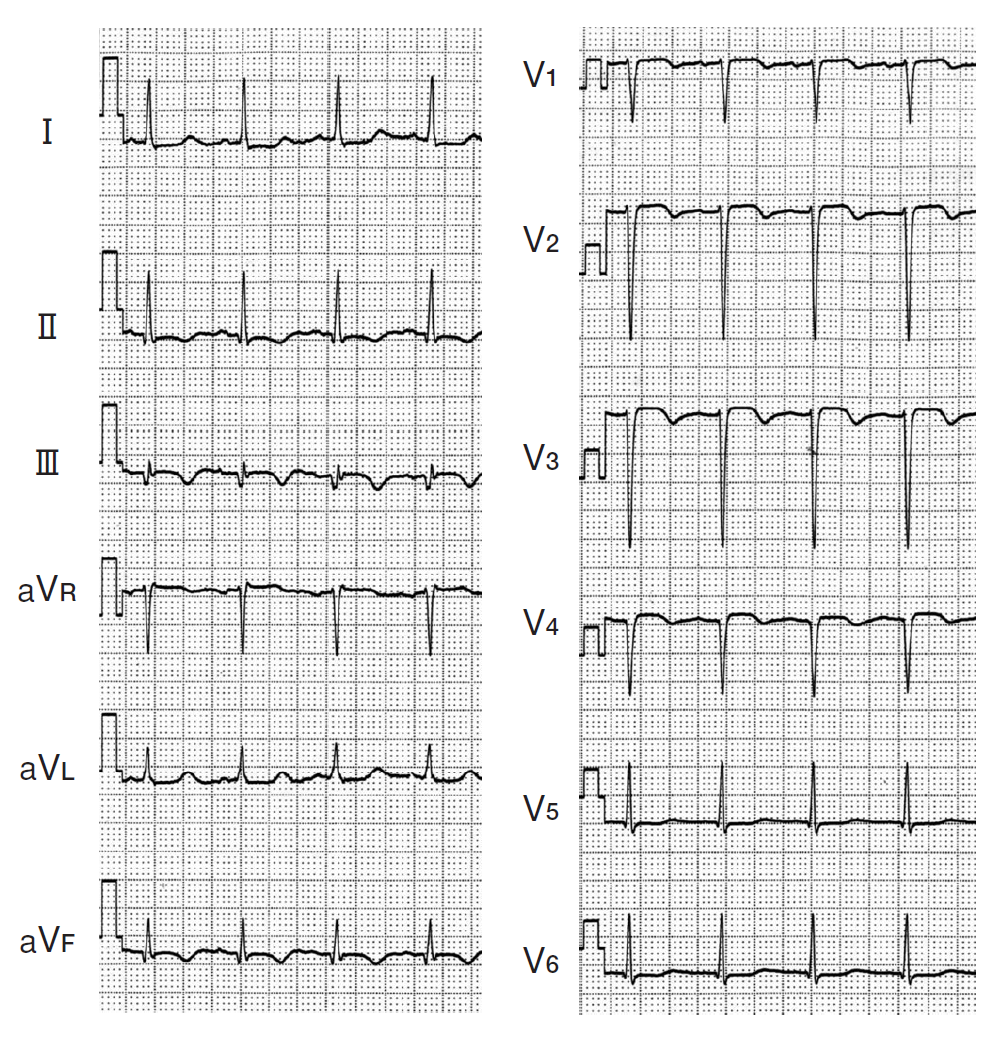
12 Lead ECG p. 472.
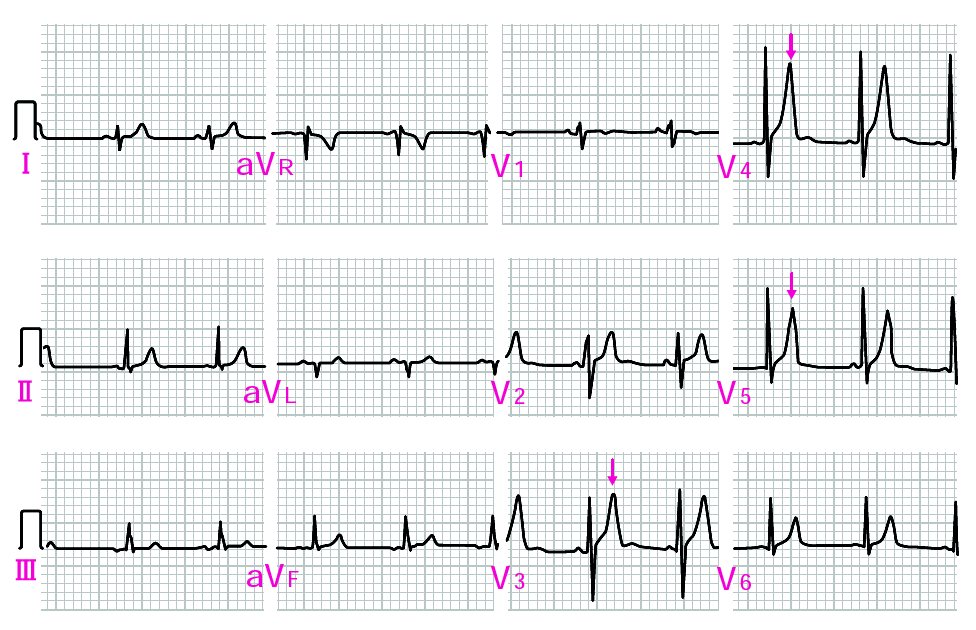
ECG 15-28
ECG 15-29
���ɹ��ɤΥߥ顼�������ST�㲼�������T�Ȥ�final p.52�Dz��⤵��Ƥ��롥
��������V1-2��R�Ȥ��������Ǥ��ʤ���
2019ǯ 5�� 23�� ������ 08:12:33 JST
�� ����ޥ��ͥ�������
�� ���㥫�륷������
�� �������Ǥ�PR�㲼
�� �㥫�ꥦ���ɤǤ�U�Ȥ�IKr����ͥ�
�� �������ꥹ�ˤ���ư�Ű�2����㲼��IK(Ca)�Ȥδط�
�� U�ȤΥᥫ�˥����ʬ��
2019ǯ 9�� 23�� ������ 23:28:33 JST
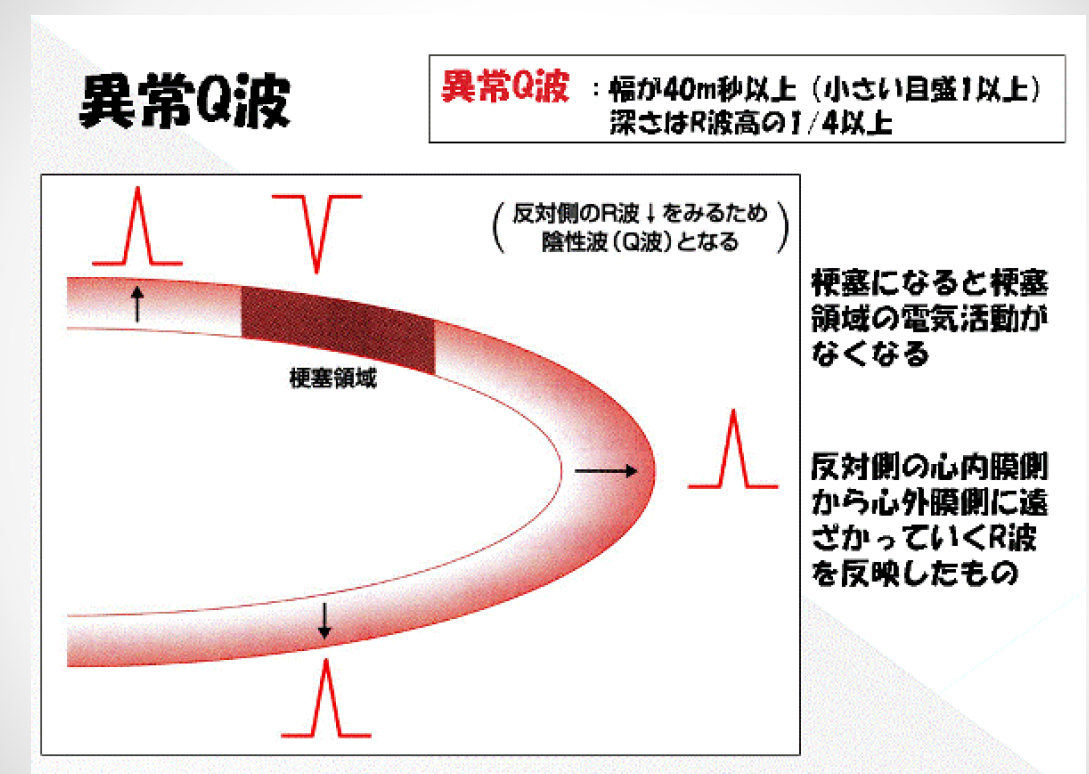
�۾�Q�Ȥ�ȯ���ᥫ�˥�����ľ�����ȡ�
�����첼���ɤ�GE #293����ˤ��������
final pp.63���ľ�����ȡ��۾�Q�ȤˤĤ������������ھɤ���ˤ��Ƥ�褤��
�ҥ�ξ������æʬ�ˤλ��ַв�: fainal.pdf��p.25
Block�Ǥ�T�Ȥ��Ѳ� p. 409
�������硧R V5 or V6 + S V1 >35mm; R in aVL >11mm
QT 0.3��0.45 QTC 0.34��0.425
111 ��Ͽ����
112 �ŶˤΤĤ��㤤
121 ȿ���ײ�ž (V1��Rs��V6��high R)transition��v3�ʲ�
122 ���ײ�ž (V1��high R�� V6��high S) transition��v4�ʾ�
131 ���Ű�(�ͻ�ͶƳ)
141 QT��Ĺ c 142 QTû�� c
151 ������
161 �⤤T��
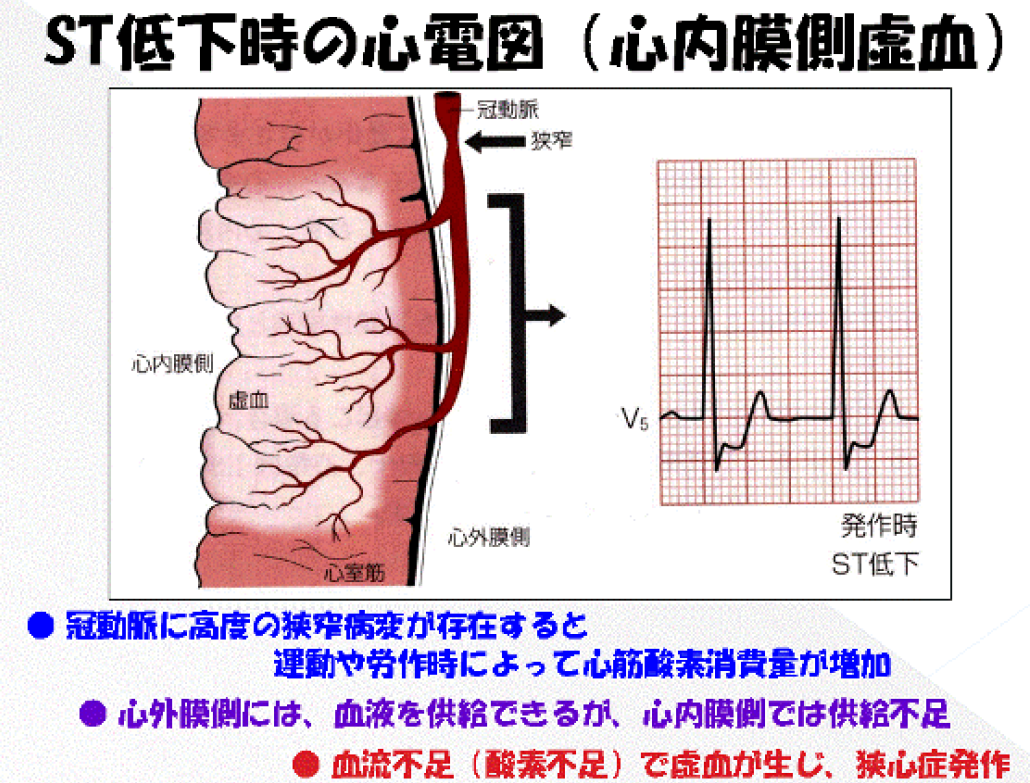
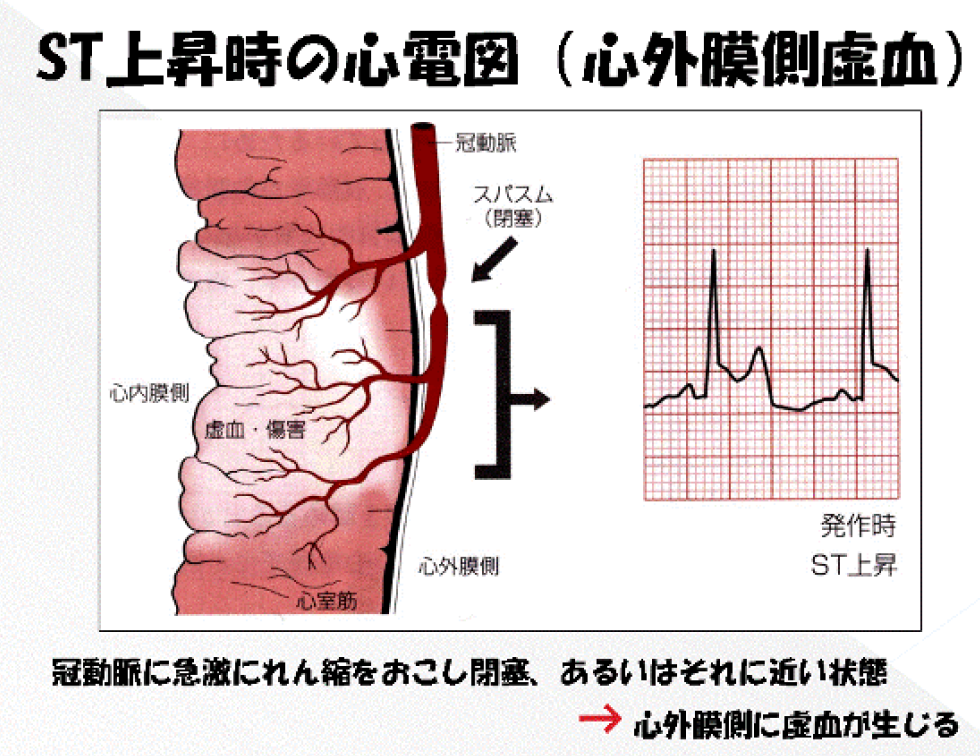
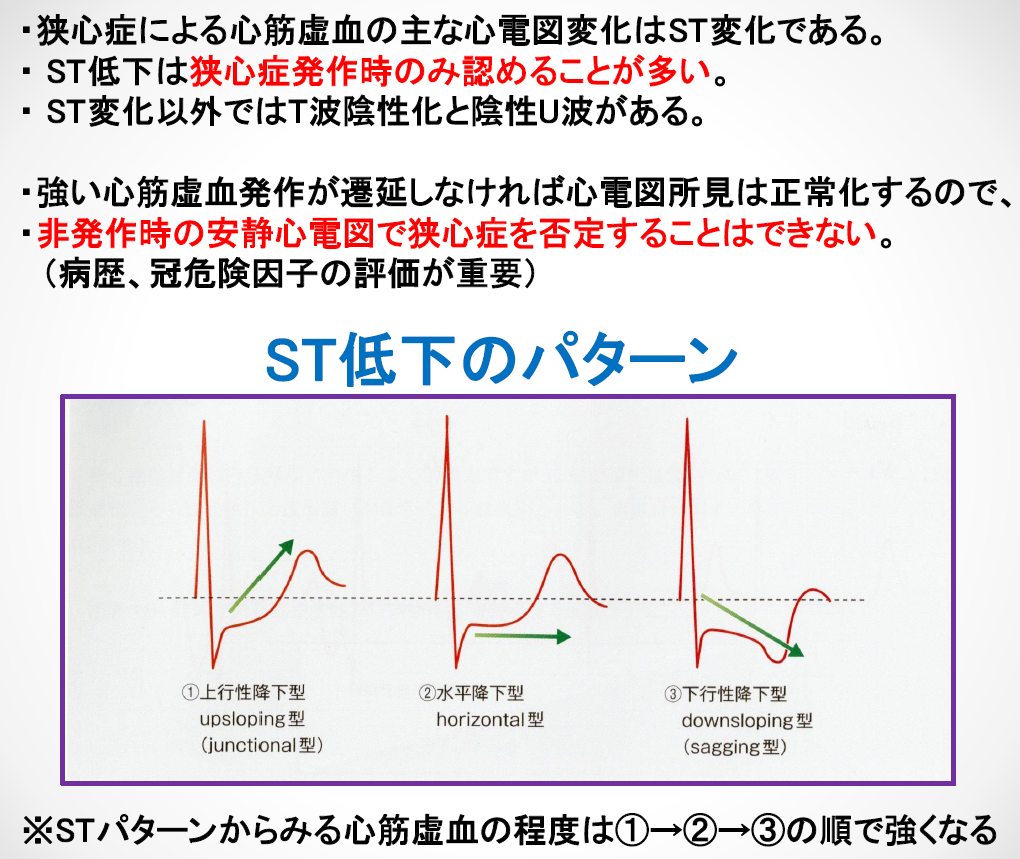
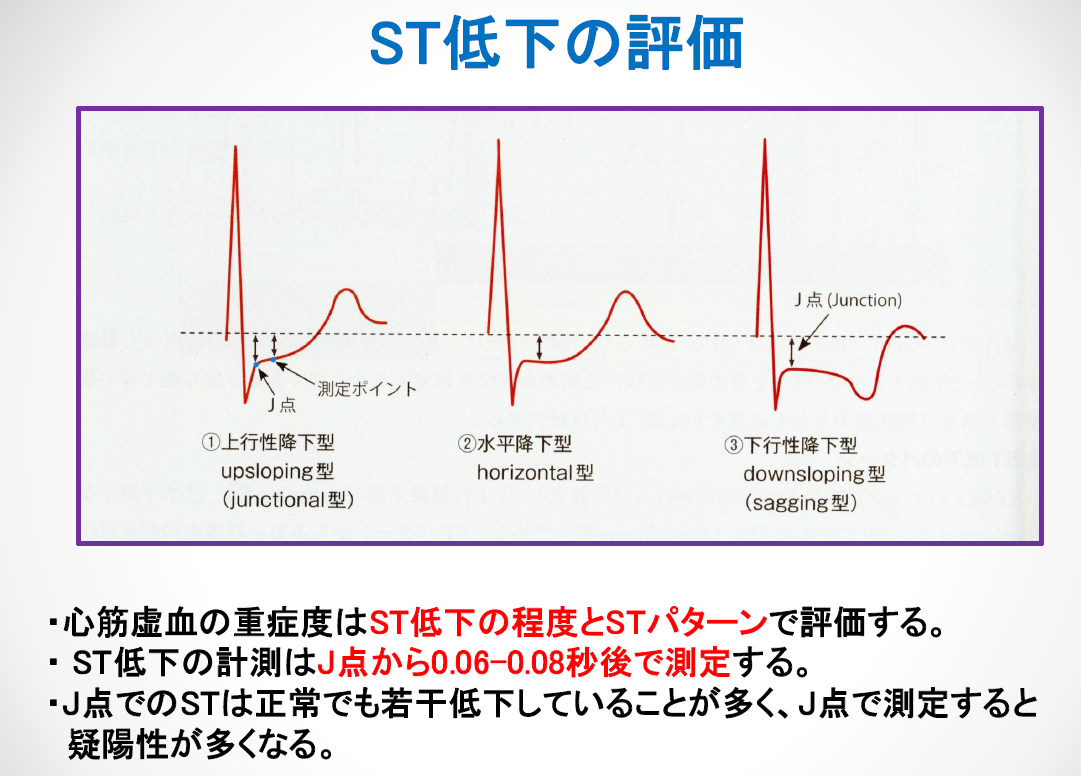
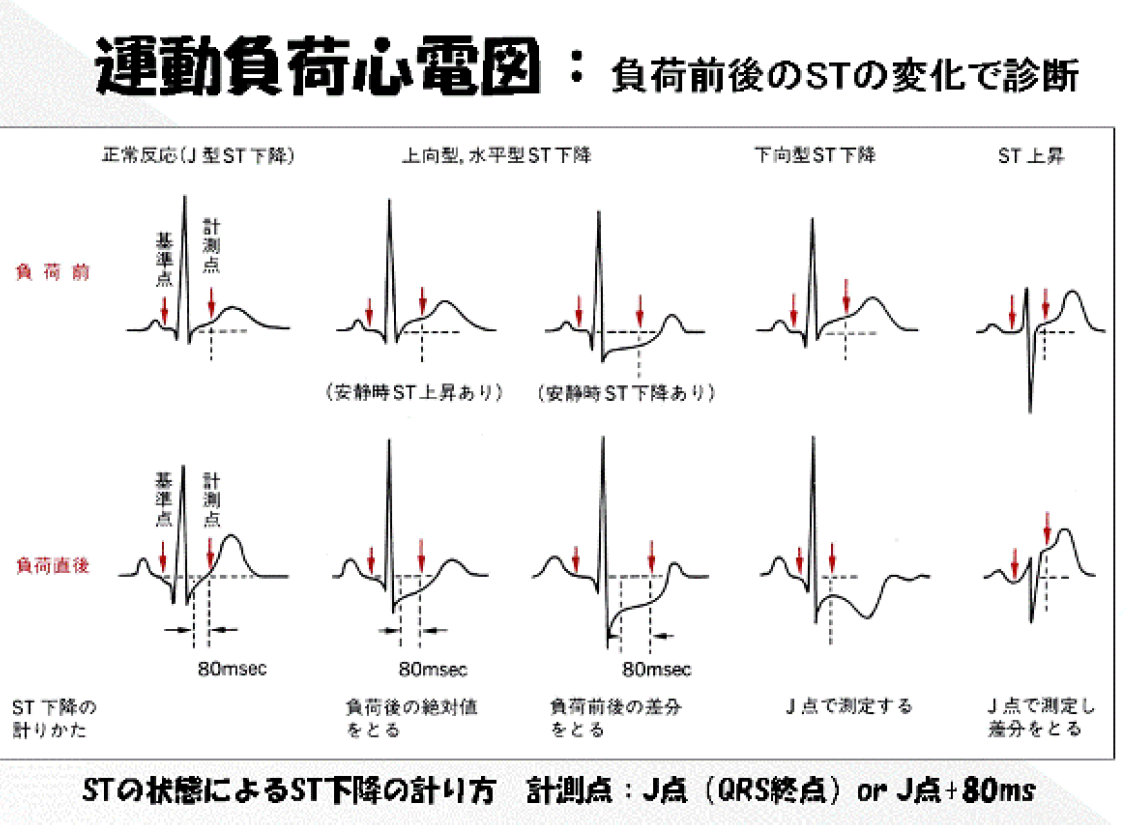
171 ST�徺
172 ST�㲼
174 ��Ƴ�ٱ� (�������դ���)
201 ���꼴
202 ���٤ʺ����а� 203 �����а� 90��ʾ�
204 ���٤ʱ����а� 205 �����Ѱ� -30��ʲ�
206 S1S2S3
300 �������� V1 r��>5mm��R/s >1 c
301 �������Ű� c ST�Ѳ��ξ�� d
303 ���٤ʱ������硥
304 ����������
306 ���������� (S1Q3)
307 ��˼��� b 308 ��˼��� b
315 ��������
401 P-Rû�� 410 P-R��Ĺ
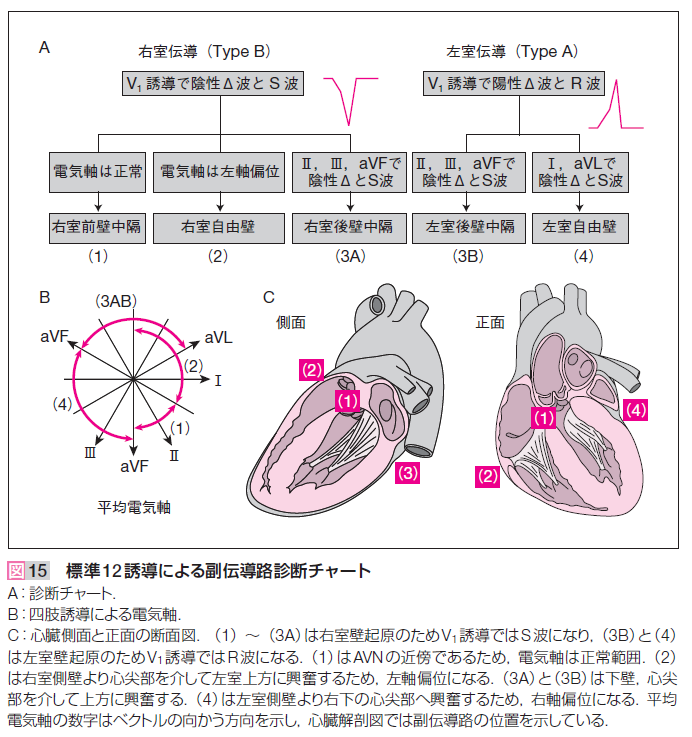
402 WPW�ɸ���
411 I��˼���֥��å� c
412 II��˼���֥��å�(Wenckebach) d
500 �ڡ����������ư
501 �Դ������ӥ֥��å� b
502 ������֥��å�
503 �Դ������ӥ֥��å� b V1,V2�ο���rS�ȡ�I, aVL, V5, V6��q�Ȥ��ʤ���QRS��0.12�ð���
504 �������ӥ֥��å� c
505 �������ӥ֥��å� d
511 �������ޥ֥��å� <-30��avL��R�ȡ�III��S�ȡ�c
512 ���Ӹ�ޥ֥��å� >90�� aVL��Q�ȡ�I��S�ȡ�c
521 ξ�ӥ֥��å� d
611 ʿ��T c
621 ����T (5mm�ʲ� c������ʾ� d)
622 ����U
623 ������U
624 ���ð�ŪT�Ȱ۾� c
632 ����ST��T�۾�
633 ST��T�۾�
701 R�Ȥ���������
712 ���ڵ��쵿��
721 �����첼����
731 ���ɹ��ɤε���
732 ¦�ɹ��ɤε���
733 ���ɹ��ɤε���
734 ������ֹ��ɤε���
735 ��̸��ɹ���orȿ���ײ�ž����
742 ¦�ɹ��ɤβ�ǽ��
743 ���ɹ��ɤβ�ǽ��
744 ������ֹ��ɤβ�ǽ��
745 ��̸��ɹ��ɤβ�ǽ��
752 ¦�ɹ���
753 ���ɹ���
754 ������ֹ���
774 �ĵ���������ֹ���
801 ������̮ƶĴΧ
802 ��˼ĴΧ�ε���
803 �۽����弼��ĴΧ
811 ƶ����̮ 45-49 A, 40-44 C
812 ƶ����̮ 101 > D2
813 ��̮ 101 > D2
814 ��̮ 45-49 A, 40-44 C
821 ƶ������̮
841 �弼����������
842 ��������������
843 �弼������̮
844 ����������̮
845 �弼��������(��ȯ)
846 ������������(��ȯ)
847 �弼������̮
848 ����������̮
871 ��˼��ư d
872 ��˼��ư d
881 ����Ǥ��ʤ�����̮
883 ����P
998 �֥륬���� (9-2-3, 9-2-4)
��˼���� final p.79
IMG_20170912_0005.pdf
Brugada final p.70
? Brugada�ζ���ͶƳ��S�Ȥ�¸�ߤ��뤫��
������¸�ߤ��Ƥ�褤��
GE�ΰ۾�Q��
#185, #183, #189, #190(WPW)
12-Lead ECG
aberrant intraventricular conduction �������ѹ���Ƴ
ACS Acute coronary syndrome
AT Atrial Tachycardia
AVNRT ˼������ꥨ��ȥ������
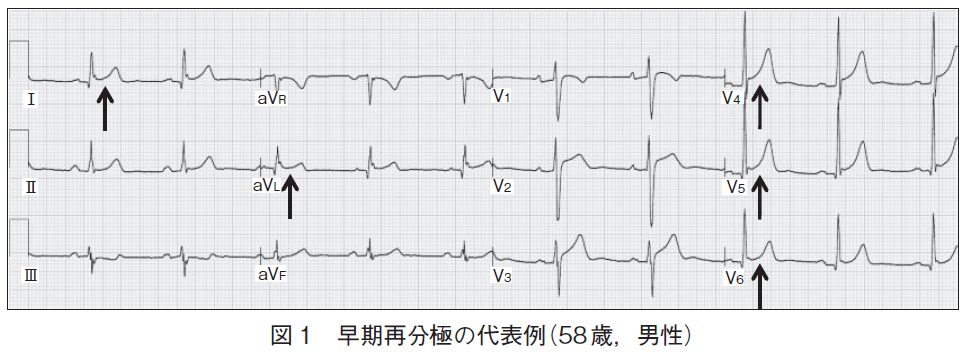
BER Benign Early Repolarisation (���������ʬ��)
CABG coronary artery bypass grafting ��ư̮�Х��ѥ���
CAD coronary artery disease
DCM dilated cardiomyopathy (��ĥ�����ھ�)
DPW �����Ƴϩ(���˼��������Ƴϩ)
FPW Fast Pathway ®��Ƴϩ
HCM hypertrophic cardiomyopathy (��ĥ�����ھ�)
IACD intraatorial conduction delay, �ͻ�ͶƳ��P�Ȥ�����Ƕ���ͶƳ��
RAE��LAE�ξ��֤���
ID intrinsicoid deflection final p.82
12 Lead �Ǥϴ�������R�Ȥ�ĺ���ޤǤλ���(VAT)�����ޤ���
ĺ����������ޤǤλ��֤�late intrinsicodd deflection�Ȥ�����
ecg 11-10, GE #298.
ID��ȯ��������ͳ�Ͽ�����¦���ڤ�æʬ�˻��֤��ٱ�Τ��ᡥ
VAT���ٱ�Ͽ�����¦���ڤ�æʬ�˻��֤��ٱ�Τ��ᡥ
idioventricalr rhythm ������ͭĴΧ
accelated idioventricalr rhythm ¥����������ͭĴΧ
IRBBB incomplete right bundle brach block��V1��RSR'��qR'��qR�ȤϽʤ���
R:S ratio��ɬ���礭���ʤ롥
intrinsicoid deflection
R�Ȥ�Ω��꤫��ĺ���ޤǤλ��֤���VAT��Ʊ����p.45, final p.82.
late intrinsicoid deflection��ĺ��������������ޤǤλ��֡�
irregularly irregular ����Ū����̮
wandering atrial pacemaker, multifocal atrial tachycardia,
atrial fibrillation.
IVCD intraventricular conduction delay, 94, 141,198, 289-292, 504-509,
522, 621, 626, 657, QRS�ǥ��������ˤʤ롥
236, 14-8 ��K��ɤ�QRS����0.12�ðʾ�˱�Ӥ롥
isoelectric R/S�椬1���̣���롥
IWMI inferior wall myocardial infarction p.354
CHF congestive heart failure
ESRD end stage renal disease
IWMI inferior wall miocardial infaruction
ECG 13-31 (p.308 S1Q3�Ǥ��뤬��IIIͶƳ��J���徺��
aVL��J���㲼(�ߥ顼�����)��
LAA Left Atrial Abnormality.
LAD Left axis deviation�������а̡�(���ɹ��ɤǤ�II,III,aVF��QS�Ȥʤ뤫�顤
����LAD�Ǥ��롥LAFB�ȤϿ��Ǥ��ʤ���
LAE Left atrial enlargement
��˼�����V1��2�����ǹ⤵������0.3mmsec�ʾ塥
LAFB Left anterior fascicular block���������ޥ֥��å���
LAH LAH�ˤ�r�Ȥ�¸�ߤ��롥�ʤ���в��ɹ��ɡ�V6��S�Ȥ�¸�ߤ��롥p.296
Left anterior hemiblock4
LBB ���ӥ֥��å��ˤ�V1��r�Ȥ�¸�ߤ��롥̵�����������ֹ��ɤ�ȼ����
left main stem ���紴�� �����ԻޤȲ����ޤ�ʬ���������η�ɡ�
LPFB left posterior fascicular block
��˺������ɤ���ʳ���뤿�ᾮ���ʺ�������ζ�ʳ�����ꡤ���θ屦����
�礭����ʳ���롥�������äơ�II, III, aVF��T�Ȥϵ�ž(flip)���롥
axis 90��ʾ塤I��aVLͶƳ��rS�ȡ�III��aVFͶƳ��qR�ȡ�
V1ͶƳ��r�Ȥ��ʤ����Ȥ⤢��(p.303)��
RAE��˼�����RVH���������������뤳�ȡ�
�Ǥ����Ū�ʱ����Ѱ̤ϱ�������Ǥ��롥
����¦�ɹ��ɤⱦ���Ѱ̤ˤʤ롥
��ޤ���������ʬ�ۤ����֥��å��ϵ�(200��3000���1�١�p.301)��
LPH left posterior hemiblock (LPFB��Ʊ��)��
MAT Multifocal atrial tachycardia
NSTEMI non-ST-segment elevation myocardial infarction
NSSTWC non spacificd ST wave change
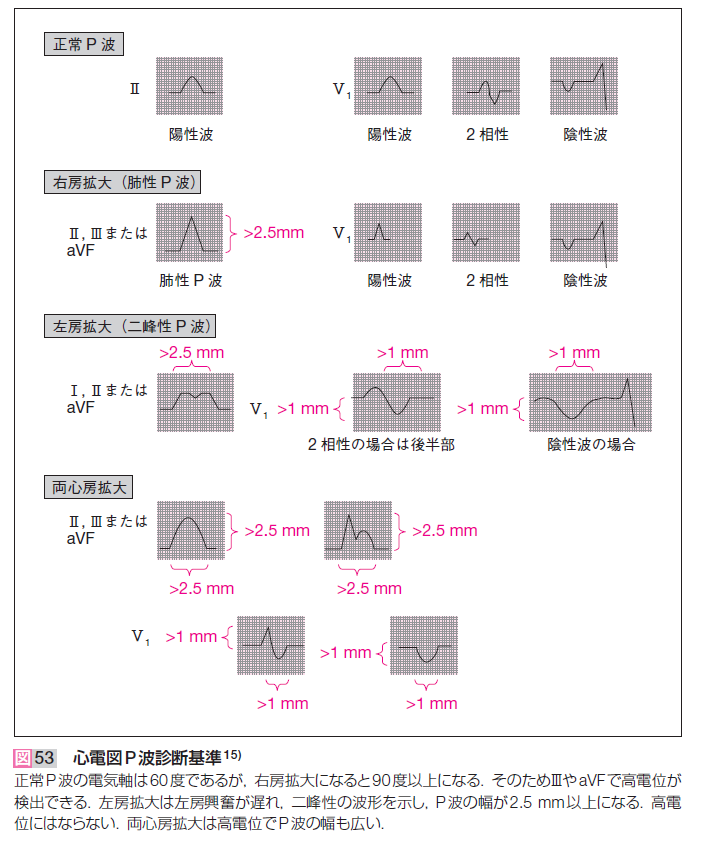
P-mitrale ��˼��P��I,IIͶƳ��0.12sec(3mm)�ʾ��P�Ȥ�M�ͤΥΥå���ȼ����
��ĤΤ���(hump)��ĺ���δֳ֤�0.04sec(1mm)��ɬ�ס�
P-pulmonale ����P��IIͶƳ��2.5mm�ʾ�ι⤵��
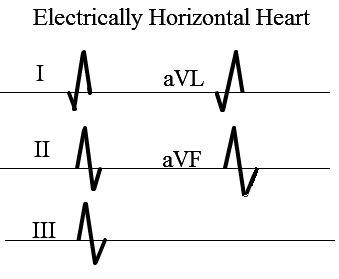
PRP poor R wave progression, ���ײ�ž�Ǥ⤽�Τ褦�˿��Ǥ��롥GE #298.
PRP��V3-6��R/S������ä����ʤ����Ȱ�̣���롥Axis <-30�ʤ�����
�٥��ȥ������V3-5��R�Ȥ����ä��ʤ���LAFB��PRP�ˤʤ롥
PSVT ȯ�����弼���AVNRT���Ǥ�¿����final p.125
RAA right atrial abnormality
RAD right axis deviation
RAE right atrial enlargement
RFCA ����ȥ��ơ��ƥ륢�֥졼�����
RVH right ventricular hypertorophy
LVH��ȼ��RVH��V1��R�Ȥ�ȼ��ʤ�(P. 362, ECG 14-25)��
S1Q3T3 right ventricular strain pattern (p.85, 302, 359)
���Υѥ������LPH��PE��Ʊ���Ǹ�����Ǥɤ��餫Ƚ�Ǥ��롥
RVH�Ǥ�Ʊ���ѥ�����ˤʤ�(P.305, ECG13-30)��
septal Q aVL��Q�ȡ�septal Q�������LBBB������Ǥ��롥GE #243
��֤Ǥκ��Ӥ��鱦�Ӥ˸�����r�Ȥ�aVL��q�Ȥ˸����롥
LBBB�ǤϤ���q�Ȥ�¸�ߤ��ʤ��ȹͤ���о��ʸ�Ϥȹ�����������
â����12 Lead�Ǥ�V1��r�Ȥ�¸�ߤ��Ƥ�LBBB�ȿ��Ǥ��Ƥ��롥
�����Դ����֥��å�(ILBBB)�Ǥ�I, aVL��q�Ȥ�̵����R�Ȥ��������ɡ�
SPW Slow Pathway ����Ƴϩ
ST Sinus Tachycardia
STEMI ST-elevation myocardial infarction��ST�徺�����ڹ���
strain T waves
RVH�Ǥϥԥ��ĥ�ä���̣�ǿ�ʿ��ST�������Ȥ���
LVH�Ǥ�V4����V6�ޤǡ�R�Ȥ��Ф���ST depression,
Concave Downward, Flipped Asynmetric T wave��
V1����V3�ޤǡ�S�Ȥ��Ф���Concave Upard,
ST Elevation Upright Asynmetric T wave (p. 363)��
three-vessel 3��(�����Իޡ������ޡ�����ư̮)����
Tp(Ta) P�Ȥκ�ʬ��T��
UA Unstable angina
uncertain age ȯ��������
upward convex ����̡�(ST�������ȤǤ�ɽ��)
concavity�ϱ�����
�̾��ST�������Ȥ�upward concavity�Ǥ��롥
V1��R��
RVH��RBBB�����ɹ��ɡ�WPW type A, �Ҷ��ȼ�ǯ
���ȥ쥤���ޤ�ſޥ��ޥ
VAT ventricular activation time final p.82.
������¦æʬ�˻��֤���������Ǥ���VAT���ٱ䤹�롥ID���ٱ䤹�롥
VTach ventricular Tachycardia ��������
��˼ĴΧ�Ȥβ�Υ��dissociated atrial rate�Ȥ�����p. 75
WAP wandering atrial pacemaker, ecg 9-8
Durrer.png
Junctional 40��60 BPM
Accelerated Junctional 60��80 BPM
Idioventricular 20��40 BPM (������ͭĴΧ)
Accelerated Idioventricular 40��100 BPM
Ventriculara Tachycardia 100��200 BPM
AV dissociation ˼����Υ ��˼�ȿ���ĴΧ��3��Υ֥��å��Ǥ��뤬�������Ʊ����
BB p.55
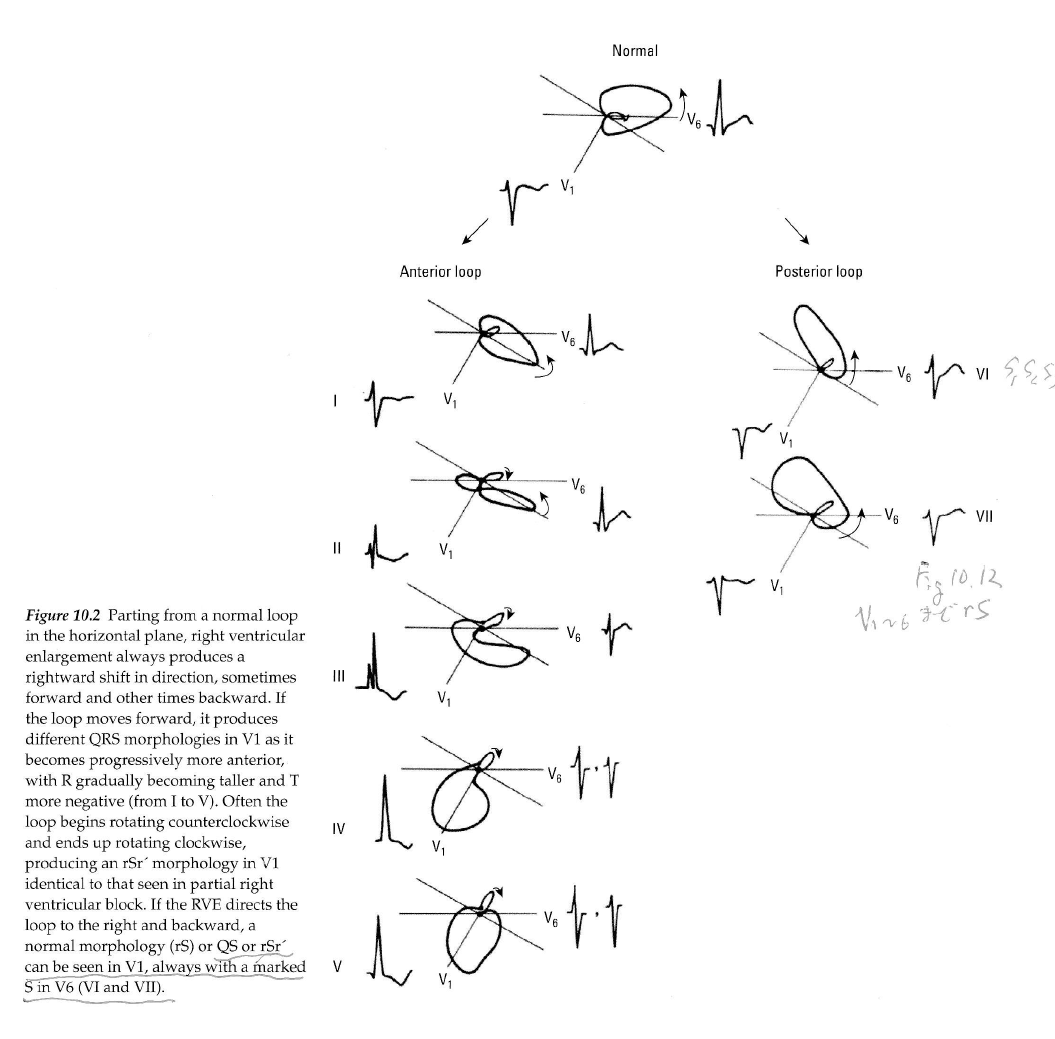
Fig 6.2��ñ�쿴�ڤ�æʬ�˲�����6.3�Ǻ�ʬ�˲�������
���ڤ�æʬ�˲����ǡܥ��ѥ����ȡݥ��ѥ�����Ʊ���˵�Ͽ����Ƥ��롥
Ʊ��������æʬ�ˤȺ�ʬ�ˤ����礦����ʤ�R�Ȥ�T�Ȥο���ϵդˤʤ롥
����������Fig 6.4�˿�˼��æʬ�ˤȺ�ʬ�ˤ��������Ƥ��롥
���ä�P�Ȥ�Ta�Ȥο���ϵդˤʤ롥
�����Ǥ�Fig 6.11A��æʬ�ˡ�6.11B�˵������κ�ʬ�ˤᤷ�Ƥ��뤫��
R�Ȥ�T�Ȥο����Ʊ���ˤʤ롥
���ξϤǤ�T�Ȥε�ž�ϵ��Ҥ���Ƥ��ʤ���
SAH, Ǿ��з�ʤɤǤϿ�����žT�Ȥ�����롥�����ϸ��Ф������ˤ�롥
Essentials of Learning ... p. 138.
�����ФϺ������ɤ���ۡ������ФϺ������ɤ���ۤ��롥ξ¦��
�����������Ƶѡ��֥��å����뤳�Ȥˤ�꿴�ſޤ��Ѳ����褹��
nejmicm020416.pdf
19�������������֥��å��Ǻ�¦Ƭ����»����48���ָ�˶��٤�ST�徺��
ST�㲼��������ո����Ǥ�����������ˤϰ۾郎����������
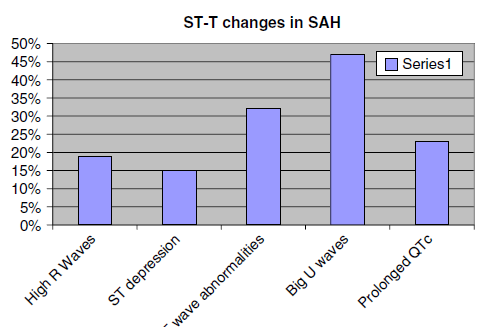
SAH�ˤ�뿴�ſ��Ѳ�����
12471_2010_Article_49.pdf
9-1 biphasic P wave��S1Q3T3�������а̡�V1�ǹ�R��LVH��IRBBB�β�ǽ����
PFB�Ϥʤ���
9-2 PAC���㡤�����Ϻ������ޥ֥��å����ͤ�����T�Ȥ����������Ǥε��Ҥʤ���
��˼P��
9-5 P-mitrale, LVH, IVCD, R�Ȥ�����ǤϤʤ����ꤷ�Ƥ��롥
9-6 P-mitrale, biatrial enlargememnt, LVH(aVL>11mm), LAH
9-7 P-mitrale, Long-QT
9-8 WAP�����P�Ȥ�T�Ȥ����Ѥ�������˹⤤P�Ȥˤʤ롥
9-9 RAE���ĵ���������ֹ��ɡ�
9-10 PAE, PAD, PJC, IRBBB�Ǥ��롥qR'��RVH��¸�ߤ��ʤ���cf ECG 11-15��
IACD V1�Ǥ�2����P�Ȥ�����IACD(intra atrial conduction delay)
9-11 IACD��RAE���㡤LAD, LAH, ��ü�ʻ��ײ�ž��V6�Ǥ�transition�������ʤ���
9-12 IACD��LAE���㡤PJC���ߤ��롥������ʳ��abberancy��
9-13 IACD��LAE���㡤II, III, aVF��Q�ȡ��о���T��ȿž��
II,III,aVF�Ϥ��о���ȿžT�ȡ�V1-6���������оΥ��ȥ쥤��T�ȡ�
�ͻ�Ͽ�ʿST��LVH����˼��١����ɹ���
9-14 LAE��IRBBB���ĵ���������ֹ��ɡ�RVH? �����а̡�II, III, aVF��T�ȵ�ž��
RVH��ɬ�ܡ�cf 11-12.
V1�϶���QR�ȷ���V2�Ͼ�����rS���̾��V1�Τ褦�˸����롥V1-V4�ϱ���
���ȥ쥤��T�ȡ������褦���Ǥ����ζ���S�Ȥϱ����������ħ��
9-15 IACD��LAE���㡤LAH��STD
9-16 IACD��LAE���㡤I, aVL�ʳ������Ƥ�ͶƳ��QS�ѥ�����1���AV�֥��å���
9-17 IACD��LAE���㡤III, aVF��Q�Ȥ����������۾�ǤϤʤ���
I��aVL���礭�ʥΥå���IVCDefect�����������Ṳ̋�I, V5-V6�Υ��ȥ쥤��T��
��˼��١��������硥
9-18 RAE, LAE, �ͻ�ͶƳ��T�Ȥ��ʤ���
9-19 RAE, LAE, IVCD��RBBB�˸����롥
9-20 RAE, LAE, Ta�Ȥ������롥
9-21 RAE, LAE
TESTECG 15
10-1 pericarditis. PR������J���徺��ST�Ͼ�˱���QRS�ν����˥Υå���
����ECG��benign early reporalization�Ȥζ��̤�����
10-2 LGL�ɸ������������ॹ(James)«��final p.112.
V1��R�Ȥ��⤤��ͳ�Ϥ狼��ʤ���AVN�ȤΥ롼�פ�𤷤�AVNRT�ˤʤ롥
��˼�ڡ�����Ԥ��ȸ�����Ƴ���˿����ϻɷ���ɽ����롥
10-3 Type A WPW
10-4 Type A WPW
10-5 Type B WPW, PAC, WAP�����뤬�����Ĥ����V1��V2��Ƚ�롥
����Q�Ȥ�AMI�˴ְ㤨�ʤ��褦�ˡ��ޤ��Դ������ӥ֥��å��Ȥ�ְ㤨�롥
WWW�ɸ���������ȯ����봵�Ԥ���ñ�˦��Ȥ�¸�ߤ������
WWW�ѥ�����Ȥ�����
10-6 Type C WPW, P-R�ֳ֤ϱ�Ĺ��
10-7 Type A WPW, III��aVF�Ǹ�����Υå��ζ���QRS�ϡ�
isolated intraventricular conduction delay(IVCD)��BBB�ȿ��̡�
10-8 Type A WPW, Digoxin���߾�T�ȤˤʤäƤ��롥
10-9 Type B WPW, ���ӥ֥��å����ο��������¦Kent«���̲᤹�뤫��
��������˶�ʳ���롥
10-10 LBBB������˸����뤬���Ȥ�¸�ߤ��롥300 BPM�ʾ�������AV�Ρ��ɤ�
��ߤ��ʤ���250�ʾ�Ǥ����AV�Ρ��ɤβ�ߤ�����Ǥ��ʤ���
10-11 orthodromic tachycardia OARVT 280 BOM, QRS���϶�����P�Ȥ���ǧ�Ǥ��ʤ�
�Τ�PSVT�Ȥδ��̤Ϻ������˼���ꥨ��ȥ������
10-12 WPW�ο�˼��ư����������̮(irregularly irregular)��STD�������롥
10-13 �ַ�ŪWPW��
10-14 �ַ�ŪWPW��Type B
10-15 1��AV�֥��å������ɹ��ɡ��������ɡ�V1��STE��̵��Ǥ��ʤ���
V1��V5�ޤǤ�RR�������ɤ�̵��Ǥ��ʤ���
10-16 1��AV�֥��å���¦�ɵ��졥
10-17 0.48sec��1��AV�֥��å���sinus escape, CRBBB, ���ɹ��ɡ�
10-18 Wenckebach 2��֥��å���sinus escape, CRBBB, ���ɹ��ɡ�
10-19 Wenckebach 2��֥��å���
10-20 3��AV�֥��å����֥��å��ȷ���T���⤤�ȹ�K��ɡ�
10-21 3��AV�֥��å���junctional escape, RBBB��LAH���ڡ�����
10-22 3��AV�֥��å���ventricular escape, idioventricalr rhythm (������ͭĴΧ).
QRS��0.12sec, v1��V3��QS�ѥ�����V6�ϴ������ӥ֥��å��˸����롥
���ȥ��ԥڡ�����
�����������Q��
����P�Ȱʳ��ˡ��ͻ�����Q�Ȥ������롥���ɹ��ɤˤ���ȡ�ST���Ѳ����ʤ���
���Q�Ȥ����������ھɤǤ⤢�롥���ھɤǤ϶���ͶƳ�Ǥ⸫���롥
11-1 low voltage
11-2 low voltage
11-3 LBBB, AMI
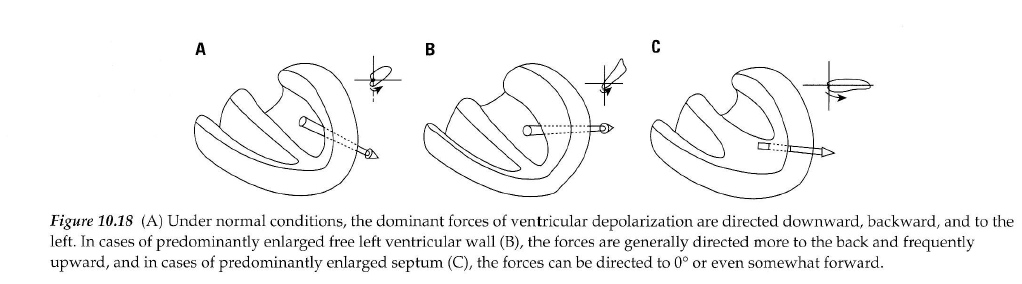 Luna��� A�����B�Ϻ�����ͳ�ɤ������C�Ϻ�����֡����������������p.138
Luna��� A�����B�Ϻ�����ͳ�ɤ������C�Ϻ�����֡����������������p.138
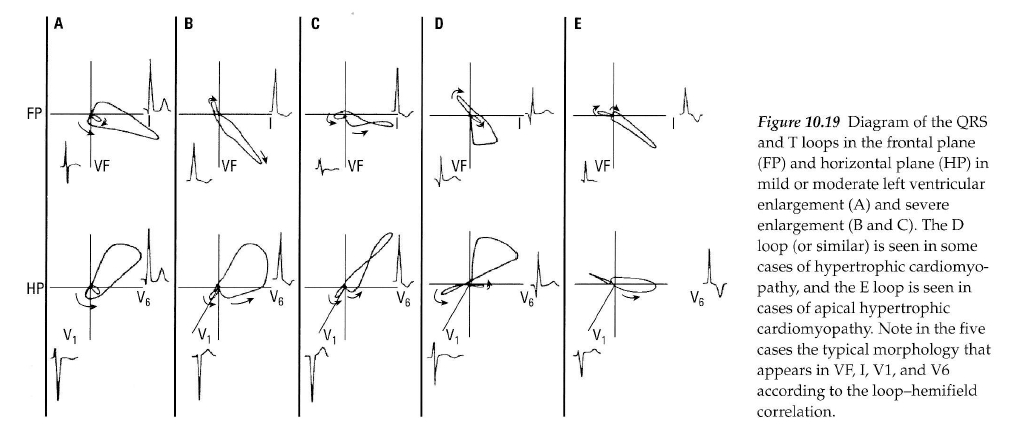 Luna��� ��������Υ٥��ȥ뿴�ſ� p.138
Luna LVH.pdf
V1�ޤ���V2��S�Ȥ�V5�ޤ���V6��R�Ȥ��¤���35mm�ʾ塥
�ɤ줫�ζ���ͶƳ����45mm�ʾ塥
aVL��R�Ȥ���11mm�ʾ塥
I��R�Ȥ���12mm�ʾ塥
aVF��R�Ȥ���20mm�ʾ塥
�嵭�Τɤ줫����������Ⱥ�������ޤ��Ϻ�����ĥ�Ǥ��롥
(PRD(PR�ֳ֤β��ߤ�0.8mm�ʲ��ʤ�����Ǥ��롥p.180)
11-4 ��������ˤ��LVH
11-5 ������ĥ�ˤ��LVH��I, II, III, aVF, V5, V6�Ǥ�
1mm�ʲ��ξ�����Q�ȤϺ�����ĥ����ħ��
������˱���ST�������Ȥ�T�Ȥϥ��ȥ쥤��(strain)�ȷ��Ǥ��롥
11-6 ŵ��Ū��LVH�ǤϤʤ���U��
11-7 �������Ű̡��ͻ�ͶƳ�Υե�åȤ�T�ȡ����ð�ŪST�Ѳ�
11-8 LVH, ���ȥ쥤��ѥ������žT�ȡ�
V1, V2��concave upward T�ȡ�V3�Ͼ����ST�����ǵ�žT�ȡ��褤��Ǥ��롥
11-9 LGL�ɸ�������̮��LVH������P�ȤǤϤʤ���
11-10 LVH, RAE, LAE, late intrinsicoid deflection, GE #298
I��R�Ȥ����˥��������������롥II�˦����ͤˤߤ��뤬WPW�ǤϤʤ���
11-11 RAE��LAE��LVH���ͻ�ͶƳ��flat��T�ȡ����ð�ŪST�Ѳ���
Luna��� ��������Υ٥��ȥ뿴�ſ� p.138
Luna LVH.pdf
V1�ޤ���V2��S�Ȥ�V5�ޤ���V6��R�Ȥ��¤���35mm�ʾ塥
�ɤ줫�ζ���ͶƳ����45mm�ʾ塥
aVL��R�Ȥ���11mm�ʾ塥
I��R�Ȥ���12mm�ʾ塥
aVF��R�Ȥ���20mm�ʾ塥
�嵭�Τɤ줫����������Ⱥ�������ޤ��Ϻ�����ĥ�Ǥ��롥
(PRD(PR�ֳ֤β��ߤ�0.8mm�ʲ��ʤ�����Ǥ��롥p.180)
11-4 ��������ˤ��LVH
11-5 ������ĥ�ˤ��LVH��I, II, III, aVF, V5, V6�Ǥ�
1mm�ʲ��ξ�����Q�ȤϺ�����ĥ����ħ��
������˱���ST�������Ȥ�T�Ȥϥ��ȥ쥤��(strain)�ȷ��Ǥ��롥
11-6 ŵ��Ū��LVH�ǤϤʤ���U��
11-7 �������Ű̡��ͻ�ͶƳ�Υե�åȤ�T�ȡ����ð�ŪST�Ѳ�
11-8 LVH, ���ȥ쥤��ѥ������žT�ȡ�
V1, V2��concave upward T�ȡ�V3�Ͼ����ST�����ǵ�žT�ȡ��褤��Ǥ��롥
11-9 LGL�ɸ�������̮��LVH������P�ȤǤϤʤ���
11-10 LVH, RAE, LAE, late intrinsicoid deflection, GE #298
I��R�Ȥ����˥��������������롥II�˦����ͤˤߤ��뤬WPW�ǤϤʤ���
11-11 RAE��LAE��LVH���ͻ�ͶƳ��flat��T�ȡ����ð�ŪST�Ѳ���
Luna RVH.pdf
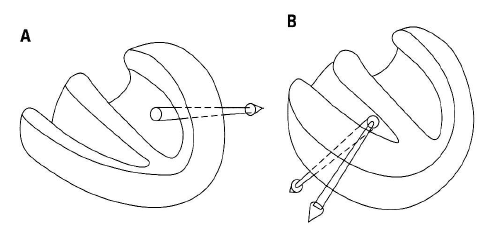 A�����B�ϱ������硥
��������ˤ��ŵ������������а̤ȸ屦���а̤���Ȥ��꤬���롥
�������ϱ��ӥ֥��å�����R'���礭����
��������V1��rS�ˤʤ롥��������������V6��S�Ȥ��礭����
S1S2S3�ϸ����������꼴�Ȥʤ롥
�Ǥ�����Ū���������Ƥ��롥
A�����B�ϱ������硥
��������ˤ��ŵ������������а̤ȸ屦���а̤���Ȥ��꤬���롥
�������ϱ��ӥ֥��å�����R'���礭����
��������V1��rS�ˤʤ롥��������������V6��S�Ȥ��礭����
S1S2S3�ϸ����������꼴�Ȥʤ롥
�Ǥ�����Ū���������Ƥ��롥
 �� �����Ѱ̤�V1���礭��R�Ȥ�RVH��ͤ��롥V1���ܼ�Ū��rSr'�Ǥ��롥
����2���ܤ�r'���礭���ʤ�ȱ��ӥ֥��å�����RVH�ˤʤ롥���ӥ֥��å���
���ϱ�����Ƴ�����ܿ��ڤ���Ƴ�ˤʤ뤿�ᡤ���������ޤ��������礭����
��������������ϥץ륭�����ݤ���Ƴ�Ǥ��뤫����Ƴ���֤�û��S�Ȥ�
���ⶹ���ޤ롥rSr'�κǽ��r����ֿ��ڤζ�ʳ��S�ȤϺ�����ʳ�Ǥ��ꡤ
�Ǹ��r'�ϱ������ڤζ�ʳ�Ǥ��ꡤ�̾��r'��������ɽ���ä�ɽ��ʤ���
�֥륬���ξ��ϱ���ή��ϩ�ο������礬���뤿�ᡤ�礭��r'�ȹͤ����
Ǽ����������
�� �̾��RBB��¸�ߤ����RVH�ο��ǤϤǤ��ʤ�����GE #121��RVH�ο��Ǥ���ǽ�Ǥ��롥
�� BB p.73�Ǥ�3�����RVH��ɽ������Ƥ��롥
���������3 type
Utah ECG Uwave
Right Ventricular Hypertrophy
General ECG features include:
* Right axis deviation (> 90 degrees)
* Tall R-waves in RV leads; deep S-waves in LV leads
* Slight increase in QRS duration
* ST-T changes directed opposite to QRS direction (i.e., wide QRS/T angle)
* May see incomplete RBBB pattern or qR pattern in V1
* Evidence of right atrial enlargement (RAE) (lessonVII)
Specific ECG features (assumes normal calibration of 1 mV = 10 mm):
* Any one or more of the following (if QRS duration < 0.12 sec):
o Right axis deviation (> 90 degrees) in presence of disease capable of causing RVH
o R in aVR �� 5 mm, or
o R in aVR > Q in aVR
* Any one of the following in lead V1:
o R/S ratio > 1 and negative T wave
o qR pattern
o R gt; 6 mm, or S < 2mm, or rSR' with R' > 10 mm
* Other chest lead criteria:
o R in V1 + S in V5 (or V6) 10 mm
o R/S ratio in V5 or V6 < 1
o R in V5 or V6 < 5 mm
o S in V5 or V6 > 7 mm
* ST segment depression and T wave inversion in right precordial leads is usually seen in severe RVH such as in pulmonary stenosis and pulmonary hypertension.
BB�Υ��饤�ƥꥢ p.73
* QRS���ŵ�����90��ʾ�����о��Ǥ��롥
a. qR ��V1
b. V1��R��7mm�ʾ塥
c. V1��R/S�椬1�ʾ塥
d. V1��ID��0.03sec�ʾ塥
e. V1��V6��QRS��rS�ȷ���
f. ��ͤ�S1S2S3�ȷ���
* ����P�ȡ�
* V1��V2��STD��ȿžT�ȡ�
9-14 LAE��IRBBB���ĵ���������ֹ��ɡ�RVH? �����а̡�II, III, aVF��T�ȵ�ž��
RVH��ɬ�ܡ�cf 11-12.
V1�϶���QR�ȷ���V2�Ͼ�����rS���̾��V1�Τ褦�˸����롥V1-V4�ϱ���
���ȥ쥤��T�ȡ������褦���Ǥ����ζ���S�Ȥϱ����������ħ��
11-12 ŵ��Ū��RVH��strain pattern��S1Q3T3�������롥RVH��V1��q�ȤϤʤ���RAE, LAE
11-13 ���귿ŪRVH��V2�� R/S ratio��1�ʾ塥
������ֹ��ɤ�ʻȯ���Ƥ��뤿���V1�ˤʤ�ʤ��������硥���̿��ǡ�
GE #121 II, aVF���ݤ����鼴��-30��ʲ���V1��PVC�Τ褦�˸����뤬�����rsR'
�Ǥ��롥V1-V3�ޤ�rsR'��ȿžT�ȡ�V4-V6��rS�Ȥ�����T�ȡ�
���ǡ�LAFB+CRBBB������RBBB�ϱ�������ο��ǤϽ���ʤ�����
V1�ΰ۾�ʹ⤵��R'��V6��S�ȡ�������ȿžT�Ȥ�RVH�碌�롥
�̾��CRBBB�Ǥ�V6��R�Ȥ�������S�ȤǤ��뤬��RVH�Ǥ�R�Ȥ���������
S�ȤϱԤ�������LAFB����ʻ�����V6��S�ȤϤ���˿����ʤ롥
GE #196 ��90�ʾ塤����P�ȡ�V1��rsR'�Ǥ��뤬��rs�����˾�������R'�ϥ��㡼�פ�
�̾�α��ӥ֥��å��Ȱۤʤ롥V2��V6�ޤǤ϶������ζ���S�ȡ����ӥ֥��å�
�Ǥ����S�������������顤���������鸫�Ƥ�RBBB�Ȥϰۤʤ롥V1��
����T�Ȥǡ�V2��ʿó��V3-V6���̾��T�ȡ�R�Ȥ�V3���Ǥ�⤯��
V6�˹Ԥ��ˤ������ä��ȹ�Ͼ������ʤ롥����P�Ȥȱ������硥
11-14 ventricular escape beat��35 BPM��IVCD,
T�Ȥ�QRS��2�����Ǥ��äƤ��ž���롥��K��� 8.7 mEq/L��
final�Ǥ�Af��ȼ����Ƴ��1ͶƳ����ɽ������Ƥ��ʤ���final p.169
11-15 qR'��RBBB
11-16 VT, ��K��� 9.4mEq/L
11-17 ����P�ȡ�3��AV�֥��å���CLBBB��CRBBB������QRS
2�����P�ȡ�PAC�θ���Ѳ����Ƥ��롥
11-18 VTach (VT)��LAH���а�����V1��V2�δ֡�
11-19 ����q�ȤȰ۾�Q�ȡ��ͻ�ͶƳ
11-20 ����q�ȤȰ۾�Q�ȡ�����ͶƳ
11-21 IIIͶƳS�ȤθƵ۰�ư���ܹ��Ӥ�V1��V2��V1�ο�������������NSSTC��PR���㲼
���ǤϽ줺��
�� �����Ѱ̤�V1���礭��R�Ȥ�RVH��ͤ��롥V1���ܼ�Ū��rSr'�Ǥ��롥
����2���ܤ�r'���礭���ʤ�ȱ��ӥ֥��å�����RVH�ˤʤ롥���ӥ֥��å���
���ϱ�����Ƴ�����ܿ��ڤ���Ƴ�ˤʤ뤿�ᡤ���������ޤ��������礭����
��������������ϥץ륭�����ݤ���Ƴ�Ǥ��뤫����Ƴ���֤�û��S�Ȥ�
���ⶹ���ޤ롥rSr'�κǽ��r����ֿ��ڤζ�ʳ��S�ȤϺ�����ʳ�Ǥ��ꡤ
�Ǹ��r'�ϱ������ڤζ�ʳ�Ǥ��ꡤ�̾��r'��������ɽ���ä�ɽ��ʤ���
�֥륬���ξ��ϱ���ή��ϩ�ο������礬���뤿�ᡤ�礭��r'�ȹͤ����
Ǽ����������
�� �̾��RBB��¸�ߤ����RVH�ο��ǤϤǤ��ʤ�����GE #121��RVH�ο��Ǥ���ǽ�Ǥ��롥
�� BB p.73�Ǥ�3�����RVH��ɽ������Ƥ��롥
���������3 type
Utah ECG Uwave
Right Ventricular Hypertrophy
General ECG features include:
* Right axis deviation (> 90 degrees)
* Tall R-waves in RV leads; deep S-waves in LV leads
* Slight increase in QRS duration
* ST-T changes directed opposite to QRS direction (i.e., wide QRS/T angle)
* May see incomplete RBBB pattern or qR pattern in V1
* Evidence of right atrial enlargement (RAE) (lessonVII)
Specific ECG features (assumes normal calibration of 1 mV = 10 mm):
* Any one or more of the following (if QRS duration < 0.12 sec):
o Right axis deviation (> 90 degrees) in presence of disease capable of causing RVH
o R in aVR �� 5 mm, or
o R in aVR > Q in aVR
* Any one of the following in lead V1:
o R/S ratio > 1 and negative T wave
o qR pattern
o R gt; 6 mm, or S < 2mm, or rSR' with R' > 10 mm
* Other chest lead criteria:
o R in V1 + S in V5 (or V6) 10 mm
o R/S ratio in V5 or V6 < 1
o R in V5 or V6 < 5 mm
o S in V5 or V6 > 7 mm
* ST segment depression and T wave inversion in right precordial leads is usually seen in severe RVH such as in pulmonary stenosis and pulmonary hypertension.
BB�Υ��饤�ƥꥢ p.73
* QRS���ŵ�����90��ʾ�����о��Ǥ��롥
a. qR ��V1
b. V1��R��7mm�ʾ塥
c. V1��R/S�椬1�ʾ塥
d. V1��ID��0.03sec�ʾ塥
e. V1��V6��QRS��rS�ȷ���
f. ��ͤ�S1S2S3�ȷ���
* ����P�ȡ�
* V1��V2��STD��ȿžT�ȡ�
9-14 LAE��IRBBB���ĵ���������ֹ��ɡ�RVH? �����а̡�II, III, aVF��T�ȵ�ž��
RVH��ɬ�ܡ�cf 11-12.
V1�϶���QR�ȷ���V2�Ͼ�����rS���̾��V1�Τ褦�˸����롥V1-V4�ϱ���
���ȥ쥤��T�ȡ������褦���Ǥ����ζ���S�Ȥϱ����������ħ��
11-12 ŵ��Ū��RVH��strain pattern��S1Q3T3�������롥RVH��V1��q�ȤϤʤ���RAE, LAE
11-13 ���귿ŪRVH��V2�� R/S ratio��1�ʾ塥
������ֹ��ɤ�ʻȯ���Ƥ��뤿���V1�ˤʤ�ʤ��������硥���̿��ǡ�
GE #121 II, aVF���ݤ����鼴��-30��ʲ���V1��PVC�Τ褦�˸����뤬�����rsR'
�Ǥ��롥V1-V3�ޤ�rsR'��ȿžT�ȡ�V4-V6��rS�Ȥ�����T�ȡ�
���ǡ�LAFB+CRBBB������RBBB�ϱ�������ο��ǤϽ���ʤ�����
V1�ΰ۾�ʹ⤵��R'��V6��S�ȡ�������ȿžT�Ȥ�RVH�碌�롥
�̾��CRBBB�Ǥ�V6��R�Ȥ�������S�ȤǤ��뤬��RVH�Ǥ�R�Ȥ���������
S�ȤϱԤ�������LAFB����ʻ�����V6��S�ȤϤ���˿����ʤ롥
GE #196 ��90�ʾ塤����P�ȡ�V1��rsR'�Ǥ��뤬��rs�����˾�������R'�ϥ��㡼�פ�
�̾�α��ӥ֥��å��Ȱۤʤ롥V2��V6�ޤǤ϶������ζ���S�ȡ����ӥ֥��å�
�Ǥ����S�������������顤���������鸫�Ƥ�RBBB�Ȥϰۤʤ롥V1��
����T�Ȥǡ�V2��ʿó��V3-V6���̾��T�ȡ�R�Ȥ�V3���Ǥ�⤯��
V6�˹Ԥ��ˤ������ä��ȹ�Ͼ������ʤ롥����P�Ȥȱ������硥
11-14 ventricular escape beat��35 BPM��IVCD,
T�Ȥ�QRS��2�����Ǥ��äƤ��ž���롥��K��� 8.7 mEq/L��
final�Ǥ�Af��ȼ����Ƴ��1ͶƳ����ɽ������Ƥ��ʤ���final p.169
11-15 qR'��RBBB
11-16 VT, ��K��� 9.4mEq/L
11-17 ����P�ȡ�3��AV�֥��å���CLBBB��CRBBB������QRS
2�����P�ȡ�PAC�θ���Ѳ����Ƥ��롥
11-18 VTach (VT)��LAH���а�����V1��V2�δ֡�
11-19 ����q�ȤȰ۾�Q�ȡ��ͻ�ͶƳ
11-20 ����q�ȤȰ۾�Q�ȡ�����ͶƳ
11-21 IIIͶƳS�ȤθƵ۰�ư���ܹ��Ӥ�V1��V2��V1�ο�������������NSSTC��PR���㲼
���ǤϽ줺��
11-22 II, III, aVF��Q�Ȥ�������V4��V6��Q�ȡ�V1��R�Ȥ��⤯����������
���ɡ�¦�ɤι��ɤ�Ϣ³��������ɤι��ɤ��ͤ����롥transition��V1��V2��
I��q�ȤϾ����礭���۾aVL��q�Ȥ�۾�ǹ��¦�ɹ��ɡ�
V1��R�Ȥ��⤯���������Τϡ����ɹ��ɤ����ä����Ȥ���
V1,V2��J�����㲼���Ƥ��ʤ����Ȥϡ����ɤ�ST�徺���ʤ����Ȥ���
���ɹ��ɤΰ۾�Q�Ȥ�III>aVF>II�ν�˾������ʤ뤬�����¦�ɹ��ɤ�
ȯ�������I�ǰ۾�Q�Ȥ������뤿��III�Ǥΰ������ⲽ���ä���롥
aVL��Q�Ȥθ����aVL=(i-III)/2������I��Q�Ȥ���III��Q�Ȥ���������
����˾�����Q�Ȥˤʤ롥
11-23 II, III, aVF�ϰ۾�Q�ȡ�V1��QS�Ȥ����V2S+V5R>35mm������LVH��
11-24 II, III, aVF�ΰ۾�Q�Ȥ�ST�徺ȿžT�ȡ�
LAE��V4��V6��T�ȵ�ž��TR��V2�����ɹ��ɤ�RVH��
���ο��ſޤˤ���ޤ롥����ECG�����Ǥ�Ƚ�ǤǤ��ʤ���
11-25 �ͻ�ͶƳ���Ű̡��ŵ�����ʿ��V1QS�˶���Ű̡�V2��V4��STȿž�����
TR��V5��V6��LAE���㴳PRD��effusion��
11-26 QT��Ĺ��1��AV�֥��å����ͻ����Ű̡�TR��V5����V6��V1��QS�ȤǤϤʤ�r�Ȥ����롥
II, V2��V5�ޤǤθ�����PRD�����뤫��pericarditis��
�ͻ����Ṳ̋ˤ�PRD�����դ��뤳�ȡ�
11-27 I, aVL���Ű̹���LVH��ƶ������̮���ŵ����Ͽ�ʿ��TR��V1��V2��ȿ���ײ�ž��
RVH�ˤʤ뤬�����������а̤Ǥʤ���ξ����ĥ�Ȳ������Ƥ��롥
�����ST��ȿž����ĥ��ST�����
11-28 RAE��TR��V1��V2�δ֡�T��ȿž���������礫���ɹ��ɤ���
���ɹ��ɤʤ�II, III, aVF���Ѳ���ɬ�ס�
R�Ȥν�λ���Τ��֡�
���β���ȯ�����롥���Τ���˽�̮��¿����p.230
�ɲ������ˤ��Ӥ줿�Υå����٤��ȯ������������¦���ڤ�
æʬ�ˤ�³��������¦���ڤ�æʬ�ˤǤ��롥
ξ�Ԥ�æʬ�ˤ��������ȥ��顼���˴ݤ��ʤ롥
ST�������ȤϿ�ʿ��J�����㲼��ȼ���㲼��J���ξ徺��ȼ���徺
�ʤɤ������
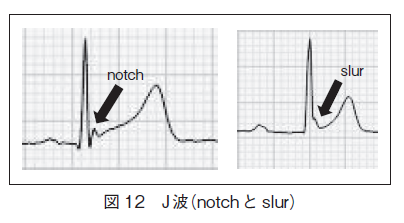
11-28 Notch��J wave���⤤���оΤ�T�ȡ�
11-31 Osborn
11-32 Osborn
11-33 Osborn
13-1 RBB��ŵ���㡤VͶƳ��R:S ratio��ɬ���礭���ʤ롥qR'�Ǥ��äơ�qR�ȤϽʤ���
13-2 rsr'r''����RBBB��LAH��ȼ��2�ޥ֥��å���
13-3 rsr'r''����RBBB��inferolateral ischemia��
WAT: wandering atrial pacemeker
iregurary iregular ��������̮
MAT: fultifocal atrial tachycardia
iregurary iregular ��������̮
TESTECG 21
�������ӥ֥��å��Ǥ��뤬���ɹ��ɤν긫���ʤ���
BB
20, 42, 47, 112, 112, 117, 119-121, 125, 127, 129, 131, 133
135-139, 355, 370-372, 175, 376, 432
IVCD����ħ��
12 lead �ˤ���(p.289) ��IVCD�϶ɽ�ŪIVCD�����ʤ��1ͶƳ��
�ä�III�Ǹ�����QRS�� 0.12sec�ʲ��ΥΥå��Τ����ȷ�(localized IVCD)�ȡ�
��ͶƳ�Ǥߤ���0.12sec�ʾ��QRS�����ȷ��Ǥ��ꡤ
�ä�LBBB��RBBB����ħ��⤿�ʤ��ȷ�(Generarized IVCD)�˶��̤���롥
����IVCD��V1�Ǻ��ӥ֥��å�����V6�DZ��ӥ֥��å�������
V1��rS�Ǻ��ӥ֥��å��ͤǤ��뤬�����θ�RS�ѥ������V6�Ǥ�R�Ȥ��������ɤ�
�ޤޤǤ��ꡤ�Ѳ���˳������QRS����3mm�Ǵ������ӥ֥��å��ȶ��̤�����
���������������ӥ֥��å����ȱ�������˶�ʳ���뤿��V6��S�ȤϤʤ���
IVCD��������QTc >0.5sec���ʤ���� > 0.44sec (��)��> 0.46sec (��)
IVCD�Υ��ߥ�졼�����
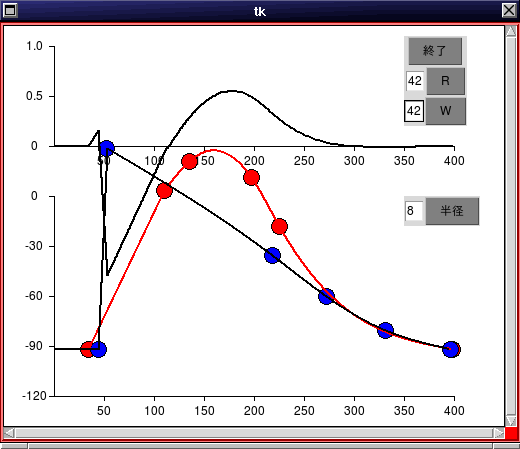
IIͶƳ�䡤V6�Υ��ߥ�졼��������
2018ǯ 10�� 29�� ������ 23:27:15 JST
8mEq/L�ʾ�ι�K��ɤ�IVCD�ˤʤ롤������¦Perkinje��Ƴ®�٤���ü��
�㲼�������Ϥΰ��̿��ڤ���Ƴ®���㲼�Ͼ��ʤ������η�̡�r�Ȥθ��
������¦����˶�ʳ�����礭��S�Ȥ������롥���θ塤������¦�ζ�ʳ�ˤ��
S�Ȥξ����ʬ�������롥S�Ȥβ������Ͼ��������٤����Ū�ԤǤ��롥
����Ͽ�����¦���ڤ���Ƴ®�٤��ᤤ���Ȥ��Ƥ��롥
GE #239 IVCD�Ǥ��롥
GE #305 PQû�̡�
���ǡ�WPW��V4-6��S�Ȥ�����Ǥ��ꡤIVCD������Ǥ��롥
GE #32��I�Ǥ�R�Ȥ�Ω��꤬�٤���V1�Ǥϲ��ߤ��ϤޤäƤ���r�ȤΥΥå��������롥
���Ӥβ��߶�ʳ���٤�Ƥ��鱦�Ӥ˶�ʳ������롥IVCD�Ȥ������ILBBB�ȿ��Ǥ��٤���
GE #243��QRS����0.16�ä�IVCD��V1-2��S�Ȥ�Ω���ǥΥå��������롥
V1��r�Ȥ����STE�����顤�������ɹ��ɤǤ��롥LAFB�Ǥ��롥
����-60������LAFB��LAFB��R�Ȥ��������ɤ�V6�Ǥ�S�Ȥ�ȼ����
aVL��q�Ȥ�septal q�����麸�ӥ֥��å��ǤϤʤ���
���ޤ�GE #243
 GE #248��QRS����0.10��IVCD�����ײ�ž�Ǥ��뤬��S�Ȥ�Ω���ǥΥå������롥
GE #305�ϰ츫IVCD�˸����뤬WPW�Ǥ��롥
intraventricular conduction defect p.94 ecg 9-5
�̾��QRS�δ֤˥���������ȯ���������ࡼ���ʶ�ʳ��Ƴ���Ǥ��ʤ����֡�
ecg 9-5��IVCDdelay�Ǥ⤢�롥V1�Ϻ��ӥ֥��å�����V6�Ͽ������������Ƥ�RS���Ǥ��롥
�ޤ�V1�ޤ���V2��S�Ȥ��Ǥ��礭��R�Ȥ��������ɤΤޤ�V6������Τⶦ�̤��Ƥ��롥
intraventricular conduction delay (IVCD) 12 LEAD ECG p.289
QRS����0.12sec�ʾ塤V1��LBBB�ͤ�V6��RBBB�ͤ��ȷ����������롥
��K��ɤ�����Ū�ȷ���
141f ecg 10-7, WPW Type A����Ǥ��뤬��III��aVF��P�Ȥ���������
ʣ����QRS�ȷ��Ǥ��롥�����IVCD�ȿ��Ǥ��롥(�ü����)
p.336 ecg 14-8�ϥƥ�Ⱦ�T�ȡ�IVCD��V5, V6��RS�ȷ��ˤʤ�ʤ�����IVCD�ȿ��ǡ�
198f ecg 11-14, ��K��ɤˤ��IVCD��QRS��������������̮��������ͭĴΧ��
V1�Ϻ��ӥ֥��å��η��Ǥ��뤬��V4�ޤ��Ѳ������ʤ���V6��RS�ȷ��ΤޤޤǤ��롥
QRS����6mm (ŵ��Ū����)
12 lead ECG pp. 289-293
13-21 PR 0.2sec, 77 bpm, IVCD
13-22 P�Ȥʤ���48 bpm, QRS 0.24sec IVCD��QT�ֳ֤ϱ�Ĺ�����Ż߾��֤����롥
p.336 14-18�ϥƥ�Ⱦ�T�ȡ�IVCD��V5, V6��RS�ȷ��ˤʤ餺���ȷ������Ƥ��롥
13-23 �����ڡ����ˤ�뿴���ȷ���IVCD�ͥѥ�����
14-57 IVCD, QRS 0.18, ����Ū��I��V6�ϻ����ȷ��Ǥ��뤬��V6��RS�ѥ�����QRS��0.12sec�ʲ�����LAFB�ˤʤ롥T�ȤˤĤ��ƤϺǸ��S�Ȥ���˹ͤ����Ʊ��(concordant)�ˤʤ뤬�֥��å�������۾�Ǥ��롥
GE #248��QRS����0.10��IVCD�����ײ�ž�Ǥ��뤬��S�Ȥ�Ω���ǥΥå������롥
GE #305�ϰ츫IVCD�˸����뤬WPW�Ǥ��롥
intraventricular conduction defect p.94 ecg 9-5
�̾��QRS�δ֤˥���������ȯ���������ࡼ���ʶ�ʳ��Ƴ���Ǥ��ʤ����֡�
ecg 9-5��IVCDdelay�Ǥ⤢�롥V1�Ϻ��ӥ֥��å�����V6�Ͽ������������Ƥ�RS���Ǥ��롥
�ޤ�V1�ޤ���V2��S�Ȥ��Ǥ��礭��R�Ȥ��������ɤΤޤ�V6������Τⶦ�̤��Ƥ��롥
intraventricular conduction delay (IVCD) 12 LEAD ECG p.289
QRS����0.12sec�ʾ塤V1��LBBB�ͤ�V6��RBBB�ͤ��ȷ����������롥
��K��ɤ�����Ū�ȷ���
141f ecg 10-7, WPW Type A����Ǥ��뤬��III��aVF��P�Ȥ���������
ʣ����QRS�ȷ��Ǥ��롥�����IVCD�ȿ��Ǥ��롥(�ü����)
p.336 ecg 14-8�ϥƥ�Ⱦ�T�ȡ�IVCD��V5, V6��RS�ȷ��ˤʤ�ʤ�����IVCD�ȿ��ǡ�
198f ecg 11-14, ��K��ɤˤ��IVCD��QRS��������������̮��������ͭĴΧ��
V1�Ϻ��ӥ֥��å��η��Ǥ��뤬��V4�ޤ��Ѳ������ʤ���V6��RS�ȷ��ΤޤޤǤ��롥
QRS����6mm (ŵ��Ū����)
12 lead ECG pp. 289-293
13-21 PR 0.2sec, 77 bpm, IVCD
13-22 P�Ȥʤ���48 bpm, QRS 0.24sec IVCD��QT�ֳ֤ϱ�Ĺ�����Ż߾��֤����롥
p.336 14-18�ϥƥ�Ⱦ�T�ȡ�IVCD��V5, V6��RS�ȷ��ˤʤ餺���ȷ������Ƥ��롥
13-23 �����ڡ����ˤ�뿴���ȷ���IVCD�ͥѥ�����
14-57 IVCD, QRS 0.18, ����Ū��I��V6�ϻ����ȷ��Ǥ��뤬��V6��RS�ѥ�����QRS��0.12sec�ʲ�����LAFB�ˤʤ롥T�ȤˤĤ��ƤϺǸ��S�Ȥ���˹ͤ����Ʊ��(concordant)�ˤʤ뤬�֥��å�������۾�Ǥ��롥
STC.pdf
��˼���硤left atrial enlargement,
��˼�ζ�ʳ�θ塤��˼��ʳ�������ˤߤ��뤫����������P�Ȥˤʤ롥
�������������0.12�ðʾ塤ξĺ���δֳ֤�0.04�ðʾ塥
P�Ȥλ���hump�ȸ�����two humps, a double hump ��ɽ�����롥(hump�Ȥ�ǭ�ؤΰ�̣)
0.12�ðʲ��ǥΥå��Τ���P�Ȥ�LAE�ȤϿ��Ǥ��ˤ�����
12 Lead ECG��p. 93.
ECG 9-5 V1��S�Ȥ�35mm�ʾ塤V6��R�Ȥ���������LVH�ȿ��ǤǤ��롥
ECG 9-6 AVL��R�Ȥ�11mm �ʾ塤LAH, LVH
ECG 9-7 LAE��long QT, V4-6��ST�������Ȥ�Ĺ�����߾��Ǥ��롥2��α�Ĺ�ϳΤ���
��������T�Ȥβ��������ԤȤϸ����ʤ���
LAH Left Anterior Hemiblock �������ޥ֥��å�
II < 0 �ʤ� axix < -30��
II,III,aVF�Τɤ줫�˾�����r�Ȥ�ɬ�ס�
�ޤ���I��qR�⤷����R�ȡ�III��rS�Ȥ�ɬ�ס�
II,III,aVF��r�Ȥ�̵�����٤�Q�Ȥʤ鲼�ɹ��ɤǤ��롥
����ͶƳ�Ϥ��٤ƥ��顼�Ǥʤ�S�Ȥ��и����롥
����ϱ����ǤϤʤ�������¦�ɤζ�ʳ�ٱ���̣���롥
13-24 LAH, Axis <-30�롤I��qR��III��rS�������롥TR��V4����V6��RS�ѥ�����
13-25 LAH, Axis <-30�롤I��qR��III��rS�������롥TR��V5����V1����V6��RS�ѥ�����
13-26 LAH, Axis <-30�롤III��rS�������롥�ͻ�ͶƳ���Ű̡��Ƶ�����ư
13-27 LPH��RAE, LAE, II,III,aVF��ST������žT�ȡ�S1Q3T3���ٹ��ɤȤδ��̤�
����ɬ�ס��᤺�餷����
13-28 Tachycardia��LPH����K��ɡ�QT�ϱ�Ĺ���Ƥ��뤬�ͻ�ͶƳ�Ǥο�ʿST���ʤ���
13-29 �������ײ�ž�Ǥ��뤬��¦�ɹ��ɤξڵʤ���S1Q3T3�Ǥ��뤬
��̮����˼��١�V1�ʤɤDZ�����٤� ħ�����ʤ�����̤Ȥ���LPH�ˤʤ롥
13-30 S1Q3T3, RAE, qR'�ǤϤʤ�qR�DZ������硥������ȿ���ײ�ž��RVH�Ǥ��롥
ȿ���ײ�ž��V1��RS���ˤʤ뤫�鱦������ξ��ˤʤ롥����P�ȡ�S1Q3T3��
�ٹ��ɤ�ħ����Axis��90��ʾ��LPH�����˱��������ͤ��롥
LPH�Ϥޤ�Ǥ��롥
V1��q�Ȥ�����r�Ȥξ��Ǥ��뤬������¦����֤�����ƺ�����
��ʳ��Ƴ�����ȹͤ��롥�ޤ�V1R��ĺ����V3R��ĺ���λ��꤬���פ���
���Ȥ��鱦�����ɶ�ʳ��������ʳ�˾��ä��ȹͤ��롥
13-31 III��q�Ȥ�ST�徺�����ܤ��롥LPH�ǤϤʤ���IWMI�Ǥ��롥
13-32 RBBB��LAH��NSR��1��֥��å���LVH
13-33 RBBB��LAH��NSR��1��֥��å���LVH
13-34 RBBB��LAH��P�ȤϤʤ�����������̮��
13-35 RBBB��LAH��NSR��LVH
13-36 RBBB��LAH��NSR��LVH
LPH Left Posterior Hemiblock ���Ӹ�ޥ֥��å�
13-37 RBBB��LPH��NSR��RAE��LAE�������Ŷ����ɡ�
13-38 RBBB��LPH��I��rS��III��qR(qS)�������ŵ�����90��ʾ塥
13-39 RBBB��LPH��I��rS��III��qR(qS)�������ŵ�����90��ʾ塥
504f-509f,
522f ecg 16-21 ���Ĺ������ˤ��IVCD��1��AV�֥��å���
V1��rS�Ǻ��ӥ֥��å��ͤǤ��뤬�����θ�RS�ѥ������V6�Ǥ�R�Ȥ��������ɤ�
�ޤޤǤ��ꡤ�Ѳ���˳������QRS����3mm�Ǵ������ӥ֥��å��ȶ��̤�����
���������������ӥ֥��å����ȱ�������˶�ʳ���뤿��V6��S�ȤϤʤ���
621, 626, 627, 657
13 B QTc¬��Ȥ��ΰ�̣
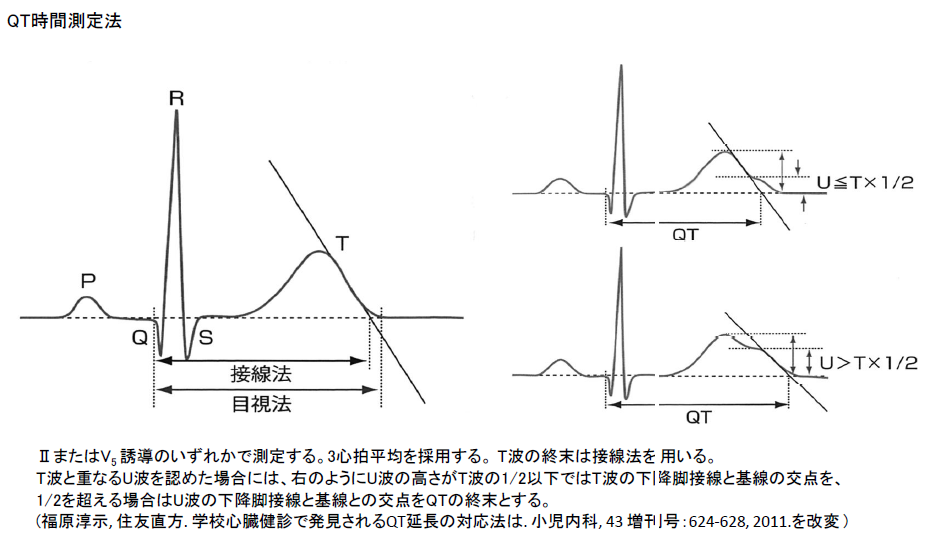
��QT���֤ȤϿ��ſޤ�q�ȤλϤޤ꤫��T�Ȥν�λ���ޤǤλ��֤Ǥ��ꡤ�����ڤμ��̻���(APD)��ɽ�������ڼ����Ϥ�������п����˽���������դ�û���֤Ƕ�ФǤ���QT���֤�û���ʤ롥�դ˼����Ϥ��夯�ʤ�ȶ�л��֤�Ĺ���ʤ�QT���֤ϱ�Ĺ���롥�ޤ�������ˤ�ƶ�����������лɷ�ǿ������¿���ʤ�ȡ����ڼ����Ϥ����ä��뤿��� QT���֤�û���ʤ롥 QT���֤���35-A�˼�����ˡ��¬�ꤵ��롥U�ȤˤĤ��Ƥ�̮�郎�٤��Ȥ��ˤ褯�и����뤬���㥫�ꥦ���ɤǤ�ɬ�ܤν긫�Ǥ��롥 T�Ȥ��ȹ��1/2����礭������ U�Ȥν�λ���ޤǤ�ޤ�뤬������ʲ��������Ω����U�Ȥξ���T�Ȥν�λ���Ƿ�¬���롥�������ä���Ω����U�Ȥ�QT���֤˴ޤ�ʤ����Ȥˤʤ롥
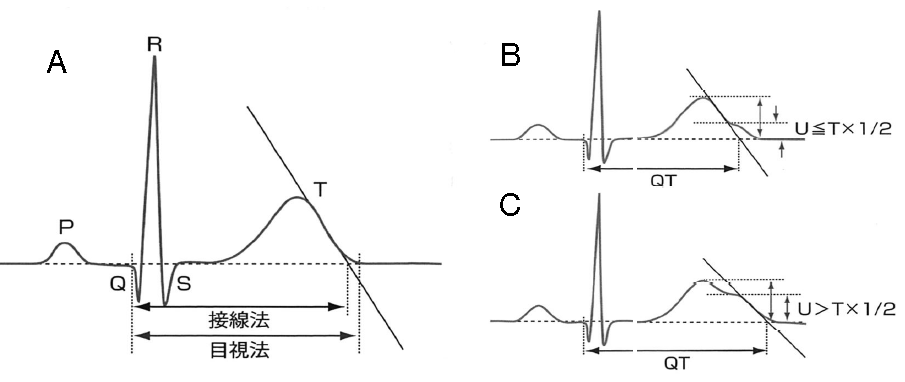
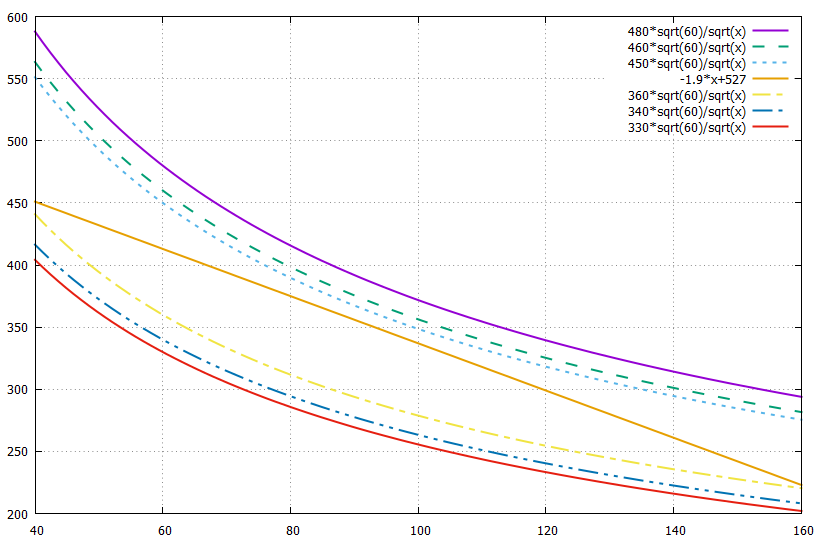
������ſް��Ż��Ǥ�QT���֤ȿ�����Ȥδط����¬�������35-B�Τ褦�˿�������Ф���ľ��Ū�˸������롤�����ǿ�����αƶ�������������ʤ����륤��ǥå����������ˡ�Ȥ���Bazett��RR�ֳ֤������ưʲ��˼�����������ͰƤ���QTc�Ȥ�֤��Ȥˤ�����
 QT (msec), RR (sec)
QT (msec), RR (sec)
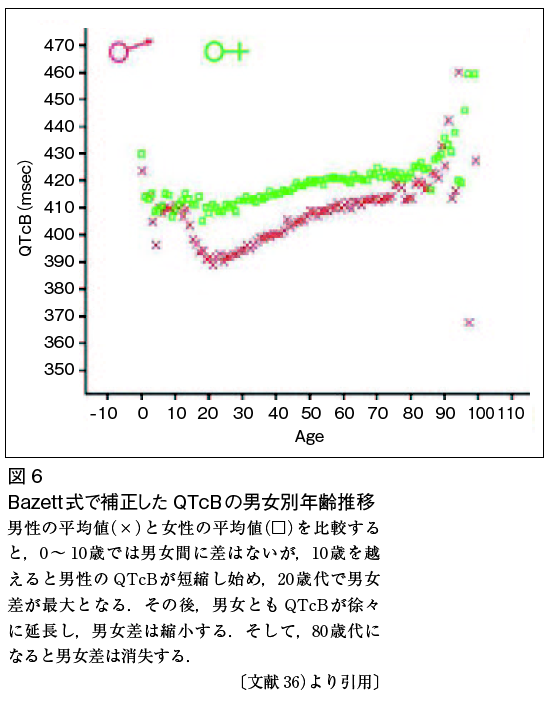
������QT��msec��RR�ֳ֤��äȤ��롥���μ�����ʬ����褦�˿������ 60�ʲ��Ǥ����ʬ�줬1�ʾ�ˤʤꡤQTc�Ͼ������ͤˤʤꡤ��������礭���ʤ���礭���ͤ���������롥���������ˤ��QTc��ǯ��δط�����35-C�˼����������Ȥ��Ƥϡ�QTc��10�ͤޤǤ��˽��κ��Ϥʤ���������10�ͤ�ۤ���Ƚ������Ѳ������ʤ�����������QTc�ϵ�˲��ߤ���25�����٤ǺǾ��ˤʤ롥���θ塤ξ�Ԥ�ǯ��ȶ��˴˽������ä���80�ͤ�ۤ���ȵ�����ä��롥 ʿ�ѤȤ�������������400 msec��������414 msec�ǡ��ˤ��������ڼ����Ϥ����20�ͤ��Ǥ��϶�����ξ�Զ���80�ͤ���ȵ�˿ꤨ�뤳�Ȥ��Ƥ��롥���ܽ۴Ĵ�ز���Ǵ��ˤ��ȡ�QTc�� 480msec�ʾ夬3����460��479 msec��2����450��459 msec��1���β������դ��Ƥ��롥��35-D��QT-�����ɸ�ˤ�����QTc�δط�����ɽ35-E��QT��Ĺ�ɸ����ο��Ǵ����������QTc�ȤϿ������Ϥ�ɾ����ɸ�Ǥ���ȶ��ˡ�QRS�����Ѳ������ʤ����Ȥ��T�Ȥ����α�Ĺ���Ǥ��礭�ʰ��ҤȤʤ롤��ü�ʹ⥫�ꥦ���ɤ�ȯ������IVCD�Ǥ�QTc�϶��٤˱�Ĺ����R on T��³��VT��ȯ���������λ��Ȥ��ƹͤ����롥
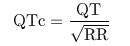
��35-A QT���֤�¬��ˡ
QT���֤�¬���q�ȤλϤޤ꤫��T�Ȥν�λ�������ܻؤǷ��ꤹ���ꡤT�Ȥβ����������������֤Τ������Ǥ���(A)��U�Ȥ�����ſФ�̮�郎�٤��ʤ��ȯ�����뤬���㥫�ꥦ���ɤǤ�ɬ��T�Ȥ�³���ƽи����롥���ξ�硤B�˼����褦��T�Ȥ��ȹ��1/2�ʲ��Ǥ����ͭ�Ϥ�̵��(B)��1/2�ʾ�Ǥ����U�Ȥβ������������ǽ���������(C)��
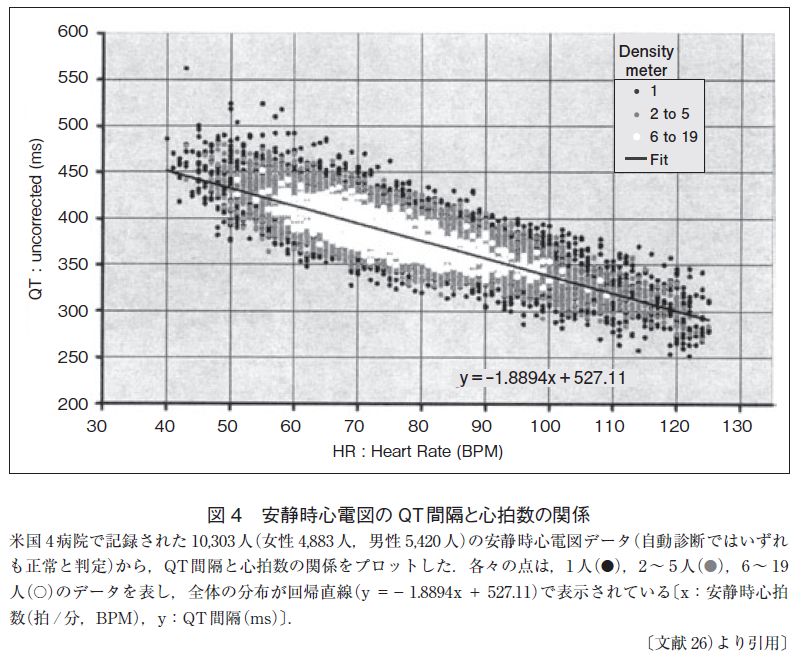
��35-B ���Ż����ſޤ�QT���֤ȿ�����δط�
�ƹ�4�±��Ǥ�(����4883�͡�����5420��)�μ�ư��¬������ȿ��Ǥ��줿�ǡ�����ľ����y=-19+527������줿����ݤ��Ǥ����٤��⤯��ľ���˽��椷�Ƥ��롥
(ʸ����LuoS, et. al. A comparion of commonly used QT correction formula
: The effect of heart rate on the QTc of normal ECGs. J Electorcaridol.
2004:37(Suppl):81-90)
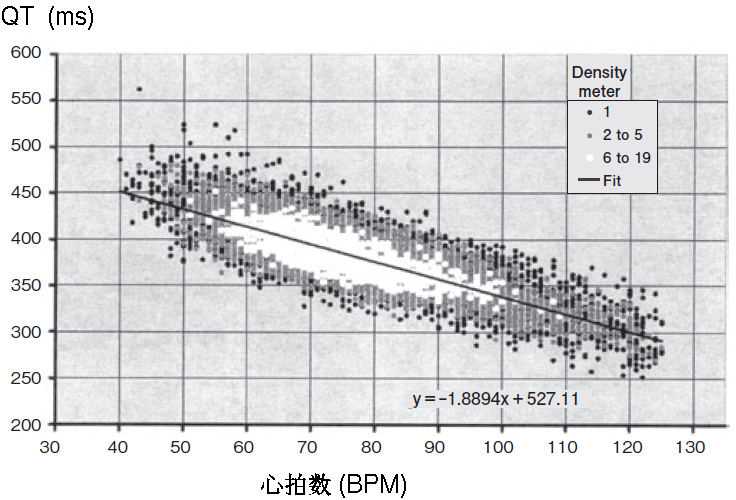
��35-C Bazett������������QTc���˽���ǯ����
�֥ޡ��������������ޡ����Ͻ�����
(ʸ����������ͺ QT�ֳ֤ˤ�뿴��ǽɽ����ͽ���ͽ¬��
���ܿ��ſز�� 2013, 33:223-246 ����������)
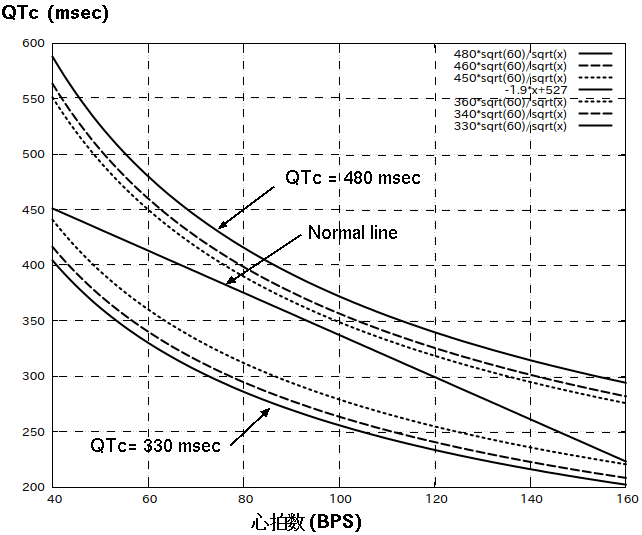
��35-D QT-�����ɸ�ˤ�����QTc�δط�
ʿ��Qt����ľ����Normal line�Ȥ���QTc�α�Ĺ�ͤ������Ǽ�����������QTc��480 msec�ǿ��Ǵ��ˤ��ȥ���ݥ�3�ˤ����롥Normal line�β����˼���������SQT�ο��Ǵ����������롥
ɽ35-E QT��Ĺ�ɸ����ο��Ǵ��
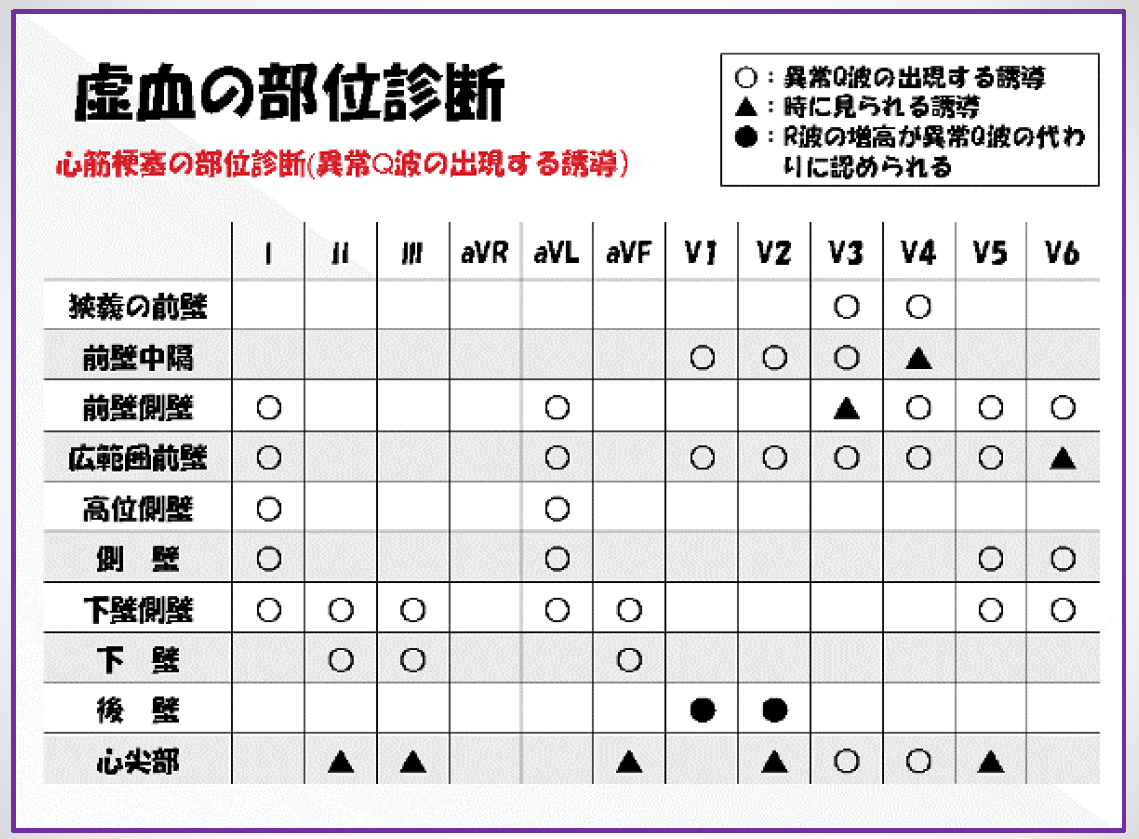
QT��Ĺ�ɸ�����Brugada�ɸ����ο��Ť˴ؤ��륬���ɥ饤��(2012)��ꡥ
QTc�ˤ�뿴��ǽɽ����ͽ���ͽ¬"
 QTc���
Bazett: QTcB=QT/(RR)1/2
Friderica:QTcF=QT/(RR)1/3
Hodges: QTcH=QT+105(1/RR-1)
Bazett��Friderica��Hodges���������Ǥ�RR��ñ�̤�sec����Ѥ��롥
Framingham: QTcFr=QT+0.154(1000-RR)
RR��ñ�̤�msec����Ѥ��롥
QTc���
Bazett: QTcB=QT/(RR)1/2
Friderica:QTcF=QT/(RR)1/3
Hodges: QTcH=QT+105(1/RR-1)
Bazett��Friderica��Hodges���������Ǥ�RR��ñ�̤�sec����Ѥ��롥
Framingham: QTcFr=QT+0.154(1000-RR)
RR��ñ�̤�msec����Ѥ��롥
ʿ�ѡ��������� 400msec, ���� 414msec
�ˤ��������ڼ����Ϥ����20�ͤ��Ǥ��ϤĤ褤��
����
QTc 480ms �ʾ� 3
460ms �ʾ� 2
450ms �ʾ� 1
���ܽ۴Ĵ�ز���Ǵ��
gnuplot
set grid
set xrange [40:160]
plot 480*sqrt(60)/sqrt(x) with lines lw 2 dt 1
replot 460*sqrt(60)/sqrt(x) with lines lw 2 dt 2
replot 450*sqrt(60)/sqrt(x) with lines lw 2 dt 3
replot -1.9*x+527 with lines lw 2
replot 360*sqrt(60)/sqrt(x) with lines lw 2 dt 4
replot 340*sqrt(60)/sqrt(x) with lines lw 2 dt 5
replot 330*sqrt(60)/sqrt(x) with lines lw 2 dt 6
 lqt.gif
QT���֤�R-R�ֳ֤�1/2�ʾ�Ǥ����long QT, ���ʤ��QT��Ĺ�ɸ����Ȥ�����
�㥫�ꥦ���ɤ�U�Ȥ�T�Ȥβ�����ʬ��ͻ�礷�Ƥ��뤿���U�Ȥ�QT���֤�
�ޤ������褤��
��������̮��ȯ������U�Ȥ�QT���֤˴ޤ�ʤ��Τ������Ǥ��롥
lqt.gif
QT���֤�R-R�ֳ֤�1/2�ʾ�Ǥ����long QT, ���ʤ��QT��Ĺ�ɸ����Ȥ�����
�㥫�ꥦ���ɤ�U�Ȥ�T�Ȥβ�����ʬ��ͻ�礷�Ƥ��뤿���U�Ȥ�QT���֤�
�ޤ������褤��
��������̮��ȯ������U�Ȥ�QT���֤˴ޤ�ʤ��Τ������Ǥ��롥
 1.5 mEq/L����K���
U�Ȥξ��P�Ȥ���äƤ��롥
1.5 mEq/L����K���
U�Ȥξ��P�Ȥ���äƤ��롥
 Romano-Word syndrome
QT��Ĺ�ɸ����Dz��٤⼺��ȯ������Ƥ롥����T�Ȥ�����U�Ȥ������롥
Romano-Word syndrome
QT��Ĺ�ɸ����Dz��٤⼺��ȯ������Ƥ롥����T�Ȥ�����U�Ȥ������롥
 ��Ca���
ST�������Ȥϥե�åȤDZ�Ĺ���롤T�Ȥ��ȷ������
QT��Ĺ�ɸ����Dz��٤⼺��ȯ������Ƥ롥����T�Ȥ�����U�Ȥ������롥
��Ca���
ST�������Ȥϥե�åȤDZ�Ĺ���롤T�Ȥ��ȷ������
QT��Ĺ�ɸ����Dz��٤⼺��ȯ������Ƥ롥����T�Ȥ�����U�Ȥ������롥
 R on T����Torsades de Pointes
T�Ȥξ�ǿ����������̤˻�������Ƴ��ȯ����2��̮�Ǥ��롤���θ塤�ȥ륵�ǥݥ���ȯ����
�Ƕ��QT��Ĺ�ɸ���������������
QT��Ĺ�ɸ����ο��ſ��Ѳ�
R on T����Torsades de Pointes
T�Ȥξ�ǿ����������̤˻�������Ƴ��ȯ����2��̮�Ǥ��롤���θ塤�ȥ륵�ǥݥ���ȯ����
�Ƕ��QT��Ĺ�ɸ���������������
QT��Ĺ�ɸ����ο��ſ��Ѳ�
Short QT Syndrome
Short QT Syndrome.pdf
14-1 J���դ��ξ����T�Ȥ�scooped�Ȥ�����Benign Early Repolarisation (BER)
14-2 J���դ��ξ����T�Ȥ�scooped�Ȥ�����PRD�������롥pericarditis. cf 10-1
ȿžT�ȡ�
14-3 �ͻ�ʿóT��(NSSTC)���������оη��α���T�ȡ������Ѳ���
14-4 �ͻ�ȿžT�ȡ�aVF����������Ϥ��٤�ȿž��������T�ȡ�wandering P,
�����Ѳ���
GE #93 �������ײ�ž������ͶƳ�Ͽ���ȿžT�ȡ�Non-Q MI.
14-5 II,III,aVF�ΰ۾�Q�ȡ�III�Ͼ�T�ȡ�V1��V6�ο���ȿžT�ȡ�LAE.
ischemia, CNS, electrolyte, pericarditis, IWMI. ��Ƚ�ǡ�
14-6 TR��V1��V2, RVH�ε��������뤬�����ξ�����о�T�ȤǤ��롥�о���T�Ȥ�
���ȥ쥤��ǤϤʤ��Τ�����Ǥ��롥
�ƥ�Ⱦ�T��
14-7 V2,V3�ϥƥ�Ⱦ�T�Ȥˤߤ��뤬���ͻ��ޤ�¾�Ǥ�T�ȤϾ�������
Q-T��Ĺ����Ca��ɡ��ͻ�����Ṳ̋϶��塥RAE��LAE��V5��V6��ST�㲼�ȵ�žT�ȡ�
cf 14-18�Ȥ���ȡ�V6��žT�ȤϻϤ�˱��������̤�2�����Ǥ��롥
14-8 V2��V5�ޤǤϥƥ�Ⱦ�T�ȤǤ��뤬������¾�Ͼ�������IVCD, ��K��ɡ�
V6��RBBB��RS�ȤˤʤäƤ��ʤ���IVCD�Ǥ��롥
14-9 AV sissociation��wide-complex tachycarda.
final�Ǥ�QRS����0.12�ðʾ�ǿ���100 bpm�ʾ��������Ƥ��롥
������Ż߾��֤��ʤ����֤��Ȥ�ɬ�ס�V2�Ǥ�P�Ȥ������뤬˼����Υ��
ȯ�����Ƥ��뤫��VT��Ƚ�ǤǤ��롥
14-10 �⤯�����������ݤ�T�ȡ�CNS�ޤ��Ϲ�K��ɡ�TR��V2��V3��2������T�ȡ�
14-11 3rd AV block LBBB�ͤ�ventricular escape��IVCD�ǤϤʤ�.
14-12 hyperacute AMI�����ɱ������ɡ�I, aVL��ST�㲼�ϥߥ顼�������V1��V4
��ST�徺�ϸ��ɹ��ɤΥߥ顼�������
14-13 ʿóT�ȡ�LAH��V1���������о�T�Ȥǡ��Ĥ���о�T�ȡ�������ECG�ȡ�
14-14 AV dissociation, Junctional escape beat. V2��ST�徺��
CNS������������ȿžT��
14-15 �оη��ǿ�����žT�Ȥ�CNS������ŵ����
14-16 PVC, �ͻ����Ű̡�II, III, aVF��������ȿžT�ȡ�TR��V4��V5��V4��V6��STD��
P�Ȥ�̵����Junctional escape, LVH��Ƚ�ǡ�
CNS�����Ǥ��롥V1��V3��T�Ȥβ������˱��줿P�Ȥ������롥
14-17 �ͻ�����T�ȡ�V1��ST�徺��V2,V3�������͡�V4��V6��ST�徺ȿžT�ȡ�
������ֹ��ɤ�Ķ��������
14-18 �ͻ�ʿóST�������ȡ�����2����T�Ȥǡ�ʿóST������QT��Ĺ��
��Ca��ɡ�14-7�Ϲ�K��ɡ���Ca��ɤǤ��롥T�ȤϾ�������ST������ʿó��
QT��Ĺ����ħ��V6��Ʊ�ͤ�2����T�ȤˤʤäƤ��롥
�������
14-19 �ե�åȤ�ST�㲼��T�ȡ�T�Ȥ��Τ�ΤϾ������
severe inferolateral ischemia.
14-20 II, III, aVF��STE��I,aVL�Υߥ顼��V1��V5��STD�����ɱ������ɡ�
���ɹ��ɤȤ����V6�ι����Ѳ����ʤ����������äƹ��ɤϱ�������
V4��V6�ϥ��ȥ쥤���LVH���ɤ�롥
14-21 II, III, aVF�ΰ۾�Q�Ȥ�ST�徺��V1��V4���������ȷ���V1��QS�ȡ�
V5��V6��Q�Ȥ�STE��
���ɹ��ɡ�������֤Ϲ��ɤ����������Ƚ�ǡ����̤�V6�ޤǤ�
������Ϥʤ���
14-22 ��ʿ��ST�ϵ���ȿ����V1��V4�ޤǤ�������T��ȿž��
II, III, aVF��T�Ȥ����оΤ�����Ǥ��뤫�顤����q�Ȥ�����ȹͤ��롥
���ɹ��ɤ��������
���ȥ쥤��Strain Pattern
J���ϲ��ߡ�����������ST�������ȡ�ȿž���о�T�Ȥ���ħ��
14-23 ����P�ȡ������а̡�II, III, aVF�Υ��ȥ쥤��T�ȡ�V1, V2�ι�R�Ȥ�
���ȥ쥤��V6��RS�ȡ��������硥
14-24 RBBB������ͶƳ��14-23�Ȼ��Ƥ��뤬QRS����0.12�ðʾ�Ǥ��ꡤV6��S�Ȥ�
���顼��
14-24 �����а̡�ξ��˼���硤1SQ3T3���������Ṳ̋�꺸�����硤ξ�������硥
�������礬�����V1, V2��R�Ȥϱ���롥
14-53 pericarditis, early repolarization, PRD��0.8mm�ʲ���
14-54 pericarditis, early repolarization, PRD��0.8mm�ʾ��ͭ�١�
14-55 early repolarization (early ropol)
14-57 IVCD
14-58 CRBBB+LAH
14-59 CLBBB+¦�ɵ��졤LBB�Ǥβ���STD������ȿ����
15-13 CRBB��LAH��ȯ����������������ֹ��ɡ�
I,aVL��STE��II,III,aVF��STD��V1-3��STE��V4�ǤϿ�ʿST�������ߤ��롥
V5-6���礭��S�Ȥθ�˾����T�Ȥ��ߤ��롥
I,aVL��STE�����¦��AMI����ǡ�
�̾��CRBBB��13-14, 13-15�Ǹ����롥
15-25 ���ɱ������ɡ�
15-26 ���ɱ������ɡ�
15-27 ���ɱ������ɡ�V4��V5��ST��ʬ�ο�ư��������
15-28 Posterior Wall AMI
15-29 �Ť�IWMI��PWMI��LWMI���������Posterior Wall AMI
15-30 ����IWMI��PWMI��LWMI
15-31 ����IWMI��PWMI��LWMI
15-32 LBBB�˵���IWMI��PWMI��LWMI
15-33 ����IWMI��PWMI��RVMI
15-34 ����IWMI��PWMI��RVMI��V1��STD�Ϥʤ���V4-V6�ޤǤ�STD��V6R��STE��
II���IIIͶƳ��STE���������ɤ���ħ�Ǥ��롥
15-35 ����IWMI��PWMI��RVMI��V5-V6��STE�����ʤ����ᱦ��ư̮�ܴɤι��ɤ�
�ͤ��롥
16-6 ��K��ɤˤ��IVCD
16-7 ��K��ɤˤ��IVCD
16-8 ��K��ɤˤ��IVCD
16-9 ��K��ɤˤ��IVCD
16-10 ��K��ɤˤ��IVCD��P�Ȥ�wandering atrial pacemakter.
16-11 ��K��ɤˤ��IVCD
16-12 ��K��ɤˤ��IVCD
16-13A ��K��ɤΥƥ�Ⱦ�T��
������������PR�������Ȥ��㲼����ST�徺�ȴְ㤨�롥
�褯����ȡ����٤Ƥλͻ�ͶƳ��ST�徺�Ǥ��롥��ͳ�ϡ�
��ǹ�˿夬���ޤꡤ������¦��˦���Ṳ̋��Ű��㲼�ˤ�롥
����ͶƳ��R, L, F�Ṳ̋��ߥå�������뤿�ᡤST�徺�ο��Ǥ����롥
�̤ιͤ�����PRD (PR depression) �Ǥ��롥�������������鸫�Ƥ�ST�徺�Ƥ��롥
PRD���������狼��ʤ������Ṳ̋Ͽ��ſ����ϳ�Ťˤ�롥VͶƳ�Ǥ����Ű̡�
 prd.png #191
IMG_20170912_0005.pdf
final p.142��ꡧ
�ܹ���ĴΧ��II��P�Ȳ�������QRS�����Ǥ�0.12�ð��⡤��Ǥ�0.19�ð��⡥
����P��
P�Ȥ��ŵ�����0��75�롤Junctional P��-60��-80�롥p.91
P-mitrale(LAE): p.93
I�ޤ���II������0.12s�ʾ塤hump��ĺ���֤�0.04s�ʾ塥
ĺ���֤�0.04s�ʲ��ʤ�LAE�ȤϿ��ǤǤ��ʤ���
P-pulmonale(RAE): p.99
�⤵��2.5mm�ʾ塥����ʲ��ʤ�RAE�ǤϤʤ���
V1ͶƳ��P�Ⱦ��������ե�åȤˤʤ뤳�Ȥ����롥
�ŵ����������аܤǡ�RAE�ʤ顤LPH��¸�ߤ��ʤ���
��˼����Ƴ�ٱ�(IACD)��p.105
V1��2������P�ȤǤ��뤬���ͻ�ͶƳ������P�Ȥ���˼��P�Ȥˤʤ�ʤ����֡�
ex1 V1����Ⱦ�ι⤵��V6�ι⤵����礭����� -> RAE�β�ǽ�����⤤��
ex2 V1�θ�Ⱦ�δٱ���1mm�������������� -> LAE�β�ǽ�����⤤��
ξ��˼����(BAE)��p.117
ex1 IIͶƳ������P�ȡ�V1��2���ܤδٱ�
ex2 IIͶƳ����˼P�ȡ�V1��1���ܤγ���
final p.79
prd.png #191
IMG_20170912_0005.pdf
final p.142��ꡧ
�ܹ���ĴΧ��II��P�Ȳ�������QRS�����Ǥ�0.12�ð��⡤��Ǥ�0.19�ð��⡥
����P��
P�Ȥ��ŵ�����0��75�롤Junctional P��-60��-80�롥p.91
P-mitrale(LAE): p.93
I�ޤ���II������0.12s�ʾ塤hump��ĺ���֤�0.04s�ʾ塥
ĺ���֤�0.04s�ʲ��ʤ�LAE�ȤϿ��ǤǤ��ʤ���
P-pulmonale(RAE): p.99
�⤵��2.5mm�ʾ塥����ʲ��ʤ�RAE�ǤϤʤ���
V1ͶƳ��P�Ⱦ��������ե�åȤˤʤ뤳�Ȥ����롥
�ŵ����������аܤǡ�RAE�ʤ顤LPH��¸�ߤ��ʤ���
��˼����Ƴ�ٱ�(IACD)��p.105
V1��2������P�ȤǤ��뤬���ͻ�ͶƳ������P�Ȥ���˼��P�Ȥˤʤ�ʤ����֡�
ex1 V1����Ⱦ�ι⤵��V6�ι⤵����礭����� -> RAE�β�ǽ�����⤤��
ex2 V1�θ�Ⱦ�δٱ���1mm�������������� -> LAE�β�ǽ�����⤤��
ξ��˼����(BAE)��p.117
ex1 IIͶƳ������P�ȡ�V1��2���ܤδٱ�
ex2 IIͶƳ����˼P�ȡ�V1��1���ܤγ���
final p.79
˼���ܹ���ĴΧ��A-V junctional rhythm.
�����ˤϿ����40��60���٤ǡ�QRS������120m sec�ʲ��������ȷ���
ƶ˼ĴΧ����»���뤿���˼���������ĴΧ�Ȥʤ롥
�չ����˿�˼�ȷ���QRS�θ�Ǹ����뤳�Ȥ����롥
 ��ޤϿ������73�Ǥ��뤫�顤¥�����ܹ���ĴΧ�Ȥ�֡�
��ޤϿ������73�Ǥ��뤫�顤¥�����ܹ���ĴΧ�Ȥ�֡�
V1��R�Ȥδ��̿��ǡ�
Right ventricular hypertrophy
Right bundle branch block
Young children and adolesents
WPW type A
Posterior wall AMI ecg 11-22, GE #57
ecg 11-12, ŵ��Ū��������
ecg 11-13, ������ֹ��ɤ�ʻȯ���Ƥ��뤿���V1�ˤʤ�ʤ��������硥���̿��ǡ�
GE #28��II,III,aVF�ΰ۾�Q�ȡ�V5-6�ΰ۾�Q�Ȥˤ�겼��¦�ɹ��ɡ�V1-2��RS�Ȥ�
���ɹ��ɤΤ���˹⤤R�Ȥˤʤ롥
GE #35��Af��V1��QR��V2��rSR'������V6��s�Ȥˤ��IRBBB��
GE #57��¦�ɸ��ɹ��ɡ�V1-3���о�����T�ȡ�
ge312.png
GE #312: ���豦�ӥ֥��å��Ǥ��ä�ECG������¦�ɹ��ɤ�ȯ����
���η�̡�V1��rsR'�Ǥ��ä��ȷ���qR�ˤʤä���V2-6�ζ�ü��STE��
�������ȷ��ˤʤäƤ��롥
I��aVL��STE���ߤ�졤II, III, aVF��STE��T�ȹ�徺�������롥
����ϵ������ɤν���ɾ��Ǥ��롥
12 Lead ECG p.253
ge #304 ���ɸ�α��ӥ֥��å����չ���P�Ȥ�T�ȤΤ��Ȥˤ��롥
T�Ȥβ���������Ĺ��QTc��������K�⤷����Mg���Ų���۾����̮�����ա�
His����Ϥ���˱��Ӥ�ʬ�ޡ����θ庸�Ӥ������ޤȸ�ޤ�ʬΥ���롥
���Ӹ�ޤϹ����ޤ狼��뤿�Ẹ�Ӹ�ޥ֥��å��ϵ��Ǥ��롥
���ſޤ�V1��RSR'���ޤ���QR'�ˤʤ롥V6�Ǥ�S�Ȥ���ǧ�Ǥ��롥
R'�Ȥβ����ϥ��顼���ޤ�S�Ȥϱ����κ�˦����Ƴ�Dz��������⥹�顼�ˤʤ롥
�� ���ӥ֥��å��DZ�������Ͽ��ǤǤ��ʤ����������˴ؤ��ƤϿ��ǤǤ��롥
IRBBB��LAH�Ͽ��Dz�ǽ��ecg 10-21
�ޤ������ӥ֥��å���������ֹ��ɤ���ǤǤ��롥GE #100
�� �Դ������ӥ֥��å���V1��rSR'�ˤʤ�ʤ���rS�ǡ�V2��rSR'�ˤʤ��Τ⤢�롥
V6��S���礭����Ф��Τ褦�˿��Ǥ��뤬��V6��S�����������IVCD�ο��Ǥ���ǽ���⤷��ʤ���
�ޤ����Դ������ӥ֥��å����������硤IVCD���֥륬���ɸ����Ͽ��̤ɤ����Ǥ��롥
13-1
13-2
13-3
Luna: Clinical Electrocardiography p.162
���ӥ֥��å���Ω�Υ٥��ȥ�ޡ�
20180729102729.png
rSR'���α��ӥ֥��å���������ɹ��ɤ�qR���ˤʤ�ᥫ�˥��ࡥ
IMG_20190922_0001.png
QRS < 0.12sec, Axis <-30��(�����а� 205), final p.89
(�������ޥ֥��å� 511)
���ա�
�������ޥ֥��å���IIͶƳ���ݡ��������äơ����ɹ��ɤ�Q�Ȥȶ��̤���
ɬ�פ����롥ɬ��r�Ȥ�¸�ߤ�Τ���뤳�ȡ�BB p. 115.
LAFB�ǻ�����q�Ȥ�V2, V3�Ǹ����뤳�Ȥ����뤬���������϶��������ɹ��ɤǤϤʤ���
���̤�LAFB�ζ���ͶƳ��S�Ȥ��礭���ʤ뤬���ä�
GE #73��LAFB�ȶ���V1-V6�ޤ�rS�ȷ��Ǥ��롤
����ͶƳ��PRP��V6��S�Ȥ�ȯ�����롥��ޥ֥��å��ȶ��̤Ǥ��ʤ���
�ͻ�ͶƳ���ŵ����Τߤǿ��Ǥ��롥
Luna: Clinical Electrocardiography p.184
20180729103222.png
QRS < 0.12sec, Axis >90��(�����а�), final p.90
������������GE #100��1��˼���֥��å���������ֹ��ɡ����Ӹ�ޥ֥��å���
����ͶƳ��PRP��V6��S�Ȥ�ȯ�����롥���ޥ֥��å��ȶ��̤Ǥ��ʤ���
�ͻ�ͶƳ���ŵ����Τߤǿ��Ǥ��롥
Luna: Clinical Electrocardiography p.189
20180729103422.png
BB p.128
���ӥ֥��å�����ħ��V1��rS���ޤ���QS�ȷ��ǡ������ȷ���V4���٤ޤ�³����
V6�Ǥ�q�ȤΤʤ�R�Ȥ������ȷ��ǡ�RR'���ΥΥå��������뤳�Ȥ⤢�롥
�ޤ�V6�Ǥ���Ƴ�ٱ�Τ����VAT��0.05�ðʾ�ˤʤꡤ
�ǥ륿���ͤΥ��顼�ȷ������Ȥ⤢�롥����ϱ���
��ֿ��ڤ����˦�ֶ�ʳ��Ƴ�ˤ�ꡤ������ֿ��ڤ�ʳ�����뤿��Ǥ��롥
VAT��Ĺ����ID�����������R�ȤΥԡ����ϸ�ˤ���롥
��ֿ��ڤα����ؤζ�ʳ���ʤ�����I�����aVL�Ǥ�q�Ȥ������ʤ���
���ӥ֥��å��ˤϴ������ӥ֥��å����Դ������ӥ֥��å������ꡤ
QRS < 0.12sec�Ǥ�����Դ���������ʾ�����Ǥ���д������ӥ֥��å��Ǥ��롥
�������ӥ֥��å��Ǥ�T�Ȥ�R�Ȥ��Ф��Ƶ�ž(discordant)���Ƥ��뤬��
�Դ������ӥ֥��å��Ǥ���а���(concordant)���뤳�Ȥ�¿����
����Ͽ�����¦��ư�Ṳ̋��ٱ䤬���ʤ���а��פ����礭����ȿž���롥
�ޤ��츫�ǥ륿�ȤΤ褦��R�Ȥξ徺�������뤳�Ȥ⤢�롥
QRS���������ۤɿ���ǽ���㲼���롥�ޤ���ü�˿������ˤʤ��T�Ȥ�
����(concordant)���Ѳ����롥������ͳ��������
�ŵ����Ͽ�ʿ�������QRS���Ϲ����ʤꡤ����ǽ���㲼����
��ľ������ȿ��ھɤ�ȼ��ξ��������ĥ����(BB p.130)��
BB p.128 fig 10.13���
���ӥ֥��å��ޤȤ�
Luna: Clinical Electrocardiography p.174
���ӥ֥��å���Ω�Υ٥��ȥ�ޡ�
20180729103030.png
������ֹ��ɤǤκ��ӥ֥��å���
��ֹ��ɤ��ʤ����V1��r�ȤϤʤ���V6�Ǥ���֤ȿ���������ζ�ʳ�Τ����V6����ä����������롥
��ֹ��ɤ�����С�V1��r�Ȥ������뤬����¦�ɶ�ʳ�Ǥ��롥�ޤ���V6��q�ȡ����ʤ�R�Ȥ�ȯ�����롥
IMG_20190922_0002.png
����T�Ȥ��ȹ�ϻͻ�ͶƳ�Ǥ�6mm�ʲ�������ͶƳ�Ǥ�12mm�ʲ��Ǥ��ꡤ����ʾ�Ǥ���й�T�ȤǤ��롥R�Ȥޤ���S�Ȥ�2/3�ʾ���T�ȤȤ���������ˡ������оΤǤ��뤳�Ȥ������� (p.325)��
positive ����T��
negative ����T��
flipped ȿžT�� (��������T�ȤʤΤ˱���T�Ȥˤʤä�����)
��K��ɡ� p.504 ecg 16-6.
�ƥ�Ⱦ�T�Ȥ�5.5mEq/L�Ǹ����롥
PR�ֳ֤α�Ĺ��6.5mEq/L�ʾ塤7.0mEq/L�ˤʤ��P�Ȥθ��塤
8.8mEq/L�ʾ����P�ȤϾü����롥
 ����K+������ǻ�٤�8.2mEQ/L���������������Ԥο��ſޡ�
����K+������ǻ�٤�8.2mEQ/L���������������Ԥο��ſޡ�
��ĥ�����ھ�(����)�������첼���ɡ�Ǿ��ɾ㳲
WJC-7-86.pdf
Luna: ECG text p.124
������Ͽ��ڤ�����ǿ��ƹ��Ͽ������Ѥγ���Ǥ��롥
��������Ǥ�V1��R�Ȥ���������о�T�Ȥ�ȿž��
��������Ǥ�V5-6��R�Ȥ���������о�T�Ȥ�ȿž��
������ĥ�Ǥ�V1��rSR'����������о�T�Ȥ�ȿž��
��������Ǥ�V6��qR�ȹ⤤�о���T�Ȥ���
RVE: right ventricular enlargement
V1�ޤ���V2��S��+V5��R�� > 35mm
�����줫�ζ���ͶƳ > 45mm
aVF > 20mm
aVL > 11mm
I > 12mm
V4, V5, V6�DZ���T��
������ĥ
����T�ȤǤʤ��Ƥ�褤��
V5, V6��ST�ٱ�������T��
II, III, aVF��1mm�ʲ��ξ�����Q�� cf ecg 11-4, 11-5
LPFB�ν������Ǥ�ɬ�ס�
RVH�ϴ���Ū��3�̤�ο��ſ��ȷ������롥BB p.73
���ƤΥ����פ� Axis > 90��϶��̤��롥
1) V1��R/S > 1. T�Ȥϥ��ȥ쥤��ˤʤ롥
11-12 �����а̡�ȿ���ײ�ž��V4-6��S�ȤϤʤ���V1��RS���Ǥ��롥
11-13 V1��R/S�Ͼ���������V2��R/S >1, DDX�η�̱��������Ƚ�ǡ�
V1-3�Υ��ȥ쥤��T�ⱦ�������Ƚ�Ǻ����ˤʤ롥
BB p.73, fig7.16
BB p.74, fig7.16A
GE #41
V1����礷�Ƹ����rsR'��IRBBB��Ʊ�������Ǥ��롥������QRS��0.9sec�Ǥ��뤫��
IRBBB�ǤϤʤ���V6�ǤϺ�����ʳ�θ�˱�����ʳ��ȯ�����롥
2) V1��qR��R�ȹ⤬7mm�ʾ塥
IRBBB�ȶ��̤���ɬ�פ����롥V6��S�Ȥ����㡼�פǤ��뤳�Ȥ��ǧ���롥
IͶƳ��rS�ȡ����ʤ�������а̤Ǥ��롥
BB p.74, fig7.16B
AF����������P�ο��Ǥ��Ǥ��ʤ���
GE #309 ��>90���ͻ趻�����Ű̡�V1��qR��V2-4��qrS, V5-6��RS��COPD�α������硥
���ǡ�4:1��AF��nodal��RVH�������а̤����Ṳ̋Ǥʤ����IRBBB������
���뤳�Ȥ��Ǥ��ʤ���������S�Ȥ����Ϻ�˦����Ƴ�Ȥ��ɤ�롥
3) V1����V6�ޤ�rS�ȡ�V1��QS�ȤǤ�褤��
BB p.74, fig7.16B RVH
BB p.74, fig7.16C RVH
1,2,3)���̤���V6��S�Ȥ����̤��롥
�����ȱ����Ȥ��ϴط��DZ��������ä����֤ȹͤ����Ǽ���Ǥ��롥
COPD(fig7.17)��S1S2S3����Ʊ�������Ǥ��롥
4) COPD�ǤϿ�¡��ũ���ˤʤꡤ��������P�Ȥ����Ṳ̋ˤʤ롥�ä�I��
�������ʤ��������������������뤿���Ǥ��롥
����ͶƳ�ο����⾮��������V1��S�ȡ����θ塤R�Ȥ����⤬�ߤ��뤬��
������V3�����硤V4�ʾ�Ͽ�¡����ʤ뤿�Ḻ�ꤹ�롥���ײ�ž�Ǥ��롥
BB p.75, fig7.17
GE #42��V6�Τ�RS�ǻĤ�ζ�����rS�ȤǤ���(�ٵ���)��
GE #198�ζ�����rS�ǻϤޤ�Ʊ�ͤο��������������롥
5) ��ͤ�S1S2S3��. ���ξ�硤�ŵ�����NE�˸����������ʤ��rS�ȤDZ����а̤�Ʊ����
���Τ���aVR��qR�ˤʤꡤ
aVL��rSr'�ˤʤ롥V1��qR�ȡ��������ײ�ž��V6��S�Ȥϥ��㡼�ס�R�Ȥ�����Ϥʤ���
BB p.75, fig7.18
6) �ٹ��ɤ���̮�����ܡ�S1Q3T3�ǡ�����90��ʾ塥���Τ���aVR��qR�Ȥˤʤ롥
V1��qR�ȡ�V6��RS�ȡ�����S�Ȥϥ��㡼�פǤ��롥
BB p.76, fig7.19
7) ξ�������������P�Ȥ�V1�ι⤤RS�ȤǤ��θ�Ϻ�������η�������
���Ϻ�������αƶ���90��ʲ��Ǥ��롥
BB p.76, fig7.20
final p.27 ��16����(����P�Ȥ�ȼ�äƤ���)��
�ŵ����ϱ����аܡ�ξ������ʤ鱦���а̤ˤʤ�ʤ���
ecg 11-27, ecg 11-28.
TR��V1��V2��ȿ���ײ�ž�ʤ鱦��������ĥ��ͤ��롥
ST�ε�ž���ʤ���б�����ĥ��
ecg 13-30������P�ȡ������а̡�S1Q3T3�α�����������Ǥ��Ĥ���
V1��qR�Ǥ��ꡤ�츫���ӥ֥��å��˸����롥����q�Ȥ���ֶ�ʳ�Ǻ����˸�������
³��R�Ȥϱ������̤ο��ڶ�ʳ�������ʤꡤ������ʳ��S�ȤΤ���̤Ǥ��롥
BB p.118, fig9.13��I�ǡݡ�aVF�ǡܤ����鱦���а̡�II,III,aVF������P�ȡ�
����V1�Ǿ�����QS�ȡ�v2��V6�ޤ�rS�Ȥ�R�Ȥ������ʤ���
�������ײ�ž�Ǥ��롥����������������ȿ��Ǥ��Ƥ��롥
V1�ޤ���V2��R/S�椬1�ʾ塥
V1�ޤ���V2�����ȥ쥤��T�Ȥǵ�ž��
V6�Ͽ���S�Ȥ⤢���̵�����⤢�롥cf ecg 11-12.
������ֹ��ɤ�V1��r�Ȥ�Q�Ȥˤʤ�ȡ����θ�α��������V1��R�ȤϾ������ʤ롥
cd ecg 11-13.
����Ū�ˤϡ�
���������Ʊ�ͤ˹��Ű̡�ST�������Ȥϥ��ȥ쥤���žT�ȤǤ��롥
�����֥��å��Ǻ�������ο��Ǥ��Ǥ��ʤ��Τ�Ʊ�ͤˡ�
���ӥ֥��å��Ǥϱ�������ο��ǤϤǤ��ʤ���
Benign Early Repolarisation. ���������ʬ�ˡ�
��ǯ������¿����Osborn�Ȼ����Υå���QRS��³���Ƹ����롥
J�Ȥޤ���J���Ͼ徺����˱���ST�������Ȥ�T�Ȥ����оΤǹ⤤��
There is elevation of the J point
The T wave is peaked and slightly asymmetrical
The ST segment and the ascending limb of the T wave form an upward concavity
The descending limb of the T wave is straighter and slightly steeper than the ascending limb
�Υå��դ���ST�������Ȥ�"fish fook" patern�Ȥ�����
 ̮����ʤ��STE�������ꡤ�������롥
�����ˤ����ꡤ��������AMI�����ȷ��롥
�������Ǥ�PR�������Ȥ��㲼�����뤬��BER�ˤϤʤ���12 Lead p.129, ECG 10-1.
50�Ͱʾ�ˤʤ��STE�ϸ�������AMI���θ���롥70�Ͱʾ��BER�ϵ��Ǥ��롥
̮����ʤ��STE�������ꡤ�������롥
�����ˤ����ꡤ��������AMI�����ȷ��롥
�������Ǥ�PR�������Ȥ��㲼�����뤬��BER�ˤϤʤ���12 Lead p.129, ECG 10-1.
50�Ͱʾ�ˤʤ��STE�ϸ�������AMI���θ���롥70�Ͱʾ��BER�ϵ��Ǥ��롥
 ��ŵ��34_368.pdf
BER(Benign Early Repolarisation)
��ŵ��34_368.pdf
BER(Benign Early Repolarisation)
akiyamalecture11.pdf
Non Q-Wave MI
���ˤȹ��Ǿ徺�����äư۾�Q�Ȥ�ȯ�����ʤ����ɡ�
Evolving ST-T changes may include any of the following patterns:
* Convex downward ST segment depression only (common)
* Convex upwards or straight ST segment elevation only (uncommon)
* Symmetrical T wave inversion only (common)
* Combinations of above changes
Non-Q Wave MI
GE #283
GE ��Q�ȹ���
2019ǯ 9�� 11�� ������ 14:56:39 JST
�۾�Q�Ȥ�������
����ιͤ�����
Q1.png
��A������ο��ڤǤϿ�����¦(�������)�Ǥ�1�˼���QS����æʬ���Ṳ̋�¬�ꤵ�졤
������¦�Ǥ�6�˼���R����æʬ���Ṳ̋������롥������Ǥ�2��5�˼����褦��
r�Ȥ�������礭���ʤ���ַ����ȷ�����¬�����ȹͤ����롥
��B�����������ɤǤϹ�����ڤ����ष�Ƥ��뤿�ῴ����¦�Ṳ̋Ͽ�����¦�Ṳ̋�
ľ��ϳ�Ť��뤿��˰۾�Q�ȤȤʤ롥�������̤Ȥζ������̤Ǥ�QR���Ȥʤ롥
��C�������칼�ɤǤ��ꡤ���ɤ��ޤ���˿�����¦�˵ڤ�Ǥ������Qr���Ȥʤ롥
��D��������¦�������Ū�ʹ��ɤ�������¦�˵ڤ�Ǥ������������̤����ʤ��ʤ�
�����R�Ȥ��ȹ��㤯�ʤ롥
�ͻ���
���ιͤ�����Wilson������ The theory of electrical window�ˤ�롥
��˦��������֤Ǥ���л��������ʤ��졤�ŵ�����٤����˹⤤��������
��˦��ʤɤξ㳲��ȯ������Ⱥ�˼�����������㲼����������¦���鿴����¦�ؤ�
�ŵ���Ƴ����ȯ������QS�Ȥ����Τޤ�����¦��¬�ꤵ�졤�۾�Q�Ȥˤʤ�Ȥ���
�ͤ��Ǥ��롥
�������������˿�����¦�Ṳ̋�QS���Υѥ륹�ȷ��Ǥ������������ơ��ƥ��Ŷˤ�
����������ü�Ҥ�¬�ꤹ���QS�Ȥ���¬����뤬���ݶˤ���ɽ�����夷���ŶˤǤ��롥
�������äơ�����ξü�Ҵ֤��Ű̺���QS�ȷ�����¬�����˲�������ο������Ṳ̋�
���ڳ�ư�Ṳ̋�ȿž�ȷ��Ǥ���ȹͤ���٤��Ǥ��롥
����ιͤ�����
���ں�˦�����ɤˤ���������Ȥ��Ƥε�ǽ���ʤ��ʤ��
��ư�Ṳ̋��ü�����ȤȤ���ŵ���Ƴ�٤����ä��롥
���äƾ㳲���Ȥ줿������¦���ڤ�ȯ�����뿴�����Ṳ̋�������¦��ϳ�Ť��롥
���줬�۾�Q�ȤȤ��Ƹ��Ф���롥���������ɤˤʤ�ʤ���а۾�Q�Ȥˤ�
�ʤ�ʤ����ޤǼ����Ȱʲ��ΤȤ���ˤʤ롥
infarc.png �۾�Q��ȯ���ᥫ�˥��ࡥ
�ޡ��۾�Q�Ȥ�ȯ��������
1/4�ʱߤϿ��������Ҥ��������ϴ������������̤���������¦��˦���Ṳ̋�
������������¦��˦���Ṳ̋������Ǽ������ޤ��������̤��ϳ��Ǥ�
������¦��˦���Ṳ̋��������Ǽ��������ޤϤ��줾���ȿž�ȷ�������
��碌�ƾ��꿴����¦��������¦�Ű̡����ΰ������ȷ�����ɽ���ſޤȤʤ롥
������¦��2�ȷ�������˲��Ť��졤�ޤ�������¦�Ṳ̋��Ԥ�ɽ��뤿���
����������ȱ�����Q�ȤȤʤ롥������¦��˦���Ṳ̋��ϳ�Ť��뿴����¦�Ṳ̋�
�����Ԥ�Ω������
12 Lead p.418��
���������ɤǤϲ��ष�������ɤ�����פˤʤäơ���¦�ɤ�R�Ȥ�ո�����
��¬���롥���������ɤǤʤ����Ǥ�1/3�ʾ�β����ؤο���������ȡ�
�������̤�Perkinje��˦�ζ�ʳ�Ϥʤ������Τ���������Ĥä����ڤˤ�
cell to cell���š��Ĥޤ��˦����Ƴ�Ƕ�ʳ������롥�����ٱ���֤�
�֡����Ϥ���ո����ζ�ʳ��ή����¬����롥
������ˤ��衤T�ȵ�ž�������Ϥʤ���
12 Lead p.207.
�۾�Q�� Signifificat Q wave
I��aVL��q�Ȥ�����Ǹ����롥�⤷0.03sec�۾�ʤ�۾�Ǥ��롥
III��q�Ȥ��ŵ�������ʿ�˸������ȸ���졤����Ǥ��롥
II��aVF��q�Ȥ�������Ȱ۾�Q�ȤǤ��롥
QS�ȷ���R�Ȥ��ʤ������Q�Ȥ�S�Ȥ�����̤Ǥ��ʤ����������ä�QS�ȤȤ�����
��������ˤ������q�Ȥ��㡥
9-17 IACD��LAE���㡤III, aVF��Q�Ȥ����������۾�ǤϤʤ���
I��aVL���礭�ʥΥå���IVCDefect�����������Ṳ̋�I, V5-V6�Υ��ȥ쥤��T��
��˼��١��������硥
final.pdf p.62 ��33
12 Lead�Ǥ�AMI��ʬ�ࡥ
Anterior Wll MI V3, V4 p.425
Anteroseptal MI V1, V2, V3, V4 p.426
Anteroseptal with Lateral Extention V1, V2, V3, V4, V5, V6 I, aVL p.431
Laeeral Wll V5, V6 LAD���гѻޤι��ɡ�
Hight Lateral Wall I, aVL p.443
Inferior Wll II, III, aVF p.446 ����ư̮�αԳѻޤι��ɡ�
Inferolateral AMI II, III, aVF, V5,V6 p.450
Apical AMI p.458
12 Lead p.425
��֤�V1,V2; ���ɤ�V3,V4��¦�ɤ�V5,V6,I�����¦�ɤ�aVL�Ǥ��롥
������ֹ��ɤϻͻ�ͶƳ�˥ߥ顼�ʤɤαƶ��Ϥ������ʤ���
15-1 V1��V5�ޤ�STE�ǿ�ʿ��R�ȤϻĤäƤ��롥aVL��STE�����Υߥ顼��
II,III,aVF��STD��
15-2 V1,V2,V3��Q�ȡ���ʿ���⤷���Ͼ������STE��T�Ȥ��оε�ž��V1����V4�ޤǡ�
aVL��q�Ȥ����
15-3 STE��V1��V4���۾�Q�Ȥ�V2��V4���о���ȿžT��V2��V4��IRBBB��LAF�Ǥ��롥
II,III,aVF��QS�ȤϤ��Τ���Ǥ��ꡤ�۾�Q�ȤǤϤʤ���
���ξڵ�˿�ʿST�Ǥ��ꡤAMI�Ȥ���ǧ����ʤ���
12 Lead p.425
GE #270, �������ɹ��ɡ�V2��V4��STD��T�����⤬�����롥
T������Ͽ�����¦���ڤ������ʬ�ˤ˸������롥
���ˤ���С�I��STD��II��STE��III��STE��ʿóT�ȡ�aVF��STE��
aVL��STD�������롥
ŵ��Ū��������֡�¦�ɹ��ɡ�V6��QS�ѥ������I, aVL�ΰ۾�Q�Ȥ����ա�
II, III, aVF�ϥߥ顼�������ST�㲼�������ɤ�����ڤǤ��롥
IMG_20180724_0006a.png GE #249
 IMG_20180724_0006a.png
p.431. ����ư̮���ĺɤǤ���С������ޤȲ����ޤ��ĺɤˤʤ롥
15-4 V1�����V2��V6�ޤ�STE�ι��ɡ�������q�Ȥ����뤬�������ϰϤ���
I,aVL��STE���ߥ顼��III,aVF��STD��������III���Ǥ�Ĥ褤�������ˤ�
q�Ȥ����뤬�������ϰϤ���
����Ǥ�q�Ȥϰ۾�Q�ȤǤ��롥Ķ������STE��
15-5 V1��V4��STE�ǥɡ������V5��V6���о���T�ȵ�ž��I,aVL��STE��
III,aVF�Υߥ顼STD��VͶƳ��R�Ȥ��ݤ���Ƥ��롥
����Ǥ�V5��STE�ǹ��ɥѥ�����
15-6 V1��V6�ޤǤΰ۾�Q�Ȥ�STE��I,aVL��STE��ȿžT�ȡ�II,III,aVF��STD�Ⱦ����
T�ȡ�
����Ǥ�V1��r�Ȥ�¸�ߤ��뤫��QS�ȤǤϤʤ���rS�ȤǤ��롥
15-7 V1��V5�ޤǤ�STE��I,aVL��STE��II,III,aVF�Υߥ顼��
15-8 Junctional P, I,aVL,V1��V6�ޤǤξ����ST������STE��
IMG_20180724_0006a.png
p.431. ����ư̮���ĺɤǤ���С������ޤȲ����ޤ��ĺɤˤʤ롥
15-4 V1�����V2��V6�ޤ�STE�ι��ɡ�������q�Ȥ����뤬�������ϰϤ���
I,aVL��STE���ߥ顼��III,aVF��STD��������III���Ǥ�Ĥ褤�������ˤ�
q�Ȥ����뤬�������ϰϤ���
����Ǥ�q�Ȥϰ۾�Q�ȤǤ��롥Ķ������STE��
15-5 V1��V4��STE�ǥɡ������V5��V6���о���T�ȵ�ž��I,aVL��STE��
III,aVF�Υߥ顼STD��VͶƳ��R�Ȥ��ݤ���Ƥ��롥
����Ǥ�V5��STE�ǹ��ɥѥ�����
15-6 V1��V6�ޤǤΰ۾�Q�Ȥ�STE��I,aVL��STE��ȿžT�ȡ�II,III,aVF��STD�Ⱦ����
T�ȡ�
����Ǥ�V1��r�Ȥ�¸�ߤ��뤫��QS�ȤǤϤʤ���rS�ȤǤ��롥
15-7 V1��V5�ޤǤ�STE��I,aVL��STE��II,III,aVF�Υߥ顼��
15-8 Junctional P, I,aVL,V1��V6�ޤǤξ����ST������STE��
¦�ɹ��ɤ�V5-6, ���¦�ɹ��ɤ� I,aVL�ΰ۾�Q�Ȥ���
15-14 I, aVL��STE��Tȿž��II, III, aVF��STD��V4-6��Tȿž�Τߡ�
BB p.118, fig 9.14
I��aVL��QS�ѥ�����LPFB�ȴְ㤨�롥LPFB�Ǥ�I��aVL��rS�Ǥ��롥
���ξ����V1��Qr��V2��V4�ޤǰ۾�Q��(QS�ѥ�����)���ġ�
����ͶƳ�˵�žT�ȤϤʤ��������T�ȤǤ��롥
III��q�ȤϤ褯�����뤬��II��Q�Ȥ�������Ȳ��ɹ��ɤβ�ǽ�����⤤��
LAFB��ʻȯ����ȿ��Ǥ����Τǡ�r�Ȥ�¸�ߤ��ʤ����Ȥ�Τ���롥
BB p.115, fig 9.6, II,III,aVF��T�Ȥ����ƾ������
GE #28�ϲ��ɹ��ɤ�V5,V6�˰۾�Q�Ȥ�겼��¦�ɹ��ɡ�
���ɹ��ɤ�ȼ�äƤ���ȹͤ���ȡ�
V1,V2�ι⤤R�ȤȤʤ뤬��V2-V3��T�Ȥ����оΤ������ȷ��Ǥ��롥
old age�θ��ɹ��ɤ�ŵ�������ѤǤ��롥
GE #28
 #28
�� final p.28�ο�18�β���ϴְ�äƤ��롥
V4,V5,V6��¦�ɹ��ɤΰ۾�Q�ȤǤ��롥���ι��ɤ����ɤ˵ڤӡ�V1��V2�ι⤤
R�Ȥˤʤ롥V5,V6��S�Ȥ��ʤ����Ȥϱ��ӥ֥��å��䱦����������ꤹ��ڵ�Ǥ��롥
2018ǯ 7�� 12�� ������ 16:51:08 JST
final�β���ϴְ㤤�ǤϤʤ���������δ���T�ȤϤɤΤ褦����������Τ�
ʬ����ʤ���GE #28��V!-V3��Ω�ɤʴ���T�ȤǤ��롥
15-15 III��aVF�˶����۾�Q�Ȥ����뤬��STE�ʤɤ��Ѳ����ʤ���Q�Ȥ���°����R��
1/3�ʾ塤�ޤ���0.03sec�ʾ�Ǥ����ͭ�٤Ȥ��롥�ĵ������ɹ��ɡ�
15-16 V1��V6���Ŷ˴ְ㤤��CRBBB�˿�ȼ����IWMI��
II,III,aVF�ΰ۾�Q�ȡ�����̤�STE��
���ȥե����� iwmi
9-13 IACD��LAE���㡤II, III, aVF��Q�ȡ��о���T��ȿž��
II,III,aVF�Ϥ��о���ȿžT�ȡ�V1-6���������оΥ��ȥ쥤��T�ȡ�
�ͻ�Ͽ�ʿST��LVH����˼��١����ɹ���
����¦�ɤ˲ä��Ƹ��ɹ��ɤ���
11-22 II, III, aVF��Q�Ȥ�������V4��V6��Q�ȡ�V1��R�Ȥ��⤯����������
���ɡ�¦�ɤι��ɤ�Ϣ³��������ɤι��ɤ��ͤ����롥transition��V1��V2��
I��q�ȤϾ����礭���۾aVL��q�Ȥ�۾�ǹ��¦�ɹ��ɡ�
V1��R�Ȥ��⤯���������Τϡ����ɹ��ɤ����ä����Ȥ���
V1,V2��J�����㲼���Ƥ��ʤ����Ȥϡ����ɤ�ST�徺���ʤ����Ȥ���
���ɹ��ɤΰ۾�Q�Ȥ�III>aVF>II�ν�˾������ʤ뤬�����¦�ɹ��ɤ�
ȯ�������I�ǰ۾�Q�Ȥ������뤿��III�Ǥΰ������ⲽ���ä���롥
aVL��Q�Ȥθ����aVL=(i-III)/2������I��Q�Ȥ���III��Q�Ȥ���������
����˾�����Q�Ȥˤʤ롥
#28
�� final p.28�ο�18�β���ϴְ�äƤ��롥
V4,V5,V6��¦�ɹ��ɤΰ۾�Q�ȤǤ��롥���ι��ɤ����ɤ˵ڤӡ�V1��V2�ι⤤
R�Ȥˤʤ롥V5,V6��S�Ȥ��ʤ����Ȥϱ��ӥ֥��å��䱦����������ꤹ��ڵ�Ǥ��롥
2018ǯ 7�� 12�� ������ 16:51:08 JST
final�β���ϴְ㤤�ǤϤʤ���������δ���T�ȤϤɤΤ褦����������Τ�
ʬ����ʤ���GE #28��V!-V3��Ω�ɤʴ���T�ȤǤ��롥
15-15 III��aVF�˶����۾�Q�Ȥ����뤬��STE�ʤɤ��Ѳ����ʤ���Q�Ȥ���°����R��
1/3�ʾ塤�ޤ���0.03sec�ʾ�Ǥ����ͭ�٤Ȥ��롥�ĵ������ɹ��ɡ�
15-16 V1��V6���Ŷ˴ְ㤤��CRBBB�˿�ȼ����IWMI��
II,III,aVF�ΰ۾�Q�ȡ�����̤�STE��
���ȥե����� iwmi
9-13 IACD��LAE���㡤II, III, aVF��Q�ȡ��о���T��ȿž��
II,III,aVF�Ϥ��о���ȿžT�ȡ�V1-6���������оΥ��ȥ쥤��T�ȡ�
�ͻ�Ͽ�ʿST��LVH����˼��١����ɹ���
����¦�ɤ˲ä��Ƹ��ɹ��ɤ���
11-22 II, III, aVF��Q�Ȥ�������V4��V6��Q�ȡ�V1��R�Ȥ��⤯����������
���ɡ�¦�ɤι��ɤ�Ϣ³��������ɤι��ɤ��ͤ����롥transition��V1��V2��
I��q�ȤϾ����礭���۾aVL��q�Ȥ�۾�ǹ��¦�ɹ��ɡ�
V1��R�Ȥ��⤯���������Τϡ����ɹ��ɤ����ä����Ȥ���
V1,V2��J�����㲼���Ƥ��ʤ����Ȥϡ����ɤ�ST�徺���ʤ����Ȥ���
���ɹ��ɤΰ۾�Q�Ȥ�III>aVF>II�ν�˾������ʤ뤬�����¦�ɹ��ɤ�
ȯ�������I�ǰ۾�Q�Ȥ������뤿��III�Ǥΰ������ⲽ���ä���롥
aVL��Q�Ȥθ����aVL=(i-III)/2������I��Q�Ȥ���III��Q�Ȥ���������
����˾�����Q�Ȥˤʤ롥
Posterior Wall AMI (PWMI) 12 Lead p.472
final p.28 ��18������ECG�ζ���ͶƳ�� GE #57�Ȥ��ä���Ǥ��롥
V9��V10��Q�ȡ�ST�徺��T�ȵ�ž���ߤ��뤬��V1,V2�ǥߥ顼������Ȥ���
R�Ⱦ徺��ST�㲼�������T�Ȥˤʤ롥
�ߥ顼������Ȥ�R�Ȥξ徺��ST�㲼����������о����ζ���T�Ȥ��̣���롥
R�Ȥ�Q�Ȥε�ž���ѥ������û����졤Ω��꤬�ߤ����ؤι⤤R�Ȥˤʤ롥
PWMI��IWMI�Ϥ褯ʻȯ���롥
V1��V2��R�Ȥ��⤯����0.03�ðʾ�ʤ�ͭ�긫�Ǥ��롥V1���V2�����������˸���롥
final p.51 ��23��
II, III, aVF�����狼���鲼�ɹ��ɤϤʤ���I, aVL�˾�����r�Ȥ����ꡤ�ޤ�SET��
�ʤ����顤���¦�ɹ��ɤϽ����Ǥ��롥�����Ѱ̤λͻ����Ṳ̋Ǥ��롥
V1-V3��STD�Ǹ��ɹ��ɤΥߥ顼������Ǥ��롥V4-V6��R�Ȥ�����ϸ���줺��
PRP�Ǥ��롥V7-V9�Ͼ�����QS�ѥ������STE�Ǥ��롥
11-22�ϲ��ɡ�¦�ɡ����¦�ɤ˲ä��Ƹ��ɹ��ɤ�.
15-28 ������V1��V4�ޤǤι⤤R�ȡ�ST�㲼�Ⱦ����T�ȡ�
���ɹ��ɤϤʤ�����Ω�������ɹ��ɡ�����R�Ȥ�V2���Ǥ�⤯V6���Ǥ��㤤��
�����γ�ư���Ѥθ����ȹͤ���Ф褤��avR��qR�Ǥ��롥����Ū�˱�����ư��
ͥ�̤ˤʤäƤ��롥
 ECG 15-28
15-29 II,III,aVF��Q�Ȥ�V1V2��R�Ⱦ徺���Ť����ɸ��ɹ��ɡ�
ECG 15-28
15-29 II,III,aVF��Q�Ȥ�V1V2��R�Ⱦ徺���Ť����ɸ��ɹ��ɡ�
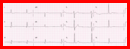 ECG 15-29
GE #57 V1��V3�ޤ�RS�ǹ⤤T�ȡ�V4��V6�˽��ä�R�ȤϾ�����V6��QS��STE��
�ߤ����Ȥ�̵���ȷ����������硩�ͻ����Ű̡�
���ɤ�AMI��V1��R�Ȥϸ��ɹ��ɤΤ��ᡤ�⤷���ɹ��ɤ�STE��ȯ������
�ޤǤδ֤Ǥ���С�V1��V3�ޤǤΥߥ顼STD��ȯ�����ʤ���V5��V6��STE��
������AMI����II,III,aVF���Ѳ��Ϥʤ����鱦��ư̮�����
���äơ��������ޤ��ĺɤˤ��¦�ɸ��ɹ��ɰʳ��˹ͤ����ʤ���
���ޤ�GE #57
���Ʊ�����ſޤΥȥ�ߥ�.
ECG 15-29
GE #57 V1��V3�ޤ�RS�ǹ⤤T�ȡ�V4��V6�˽��ä�R�ȤϾ�����V6��QS��STE��
�ߤ����Ȥ�̵���ȷ����������硩�ͻ����Ű̡�
���ɤ�AMI��V1��R�Ȥϸ��ɹ��ɤΤ��ᡤ�⤷���ɹ��ɤ�STE��ȯ������
�ޤǤδ֤Ǥ���С�V1��V3�ޤǤΥߥ顼STD��ȯ�����ʤ���V5��V6��STE��
������AMI����II,III,aVF���Ѳ��Ϥʤ����鱦��ư̮�����
���äơ��������ޤ��ĺɤˤ��¦�ɸ��ɹ��ɰʳ��˹ͤ����ʤ���
���ޤ�GE #57
���Ʊ�����ſޤΥȥ�ߥ�.
���ɹ��ɤ�ȼ�ä�ȯ�����롥
I, aVL�Υߥ顼���̤ˤ��ST�㲼��
GE #52 �������ɤβ�ǽ�����⤤��
final p.49,
12 Lead p.468
���ɹ��ɤ�ȼ������STE��II���III���⤯���ޤ���V1��STE��V2��STD��
���V3������STE���⤤�ȱ������ɤ�ͤ��롥
14-12 hyperacute AMI��V1��V3�˾�����r�Ȥ������롥���ɱ������ɡ�
14-20 IWMI������·������III��STE��������V1��ST���������ǤäƤ��롥
V2��STD��V3��STD��������ľ����T��ʿó��15-26�˻��Ƥ��롥
15-25 II,III,aVF�ΰ۾�Q��STE��v2���濴�Ȥ���STE���������ȷ���
�褯�����V1��V3��r�Ȥ�¸�ߤ��롥I,aVL��STD��T��ȿž��
15-26 I,aVL��STD��II�ξ�����STE��Q�Ȥ⾮������III���礭��Q�Ȥ��礭��STE��
aVF��Q�ȤϾ��������礭��STE��V1��V3��STE�Ǥ��뤬��V2��STD����
������STE���Ƥ��롥
15-26 I,aVL��STD��II���Ѳ��Ͼ��ʤ���III��STE��aVF�Ͼ�����Q�Ȥ�STE��
V1��STE��������ˤ⸫���롥V2��V5�ޤ����Ǥä�ST�������ȡ�
�����RVI�ο��Ǵ��ˤʤ�����¦ͶƳ�Υǡ����dz��ꤹ�롥
l2 Liead p.458.
����ư̮�ܴɤι��ɤ�ȯ�����롥
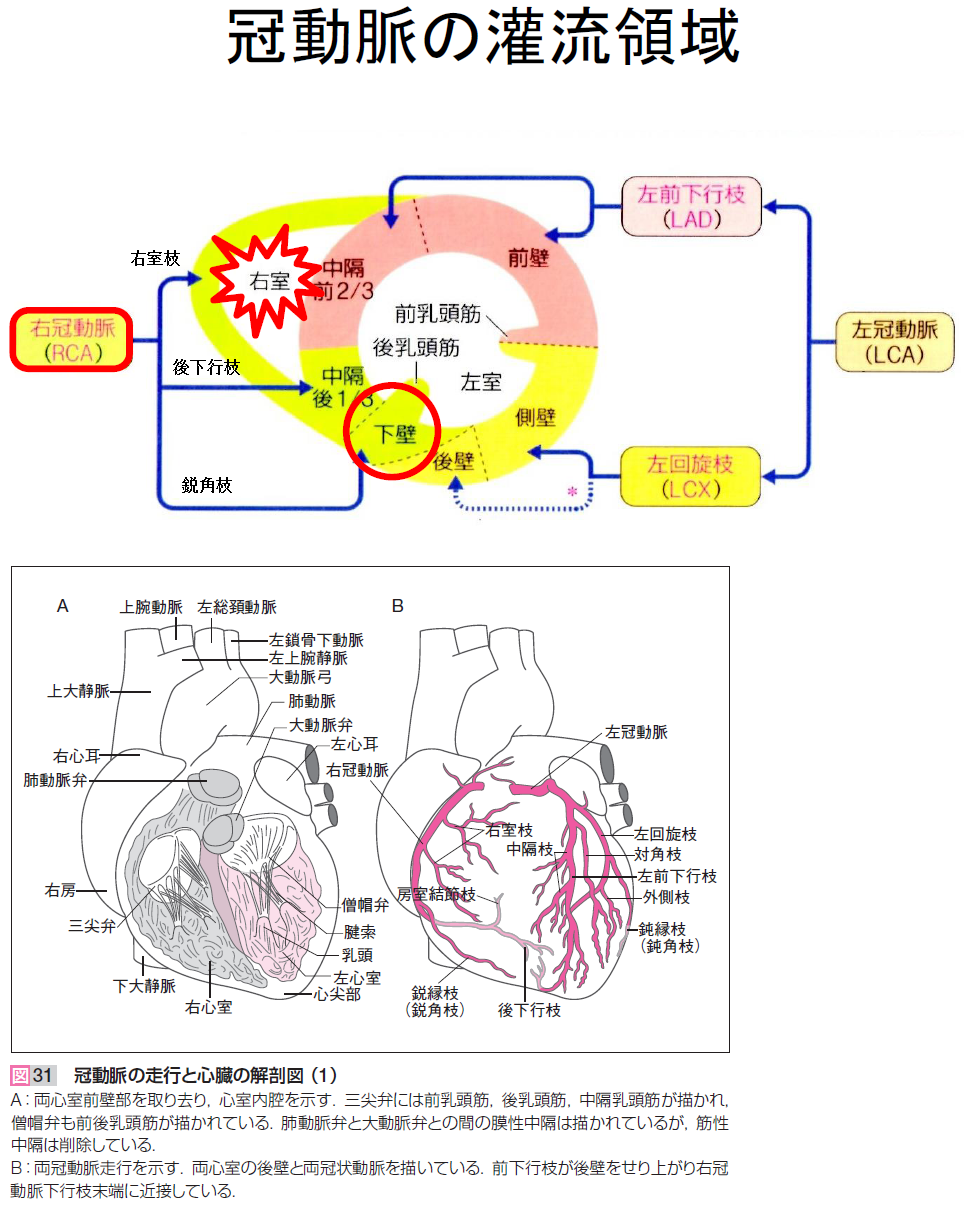
II,III,aVF,V3,V4,V5,V6,������I,aVL�˱ƶ����롥
II,III,aVF�ϱ���ư̮�岼�Իޡ�
V3,V4�Ϻ���ư̮�����Իޡ�
V5,V6�Ϻ���ư̮�����Իޤ��гѻޡ�(¦�ɹ���)
final p.62���. coronary.png
 15-22
���������ɡ�I��II��III��STE��aVR��STD��aVL�Ͽ�ʿ��V1��STD��V3-6�ޤǶ��٤�STE��
15-22
���������ɡ�I��II��III��STE��aVR��STD��aVL�Ͽ�ʿ��V1��STD��V3-6�ޤǶ��٤�STE��
 15-23
���������ɡ�I�Ϸ��٤�STE��II��III��STE��aVR��STD��aVL��ȿžT�ȡ���V1�����V2-6�ޤǶ��٤�STE��
15-23
���������ɡ�I�Ϸ��٤�STE��II��III��STE��aVR��STD��aVL��ȿžT�ȡ���V1�����V2-6�ޤǶ��٤�STE��
R�Ȥ��������� (poor r progression/reversed r progression)
 ���ޤ�LAFB�ˤ��PRP��ȯ�����Ƥ��뤬��V2��V5�ǤΥΥå���IVCD����
IVCD GE #243
���ޤ�LAFB�ˤ��PRP��ȯ�����Ƥ��뤬��V2��V5�ǤΥΥå���IVCD����
IVCD GE #243
���ɸ�2W���äƤ�STE�����ʤ���п�����Ǥ��롥�̾�V5��V6
��STE�Ϥʤ���T�Ȥϵ�ž���롥
���ɿ�����
 ���ɿ�����1
GE #328��ꡧ
���ɿ�����2
���ɿ�����
���ɿ�����1
GE #328��ꡧ
���ɿ�����2
���ɿ�����
ECG library A-Z
HCM
���������緿���ھ�(�����ɸ���)
���ھɿ��ť����ɥ饤��(2018ǯ������)
���֤���ˡ�
1957ǯ��Brigden����ŷ��������ɡ����졤��찵���Ѳ����ʤ��ƿ����硤����ĥ��������ھɤȤ���������ή��ϩ������ȯ����������Ȥ�����ȯ���������ư̮�۲������� idiopathic hypertrophic subaoric stenosis (IHSS)�����緿�ĺ������ھ� hypertrophic obstructive cariomyopathy (HOCM)����̾���Ĥ���줿�����θ塤ή��ϩ�����Ͽ�����֤ΰ۾�����ˤ����Ū�Ѳ��Ǥ���ȹͤ���졤���緿���ھ� HCM�����夷�������ھɤ�ʬ��Ȥ��Ƥϡ�
1����ĥ�����ھɡ�dilated cardiomyopathy; DCM)��
2�����緿���ھɡ�hypertrophic cardiomyopahy; HCM)��
3����«�����ھɡ�restrictive cardiomyopathy; RCM)��
4��������̮���������ھɡ�arrhythmogenic right ventricular cardiomyopathy�ˡ�
5��ʬ����ǽ�ο��ھɡ�unclassified cardiomyopathy) ��
6. ���꿴�ھɡ�specific cardiomyopathies�ˤȤʤ롥
������ʬ�Ұ����ؤο���ˤ�꼡���ȿ��ھɤ��°������Ұ۾郎Ʊ�ꤵ��Ƥ���8�ˡ�9�ˡ�HCM �ǤϤ���ޤǤ˿��ڦ¥ߥ�����ź������ڥȥ��ݥ˥�T�����ڥߥ�����������C�ʤɤξ��ʤ��Ȥ�10��Υ��륳�ᥢ�ʴ�Ϣ�˰����Ҥ�200�ʾ�������Ѱۤ���𤵤�Ƥ��롥��ĥ�����ھɤǤ⥢���������ȥ��ե���ʤɤΰ����Ұ۾郎�ߤ��뤳�Ȥ���𤵤�Ƥ��ꡤ���ھɤϤ�Ϥ�ȸ��������ʿ��ڼ����ɤȤϤ����ʤ��ʤä������Τ褦�ʿ������WHO/ISFC ��Ʊ�Ѱ������Ƥ�1995ǯ�˲������줿��
���緿���ھ�
���������ĺ������ھ�
��ĥ�����ھɤʤ�Ӥ˴�Ϣ�����������ھɤο��Ť˴ؤ��륬���ɥ饤��
��ꡥ
��ĥ�����ھɥޥ���
��ĥ�����ھɥߥ���
��ȯ�����ھɤ��֤��뿴������ʼˡ�����������Ū��Ƥ
��ĥ�����ھɤο��ſޤ���ħ��
����ĥ�����ھɤ��ð�Ū�ʿ��ſ긫�Ϥʤ����������ʤ��顤���ڤ����ݲ�����˼�����γ�ĥ���ɷ���Ƴ�Ϥξ㳲������������ͳ�褹���ȷ��Ѳ�������̮��ǧ����롥�ä˺����γ�ĥ�����ݲ����ʹԤ���ȡ��������Ű̢���������ʳ���ˡ�r �ȸ�����ä�V1����V3 ͶƳ��poor r progression�ˡ��۾�Q�ȡ�QRS����Ĺ����¦����ͶƳ�ˤ�����VAT��Ĺ�� �ӻޥ֥��å��� ������֥��å��� ST-T�Ѳ��ʤɤ��и����롥�����γ�ĥ������˿ʹԤ���ȡ�QRS����0.12�ä�Ķ�������ӥ֥��å��긫���褹�뤬�������ȷ��Ϻ��������ȼ��ʤ�������κ��ӥ֥��å��ȤϰۤʤꡤQRS�Ȥ�ʣ����notch��ޤ�褦�ʰ۾���ȷ����������κ��ӥ֥��å��ˤȤʤ롥�ޤ������������ݲ������٤˿ʹԤ���ȡ������ε����Ϥ��㲼�ü����ơ���¦����ͶƳ��R�Ȥ������˸��⤷��S�Ȥ����Τζ���ͶƳ�ȷ����ʱ��ӥ֥��å��������ˤȤȤ�ˡ��ͻ�ͶƳ�����Ű̲�����褦�ˤʤ롥�����������γ��硤����٤�������ȱ�¦����ͶƳ��T�Ȥ���ž���������줬��������ˤʤ��V4��V5ͶƳ�ޤ�T��ž���ȵڤ��뤬��Ʊ���˺������礬¸�ߤ���ȡ������Ѳ�����Ω���ʤ��ʤ롥
����˼��˼���ۤε�ή�亸����ĥ�������ξ徺��ȼ�äƳ�������ݲ���������P�����α�Ĺ�亸˼��ٽ긫���褷����˼���������̡���˼��ư��AF�����ο�˼������̮���и����Ƥ��롥�����������̤⿴��ǽ���㲼�ȤȤ��¿ȯ����褦�ˤʤꡤϢȯ��¿�����������̤�и����롥
����ĥ�����ھɤǤϼ�Ȥ��ƺ��������Ѥ�ͭ���뤿�ᡤ�����������̤��ȷ��ϱ��ӥ֥��å����褹�뤳�Ȥ�¿�����������륳���ɡ���������ִ��������Ѥ�ȼ�����ϡ����ӥ֥��å��ʤޤ��Ϻ��ӥ֥��å��ˡܲ��������δ������̢����������VT�ˤ������롥��
�����������֤Ǥϳ�����̮�Ȥʤ뤬�����κݤ�P�ȷ����۽�����˼�������Ƥ������ƶ���ᵯ����I��II�� IIIͶƳ��P�Ȥ������ˡ���̲���100/ʬ��Ķ����ƶ��̮���褷�Ƥ�����ϡ� ��˼�������Ŭ��ƶ��̮��inappropriate sinus tachycardia�ˤ˴�Ť���̮Ͷȯ�����ھɤ�32�ˡ����ڤ������ˤ��ɷ���Ƴ�Ϥ����������ȡ�I��III��˼���֥��å��������뤬�������륳���ɡ������Ǥ��½������˼���֥��å���ȼ���䤹��33�ˡ���12 ͶƳ���ſޡ���٥�4a�����졼��A��
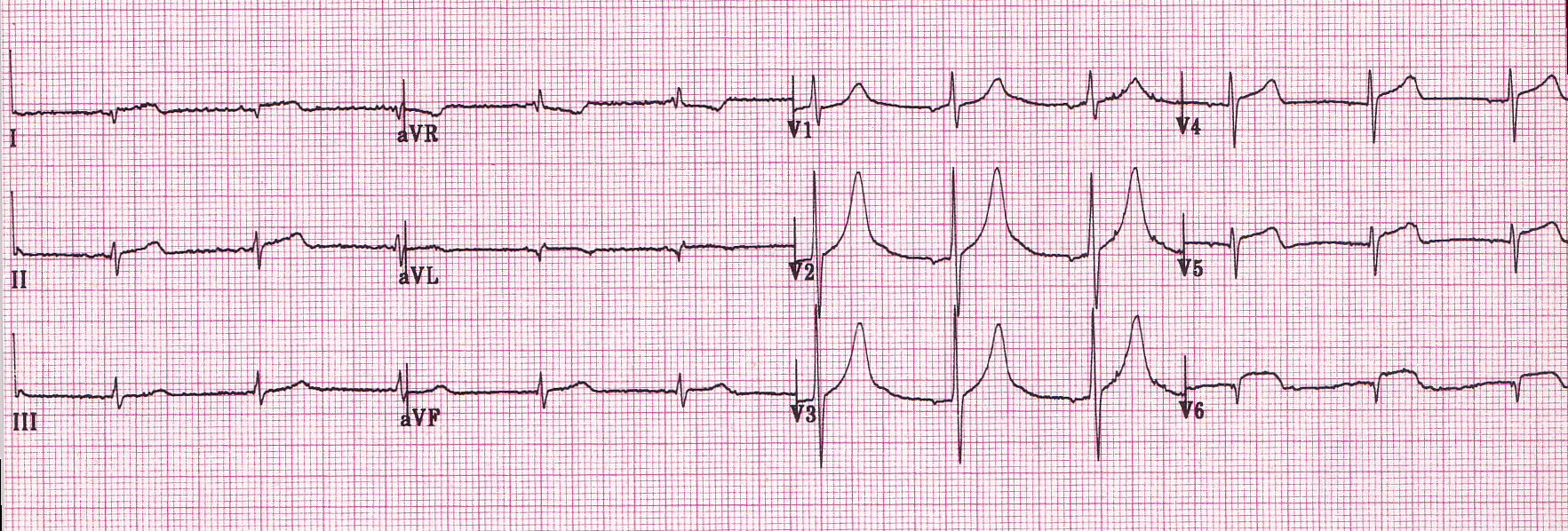
��ĥ�����ھ�1
V2��S�� > 35mm������LVH�������а̤�����ξ�������硤LAE��II��P�Ȥ��⤯RAE��
V5,6��R�Ȥ��㤤���Ȥ��麸�����ڤϳ�ĥ�ȹͤ��롥ST����Ĺ�����Ȥ����л��֤α�Ĺ���ͤ����롥��̤Ȥ���QTC�ϰ۾��Ĺ���ʤ롥
��ĥ�����ھ�2
ŵ��Ū��LVH�ѥ�����V1��P�Ȥ�RAE��LAE�������롥RVH�ν긫�Ϥʤ������������ξ�������礬��ǧ���줿��QTc��Ĺ����
��ĥ�����ھ�3
�����а̤Ⱥ������硥QRS���Ϲ���CLBBB�ͤǤ��뤬��V6�˾�����q�Ȥ����뤿�����Ƴ�ٱ�(IVCD)�Ǥ��롥���ߤ���ST�������Ȥϥ��ȥ쥤�������ꥹ���̤�������
��ĥ�����ھ�4
Af����LBBB��VT��DCM�Ǥ褯�����롥�ɤ������R on T��VT�ǤϤʤ���AF�ˤ����̮�Ǥ��롥
���緿���ھɤο��Ť˴ؤ��륬���ɥ饤��(2007)
���緿���ھɥޥ���
���緿���ھɥߥ���
dagger.png
dagger2.png
dagger3.png
apical.png
apical2.png
apical3.png
apical4.png
HCM���̾����֤������ȯ���������줬����ή��ϩ�ˤޤ��ȵڤ�����ĺ������緿���ھ�(HOCM 25%)�Ȥ�֡��ü�ʷ��Ȥ��ƺ�����ͳ�ɤ����礬�ڤ֤ȿ��������ĺ������ھ�(20%)����֤ǤϤʤ������������礹��ȿ��������緿���ھ�(10%)�Ȥ�ӡ����̥������ͤ�¿����
��HCM ����Ⱦ���˾���������ͥ�������β�²��ȯ�ɤ��ߤ��롥��ȯ���HCM �Τʤ��ˤϤȤ�櫓���������緿���ھɤ�¿���ޤޤ졤HOCM �Ͼ��ʤ��� C���αꥦ���륹��HCV�ˤ�HCM �θ����Ȥ��ƽ��פǤ��뤳�Ȥ���������Ƥ���29�ˡ� HCM �Ǥϳ�ĥ�����������֤ǡ�����ǽ�ϰ���Ū�ˤ��ݻ�����Ƥ���56�ˡ�67�ˡ�
������ή��ϩ���� HOCM �ϡ�HCM ���Τ���25�����٤Ȥ���Ƥ���75�ˡ����оɾ��˶��ˤ�¿������������ ���˻����� HCM ���Ԥ��Ф��Ƥ϶ش����Ǥ��ꡤ���ˤ��Ф��Ƥ�Ŭ�ڤʿ��Ǥ�ɬ�פǤ��롥ưة������̮����̮�����Ƽ����Ϥ�����ʤɤ�ǧ����롥
���̾�HCM ���ԤǤϾ弼�����뤤�Ͽ���������̮�ˤ��ưة��¿�������ʤ餺��ȯ������˼��ư���³����˼��ư�Τ����ưة�⤢�ꡤ�ۥ륿�����ſޤʤɤ�Ŭ�ڤ�������ο��Ǥ�ɬ�פǤ��롥
���������Ṳ̋����٤ϡ���ǯHCM �Ǥ��㤯121)��������ԤǤϹ⤯�ʤ�122)��
ii�˰۾�Q �Ȥʤ�Ӥ������Q �Ȥξü����۾�Q �Ȥϡ�����HCM ����Ⱦ����121)�����ͤ�25��31���ǧ�����80)��117)���۾�Q�ȷ����ˤϡ���֤��Զ���������ȿ���������2 �Ĥ���������¬�����127�ˡ����Ԥ����о����������ˤ�����٥��ȥ���ԶѹդǤ��ꡤ���ζ�������Q �Ȥ��������֥٥��ȥ뤬�����鱦�����˸��������ˤ�V5,6 �ˡ����������Ǥ����II��III��aVF ��Q �Ȥ���������롥��֤˸¶ɤ�����ǯ������ǰ۾�Q �Ȥ����٤��⤯117�ˡ����礬������ͳ�ɤؿ�Ÿ���뤫����֤ο��ڤ����ݲ���������С���֥٥��ȥ������Ū�����ˤ�ꡤQ �Ȥϸ��⤷��HCM ��15��ǤϾü����롥�ޤ������������緿���ھɤ䱦��������Ǥϡ��۾�Q �Ȥ�ȼ��ʤ�128�ˡ�����Ԥϡ����ڤ����������ݲ��ˤ��ɽ�ε����Ͼü��Ǥ��ꡤR�Ȥθ���ȤȤ�˿����ʰ۾�Q �Ȥ��и����롥����Q �Ȥ����������Ȥ�¿����V4-6 ͶƳ�ˤߤ��롥 D-HCM (dilated phase of hypertrophic cardiomyopathy: ��ĥ�����緿���ھ�)��¿����
iii)����¾��QRS �۾�
�����а̤�20��30���ǧ���졤�����а̤�¿������������Ƴ�㳲�ϻɷ���Ƴ�Ϥξ㳲��ȿ�Ǥ��롥15���WPW�ɸ����ʤɿ��������ʳ����ʻ��129��-131�ˡ�����������θ����Ȥʤ�130�ˡ�
b��ST-T �Ѳ�
��ST���ߤȱ���T�Ȥ�70�� 95���ǧ����롥�����Ȥ��Ƥϡ����������ȼ�������첼���ڤ�����Ū���ڵ��졤���翴�ڤκ�ʬ�˲������ٱ��ȼ���켡���Ѳ���æʬ�˲������Ѳ���ȼ�������Ѳ��ʤɤ���¬����롥���ȥ쥤��ѥ�����¿�������㲼�����٤���������٤���ؤ��ʤ���
�����������緿���ھɤǸ����뺸¦����ͶƳ�ι��Ṳ̋�ȼ�����籢��T�Ȥ�V3 �� 5���濴�ˡ�1.0mV�ʾ���о����������Ф���ST���ߤ��132�ˡ���������������٤������ۤɿ����ʤ�133�ˡ����������緿���ھɤ�70 ��Ǥϡ����Ṳ̋���籢��T�ȤϷв�ȤȤ�˸������ü���124�ˡ����θ��������翴�ڤ����������ݲ���ȼ��������Ѳ��ȹͤ����롥
�����ˡ���¦����ͶƳ��II��III��aVF�����뤤��I�� aVLͶƳ�ˡ�R�Ȥθ�������ι����۾�Q �Ȥ�ȼ��ST �徺��ǧ��뤳�Ȥ����ꡤ���������οʹԤ���¬����� 134�ˡ�D-HCM �俴�����������ʻ��ˤ��Ф��Фߤ��롥
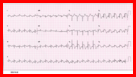
���緿���ھ�1 Dagger-like Q Waves
���緿���ھ�2 Giant T wave inversion
���緿���ھ�3 Classic HCM with asymmetrical sptal hypertrophy
���緿���ھ�4 ���Ʊ���̤���
���緿���ھ�5
���緿���ھ�6
���緿���ھɥ�����
���緿���ھɥ�����3
���緿���ھɥ�����2
���緿���ھɥ�����4
���緿���ھɥ�����5
���緿���ھɥ�����6
12%��WPW��PR�ֳ֤�����Ǥ��롥
memo
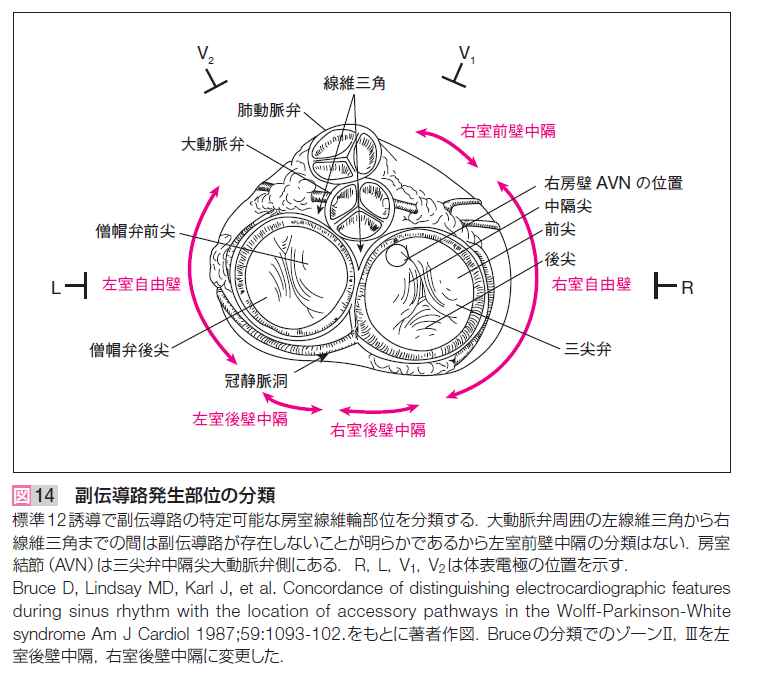
����Ƴϩ�ΰ��֤Ϻ�����ͳ�ɤ��Ǥ�¿��55%��
�Ĥ��Ǹ�����֤�33%��������ͳ�ɤ�9%��
����������֤�3%����𤵤�Ƥ��롥
(Wellens: p.80)
GE #305��
�츫V1��LBBB��V6��RS�Ȥ�����IVCD�Τ褦�˸����뤬��V6��S�Ȥϥ��㡼�פǤ��롥
�������äơ�RBBB��V6�ǤϤʤ���PQû�̻ͻ�ͶƳ�Φ��Ȥ���B����WPW�Ǥ��롥
��Ƴ���̤�(3A)����������֤ˤʤ롥
���ǡ�final p.97.
 IMG_20170912_0002.pdf
IMG_20170912_0002.pdf��GE #190�������������ʤ�����
III��aVF�Υǥ륿�Ȥϥǥ륿�ȤǤϤʤ���
P-Rû�̤ǰ۾�Q�Ȥ�WPW�ɸ����ȴְ㤨�ʤ��褦�ˤ��ʤ���Фʤ�ʤ���
(12 Lead p.137���)
Type A:
V1�Ǿ�������ȡ����Ƥζ���ͶƳ��R�Ȥˤʤ롥����(Kent«)������Ƴϩ�����뤫��
���ӥ֥��å����˻��롥
Type B:
V1�Dz��������ȡ���¦����ͶƳ�Ͼ������R�Ȥˤʤ롥����������Ƴϩ�����뤫��
���ӥ֥��å����˻��롥
GE #186: �ַ�WPW��
Type C:
V1����V4�ޤǤϾ������V5, V6�ϲ�����S�ȡ����Ǥ��롥
Type B��II, III, aVF�α������ȤϿ��ڹ��ɤΰ۾�Q�Ȥȴְ㤨�䤹����
pseudoinfarct�Ȥ����Ƥ��롥Type A�ι⤤R�Ȥϸ��ɹ��ɤȴְ㤨�䤹����
IVCD�ȴְ㤦WPW��
GE #305 PQû�̡�IVCD��
���ǡ�WPW��V4-6��S�Ȥ�����Ǥ��ꡤIVCD������Ǥ��롥
��ʳ��Kent«���鿴�������ꡤ�չ�����AV node���䤹�뿴�������
antidromic�Ȥ�Ф�롥wide-complex tachycardia��VT�ȶ��̤Ǥ��ʤ���
����Ǥ��롥�ޤ�AF��Af�Ȥ�1:1�б������郎�ᤤ��
�դ�AV node����Kent«�˸������롼�פ�orthodromic�Ȥ�Ф�롥
������Ƴ�Ǥ��뤫��narrow-complex tachycardia�Ǥ��ꡤ�����٤��㤤��
AV node���ٱ䤬Ư������Ǥ��롥������٤���
����̮ƶ����˹�ۤ���¦�����Ԥ�������������֤˰��֤��롥
���Τ���ˡ�����̮ƶĴΧ��WPW����Ƴϩ�Ϻ�����������ն�ȹͤ����롥
wpw2.png
IMG_20170912_0002.pdf
IMG_20170912_0002.pdf��GE #190�������������ʤ�����
III��aVF�Υǥ륿�Ȥϥǥ륿�ȤǤϤʤ���
P-Rû�̤ǰ۾�Q�Ȥ�WPW�ɸ����ȴְ㤨�ʤ��褦�ˤ��ʤ���Фʤ�ʤ���
(12 Lead p.137���)
Type A:
V1�Ǿ�������ȡ����Ƥζ���ͶƳ��R�Ȥˤʤ롥����(Kent«)������Ƴϩ�����뤫��
���ӥ֥��å����˻��롥
Type B:
V1�Dz��������ȡ���¦����ͶƳ�Ͼ������R�Ȥˤʤ롥����������Ƴϩ�����뤫��
���ӥ֥��å����˻��롥
GE #186: �ַ�WPW��
Type C:
V1����V4�ޤǤϾ������V5, V6�ϲ�����S�ȡ����Ǥ��롥
Type B��II, III, aVF�α������ȤϿ��ڹ��ɤΰ۾�Q�Ȥȴְ㤨�䤹����
pseudoinfarct�Ȥ����Ƥ��롥Type A�ι⤤R�Ȥϸ��ɹ��ɤȴְ㤨�䤹����
IVCD�ȴְ㤦WPW��
GE #305 PQû�̡�IVCD��
���ǡ�WPW��V4-6��S�Ȥ�����Ǥ��ꡤIVCD������Ǥ��롥
��ʳ��Kent«���鿴�������ꡤ�չ�����AV node���䤹�뿴�������
antidromic�Ȥ�Ф�롥wide-complex tachycardia��VT�ȶ��̤Ǥ��ʤ���
����Ǥ��롥�ޤ�AF��Af�Ȥ�1:1�б������郎�ᤤ��
�դ�AV node����Kent«�˸������롼�פ�orthodromic�Ȥ�Ф�롥
������Ƴ�Ǥ��뤫��narrow-complex tachycardia�Ǥ��ꡤ�����٤��㤤��
AV node���ٱ䤬Ư������Ǥ��롥������٤���
����̮ƶ����˹�ۤ���¦�����Ԥ�������������֤˰��֤��롥
���Τ���ˡ�����̮ƶĴΧ��WPW����Ƴϩ�Ϻ�����������ն�ȹͤ����롥
wpw2.png
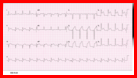
 ����̮ƶĴΧ�ˤ��WPW�ȷ�
2018ǯ12��22��(ECG4.doc)���
����� 80��P�� 118, QRS�� 77, T�� 85
wpw3.pdf
����̮ƶĴΧ�ˤ��WPW�ȷ�
2018ǯ12��22��(ECG4.doc)���
����� 80��P�� 118, QRS�� 77, T�� 85
wpw3.pdf
concordant ����������
discordat ����������(��ž��ȿž)
�Ǹ��QRS��������discordant������Ǥ��ꡤconcordant�Ǥϵ����Ѳ��Ȥߤʤ���
RBBB�����IRBBB�Ǥ�S�Ȥϲ�����������������T�Ȥˤʤꡤ����ȶ��̤Ǥ��ʤ���
final p.86
�ٹ���
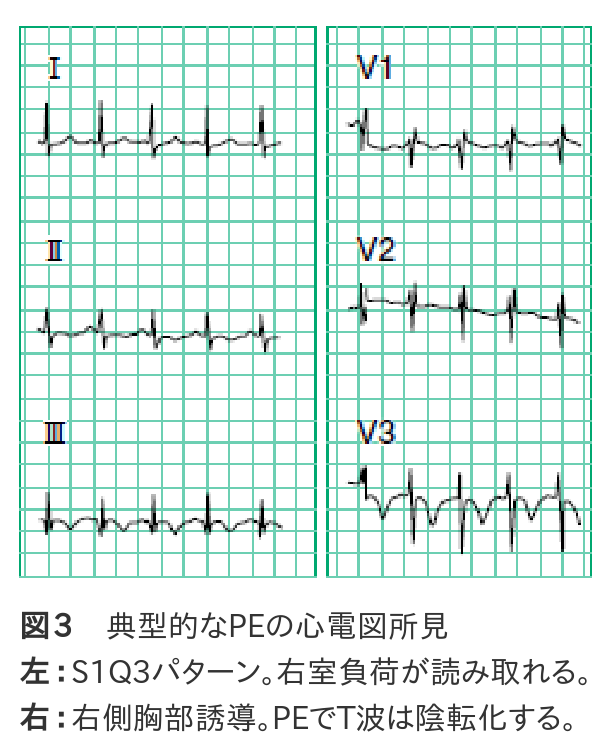 ����PE�ο��ſ긫�Ǥϡ�������S1Q3�α�����٥ѥ�����ʿ�3���ˤ�ͭ̾�Ǥ�����
�ߤ��������٤�30��ʲ��Ǥ���������ž��٤ȤϤ��ޤ���ؤ��ޤ���
�¤ϡ�������ⱦ¦����ͶƳ��V1-3�ˤ�T�Ȥ��Ѳ��Τۤ���ͽ���褯ȿ�Ǥ��ޤ��ʿ�3���ˡ�
��������ǰ�ʤ��顤����������ˤˤߤ�����긫�ǤϤ���ޤ���
McGinn-White��pattern�Ȥ�S1Q3T3�ο��ſޤ���
II��III�α���T�Ȥϲ��ɤε���긫��Ʊ����
V1��V3�α���T�Ȥ�������������T�Ȥ�����Ǥ���Τ�
���餫�˰۾�Ǥ��롥
T�٥��ȥ뤬�����˸������긫�Ȥ����Ƥ��뤬��
�������ڤγ�ĥ�������ȼ��������¦���ڤ������ʬ��
�ˤ��۾�ȹͤ��롥
PE�Ǥϱ�����ĥ���뤬����������ˤϤʤ�ʤ������Τ���V1��R�ȤϾ�������
V1��rSR'�ϱ�������Ǥⶦ�̤���긫�Ǥ��롥V6��S�Ȥơ��������ޤ����
���ӥ֥��å��ǤϤʤ���S1��S�Ȥ�����������
BB p.76, fig7.19 �ٹ��ɡ�S1Q3T3��I��rS�ˤ�뱦���а̡�V1��qR�ޤ���rR'��V6��RS�����ײ�ž��
����PE�ο��ſ긫�Ǥϡ�������S1Q3�α�����٥ѥ�����ʿ�3���ˤ�ͭ̾�Ǥ�����
�ߤ��������٤�30��ʲ��Ǥ���������ž��٤ȤϤ��ޤ���ؤ��ޤ���
�¤ϡ�������ⱦ¦����ͶƳ��V1-3�ˤ�T�Ȥ��Ѳ��Τۤ���ͽ���褯ȿ�Ǥ��ޤ��ʿ�3���ˡ�
��������ǰ�ʤ��顤����������ˤˤߤ�����긫�ǤϤ���ޤ���
McGinn-White��pattern�Ȥ�S1Q3T3�ο��ſޤ���
II��III�α���T�Ȥϲ��ɤε���긫��Ʊ����
V1��V3�α���T�Ȥ�������������T�Ȥ�����Ǥ���Τ�
���餫�˰۾�Ǥ��롥
T�٥��ȥ뤬�����˸������긫�Ȥ����Ƥ��뤬��
�������ڤγ�ĥ�������ȼ��������¦���ڤ������ʬ��
�ˤ��۾�ȹͤ��롥
PE�Ǥϱ�����ĥ���뤬����������ˤϤʤ�ʤ������Τ���V1��R�ȤϾ�������
V1��rSR'�ϱ�������Ǥⶦ�̤���긫�Ǥ��롥V6��S�Ȥơ��������ޤ����
���ӥ֥��å��ǤϤʤ���S1��S�Ȥ�����������
BB p.76, fig7.19 �ٹ��ɡ�S1Q3T3��I��rS�ˤ�뱦���а̡�V1��qR�ޤ���rR'��V6��RS�����ײ�ž��
transiton �ܹ��� R/S�椬1�ξ�ꡥp.219
����ʤ�V3��V4�δ֤ˤ��롥
�ܹ��Ӥ�
V1�˶�Ť���ȿ���ײ�ž(counterclockwise rotation)��
V6�˶�Ť��Ȼ��ײ�ž(clockwise rotation).
��ü�ʻ��ײ�ž��ecg 9-11�Ǹ����롥
������
�����ϱ��Ф������˰��֤��롥�����Ϻ�˼����ư̮�˸��ꤵ�졤��ư���ˤ���
���֤Ǥ��뤬�������Ͽ�����ȶ��˱�¦���˰�ư�Ǥ��롥
�������äơ�ȿ���ײ�ž���ưפ�ͭ�����롥
�ܹ��Ӥ�V1��V2�ʤ�ȿ���ײ�ž�����R�Ȥ��⤯�ʤꡤ�������硤���ɹ��ɤ��θ���롥
ecg 11-22��
���ײ�ž��
�������硤
V1��R���������Ƥ�ȯ�����뱦������(MS, PH, COPD, PE)��
ξ�����硥
ALFB
pectus exavatum(ϳ�Ͷ�)
��¡����ʿ�̤ˤʤ��ȿ����������ž(good R progression, early transition)��
�������䤹����V1��r���礭���ʤ롥
 I��aVF��II��aVF�ϻ��Ƥ��롥
S1S2S3�����꼴�ˤʤ롥
I��aVF��II��aVF�ϻ��Ƥ��롥
S1S2S3�����꼴�ˤʤ롥
 ��¡��ȿ����������ž�����С�
V1��V6��R�Ȥ����ˤǤ롥
EMS 12 Lead
Prominent R Wave in Lead V1: Electrocardiographic Differential Diagnosis.
Mattu, Brady, et al.
Am J Emerg Med 2001;19:504-513.
Right bundle branch block
Left ventricular ectopy
Right ventricular hypertrophy
Acute right ventricular dilation
Wolff-Parkinson-White syndrome Type A
Posterior myocardial infarction
Hypertrophic cardiomyopathy
Progressive muscular dystrophy
Dextrocardia
Misplaced precordial leads
Normal variant
��¡��ȿ����������ž�����С�
V1��V6��R�Ȥ����ˤǤ롥
EMS 12 Lead
Prominent R Wave in Lead V1: Electrocardiographic Differential Diagnosis.
Mattu, Brady, et al.
Am J Emerg Med 2001;19:504-513.
Right bundle branch block
Left ventricular ectopy
Right ventricular hypertrophy
Acute right ventricular dilation
Wolff-Parkinson-White syndrome Type A
Posterior myocardial infarction
Hypertrophic cardiomyopathy
Progressive muscular dystrophy
Dextrocardia
Misplaced precordial leads
Normal variant
��ư̮�β�˶��final p.60
���̤ο��ſޤǤϣ���ͶƳ���ſޤȤ��äơ�
��¡�����������鿴�ſޤ�Ͽ�����Ǥ����ʿ��Τ��դ����Ŷˤϣ����ġ�
���Τ����� IIͶƳ��IIIͶƳ��aVfͶƳ�Ȥ�����Σ��ȡʿ�˼�μ��̤���Ȥ����ȡˤ�
�������ˤʤäƤ�����̾�Ͼ�����ˤ�Τ���̮ƶĴΧ�ȸƤ�Ǥ��ޤ���
GE #272, PR 0.13, Axis -20�롤�а��̤�V1��V2�δ֤ϰ۾NSTWC��
���ſ�II,III,aVFͶƳ�Ǥα���P�ȤǼ������չ���P��ĴΧ�ϸŤ���괧��̮ƶĴΧ��
�ƤФ�,��ŷ���������ä˺�������̮��ľ�,��̮ƶ����˼��ַ�»��,
������̮��»����ǹ����٤ˤߤ��뤳�Ȥ��Τ��Ƥ���.
�и����������������Τ���,����̮ƶĴΧ���褷���Τ�
��������̮��Ĺ�ʻ��35����7��(20.0%),��̮ƶ����˼��ַ�»��14����4��(28.6%)��
��Ψ�Ǥ��ä�.������̮��»���1��Ϻ�������̮���Ĥ��ʻ������̮ƶĴΧ�Ǥ��ä�.
�оȤȤ������������ݷ���˼��ַ�»��173���洧��̮ƶĴΧ��5��(2.9%)��
�Ȥɤޤä�.����ݷ���˼��ַ�»����νѸ忴�ſ�follow up��P���κ�������
43��(24.9%)��ǧ��,���Τ�������̮ƶĴΧ�ؤΰܹԤ�22��(12.7%)�ˤߤ�줿.
����̮�ؤΥ����˥��åȤ���Ѥ��뿴˼��ַ�»�ɽ����Ǥ�,����ˤ��ƶ�����
�㳲�ˤ��Ѹ崧��̮ƶĴΧ���������Τȹͤ���줿.
PR�� 0.12�ðʾ�Ǥ��롥
����̮ƶĴΧ (coronary sinus rhythm)
irregularly irregular ����Ū����̮
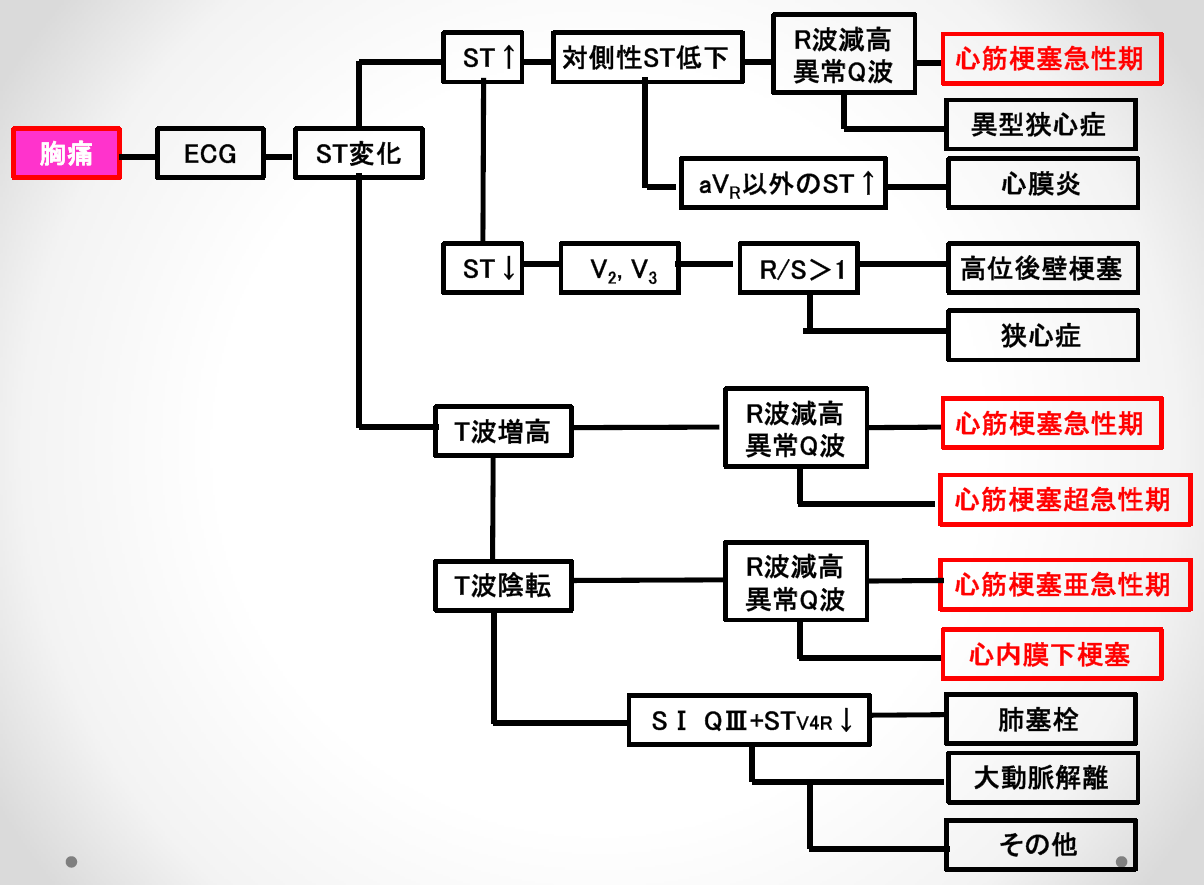
ST�徺(STE)���Ф�����¦���ڤ�ST�㲼(STD)����
T�Ȥ��Ф��Ƥ��Ѳ����ʤ�����ž�������ʤ���ñ���Ż��Ṳ̋������Ѳ��Ǥ��롥
cf. final p.52
¦�ɹ��ɡ�I,aVL��STE���Ф���II,III,aVF��STD��II���Ѳ��Ͼ��ʤ���GE #104��
���ɹ��ɡ�II, III, aVF��STE -> I, aVL��STD
�������ɡ�VR��STE ->V1, V2��STD���������������ɤ�V1,V2��STE��ͭ�����롥
�����ɤ϶������̤ˤ��뤿�ᡥ
���ɹ��ɡ�V6��V9��STE -> V1, V2��STD
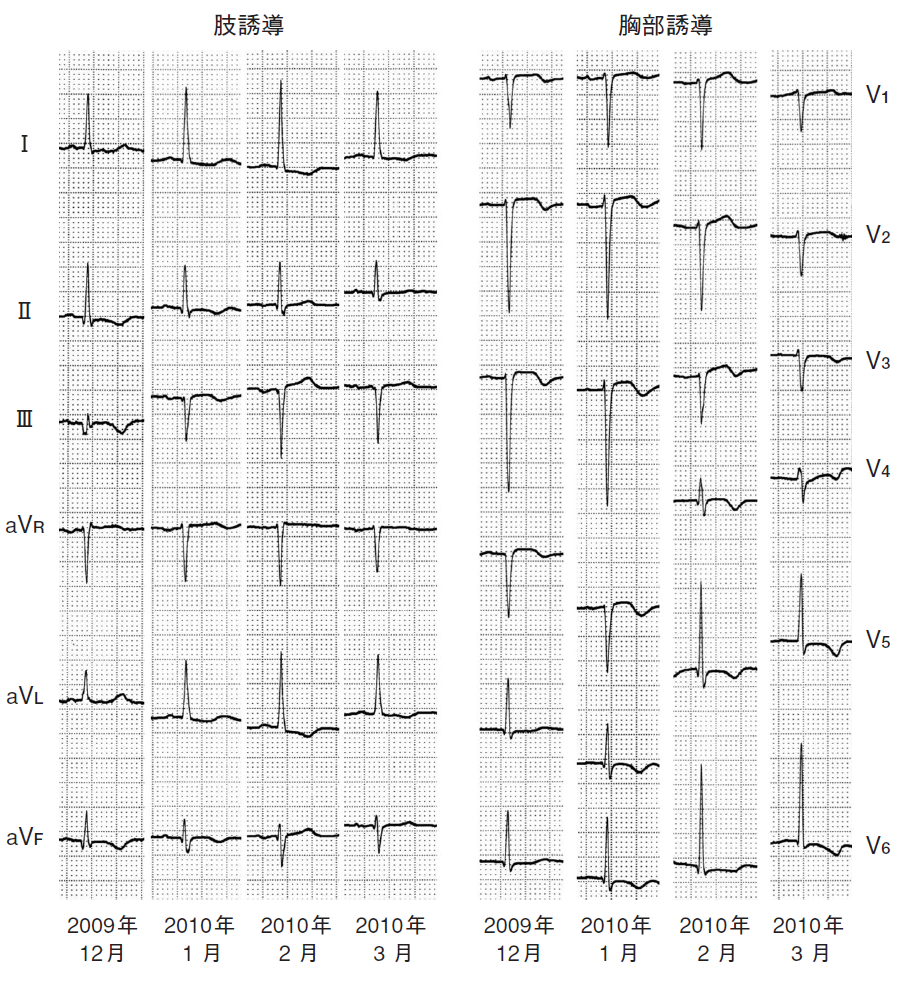
������˿��ſ긫�����ȥ쥤��ѥ�������Ѳ�����Ķ��������1��
���� Ű�����Ĺ̰�Ϻ��������˿��ſ긫�����ȥ쥤��ѥ�������Ѳ�����Ķ����������1�㡥��¡ 43:43-48, 2011.
LVH
��������ν긫�Ȥ��ƤϺ������Ű̡�QRS���֤α�Ĺ���ä�VAT�ʿ�����ʳ���֡ˤ���
Ĺ���롢ST-T�Ѳ��Ȥ��ä���Τ��Τ��Ƥ��롣�������Ṳ̋ΤߤǤϺ�������Ȥϸ�
��ʤ������礬�ʤ�ȡ�T�Ȥ�ʿó����ST���ߡ�T�Ȥα�ž����ǧ�����褦�ˤʤ롣
�����ȥ쥤��ST-T�Ѳ��Ȥ��������ȥ쥤�ǤϾ���̤�ST�㲼�Ǥ��ꡢ
��Ⱦ���ʤ��餫�Ǹ�Ⱦ����ʺ������о����α���T�ȤȤʤ롣I, aVL, V4��V6ͶƳ��
ǧ����뤳�Ȥ�¿����Ω�̿��Ǥ�I,aVL�ǤϤʤ�II,III,aVFͶƳ�ˤ������Ѳ���
ǧ����뤳�Ȥ����롣
RVH
����������ٹ�찵�ɤʤɤ�ǧ�����긫�Ǥ��롣�����Υߡ����饹�ɸ����ʤ�
�ٺ���ɤǤϽž��١�����ˡ����ꤹ�뤦���Ǥɤ����٤��ٹ�찵������Τ���
���פȤʤäƤ��뤿�ᡢ��������ν긫�����˽��פǤ��롣�����а̡�����P��
��P�Ȥι⤵��25mm�ʾ�ˡ�V1��V3��R�Ȥ����⡢VAT��0.03����0.05�á�V1��V3��
���ȥ쥤��ѥ�����I, aVL, V5, V6�ο���S�ȡ��Դ������ӥ֥��å��Ȥ��ä�
�긫���Ȥ߹�碌���ٹ�찵�����٤�ͽ¬���롣�ٺ���ɤǤϤ����ν긫��٤���
ʬ�Ϥ����80��ʾ�ξ���ǿ��ſް۾郎��Ŧ�Ǥ���Ȥ���Ƥ��롣��������ˤ�ä�
������ϰϤ��Ѳ�������פ���Ǥ��롣
���ſޤ��ɤ���
 II, III, aVF�ξ�����q�ȡ�����T�Ȥ����ա�
II, III, aVF�ξ�����q�ȡ�����T�Ȥ����ա�
V6��R�Ȥ����������������ε�ǽ�㲼�Ǥ��롥
BB fig. 10.19 (p.133)CLBBB�Ǥ�V1-V5��QS�ѥ�����V6���������������ι���R�ȡ�
���̤�CLBBB�Ϻ�����Ƴ�ٱ������QRS�ο������礭���ʤ롥
GE #57 V6��QS�ȷ���¦�ɸ��ɹ��ɡ�aVR��qR�ȷ���
GE #73 ��-60 V1-V5�ޤ�rS�ǻ����ȷ���V6��RS����S�������礭����
LAFB, QRS����0.14������,�ޤ��Υå������뤿��IVCD��
GE #121 II, aVF���ݤ����鼴��-30��ʲ���V1��PVC�Τ褦�˸����뤬�����rsR'
�Ǥ��롥V1-V3�ޤ�rsR'��ȿžT�ȡ�V4-V6��rS�Ȥ�����T�ȡ�
���ǡ�LAFB+CRBBB������RBBB�ϱ�������ο��ǤϽ���ʤ�����
V1�ΰ۾�ʹ⤵��R'��V6��S�ȡ�������ȿžT�Ȥ�RVH�碌�롥
�̾��CRBBB�Ǥ�V6��R�Ȥ�������S�ȤǤ��뤬��RVH�Ǥ�R�Ȥ���������
S�ȤϱԤ�������
GE #196 ��90�ʾ塤����P�ȡ�V1��rsR'�Ǥ��뤬��rs�����˾�������R'�ϥ��㡼�פ�
�̾�α��ӥ֥��å��Ȱۤʤ롥V2��V6�ޤǤ϶������ζ���S�ȡ����ӥ֥��å�
�Ǥ����S�������������顤���������鸫�Ƥ�RBBB�Ȥϰۤʤ롥V1��
����T�Ȥǡ�V2��ʿó��V3-V6���̾��T�ȡ�R�Ȥ�V3���Ǥ�⤯��
V6�˹Ԥ��ˤ������ä��ȹ�Ͼ������ʤ롥����P�Ȥȱ������硥
GE #249 I,aVL��Q��STE��V1��V6�ޤ�QS��STE��ST�Ͼ�������Ǥ��롥����¦�ɹ��ɤ�
�������塥V6�ʤ�����R�ȤǤ������̤����ɤˤ��QS�ˤʤ�ȡ�
�Ṳ̋⸺�夵�졤��ˤ�PRP�ˤʤ롥
ecg 9-16 ���Ƥζ���ͶƳ��QS�ѥ�����
ecg 16-7 ��K�����Ƕ���ͶƳ��rS�ѥ�����ˤʤ�IVCD��V6������rS�ѥ�����
#57 ¦�ɸ��ɹ���
#249 �������¦�ɹ���
#293 ����¦�ɹ���
#294 �����ڡ�����
V1�ο����������������ٵ����ͤ��롥
BB p.46, fig4.34 I��rS, �����Ѱ�, RVH, COPD������P�ȡ����ײ�ž��V1��QS��V6��rS��
BB p.63, fig7.4 RVH, COPD������P�ȡ����ײ�ž��V1��QS��V6��rS��
BB p.75, fig7.17 RVH, COPD������P�ȡ����ײ�ž��V1��QS��V6��rS���㿶����I�Ͽ�ʿ��
BB p.76, fig7.19 �ٹ��ɡ�S1Q3T3��I��rS�ˤ�뱦���а̡�V1��qR�ޤ���rR'��V6��RS�����ײ�ž��
BB p.87, fig8.17 ���ɹ��ɡ�V1��rS��V3��rS���Իġ��Ŷ˴ְ㤤�β�ǽ����
BB p.117, fig9.11 LPFB ������ޥ֥��å���V1��rS�Ǥ��뤬��R�Ȥ���������
BB p.118, fig9.13 RVH������P�ȡ���90��ʾ塤V1��QS��V2��V6�ޤ�rS�ȡ�
BB p.118, fig9.14 ���¦�ɹ��ɡ�v1��qr�ȡ�V2��V4�ޤ�QS�ȡ���
BB p.126, fig10.12 Idioventricular Rhythm.
BB p.142, fig11.5A Ventricular escape.
BB p.143, fig11.6A Ventricular escape.
GE #25 Axis -30, rS�������ȷ���-30�ʤ�LAFB�Ȥ���������ˤ��롥
GE #186 �ַ�ŪWPW Type B�����麸�ӥ֥��å�����intermittent preexcitation.
�������ѹ���Ƴ��aberrant intraventricular conduction��
a) �弼������Υ���ѥ륹���ŵ�Ū�ɷ�ˤ���������ã���������ǡ�������ɷ���Ƴ�Ϥ���
�Ԥ��뿴�����ζ�ʳ����Ф�餺�Ա����ˤ����硢����ѥ륹�ο��������Ť��۾��
�ٱ䤹�뤿���ѹԤ��뤳�Ȥ����ѹ���Ƴ�Ȥ������ѹ���Ƴ�ϱ��ӥ֥��å�����
���ӥ֥��å������ޤ��Ϻ��Ӥ�ʬ�ޥ֥��å����Ǥ��롥
b) ���̤˿��ڤ��Ա�������Ԥ��뿴������Ĺ�������㤷����Կ�������û���Ȥ����Ա�����
û����Ĺ���Ȥ����Ա�����Ĺ����������ɷ���Ƴ�Ϥ���DZ��Ӥ��Ա������Ǥ�Ĺ����V1Ͷ
Ƴ��rSR'���α��ӥ֥��å����ȷ��Ȥʤ롣
c) �������ѹ���Ƴ�ˤ�ꡢ���ſ�QRS�Ȥ������������̤��ȷ��˻��Ƥ��뤿�ῴ����
�����̤�Ƚ�Ǥ��줿�ꡢ�弼�����������QRS�Ȥ�������������˿�������ȴְ㤨���
�뤳�Ȥ����롣
ʸ��a)�Ρ���Ԥ��뿴�����ζ�ʳ����Ф�餺�Ա����ˤ�����פȤϡ�
���ڤ���ʬ�ˤ���ޤǤλ��֤���Phase 3 Aberration,
���ʤ��T�Ȥ�����Ǽ���QRS��ȯ�����뤳�Ȥ��̣���롥
�� �㤤��
�� ventricular ectopy���۽���������ʳ��������������
���ι���QRS��T�Ȥϵ�ž���롥�⿶����ĴΧ�ȴط��ʤ�ȯ����
�� aberrancy �ѹ���Ƴ��
Phase3�ޤ���4��ȯ�����뱦�ӥ֥��å��ޤ��Ϻ��ӥ֥��å�����QRS��VT��SVT�ʤɤ�
��̮�ˤʤ뤳�Ȥ�¿����
 2:1��AFĴΧ����Phase 3�κ��ӥ֥��å������ѹ���Ƴ��3Ϣȯ³�������θ�1:1��AF��PSVT�ˤʤäƤ��롥
3Ϣȯ��QRS���������ʤ���ͳ�Ϻ��ӥ֥��å������δ֤˲������줿����Ǥ��롥
aberrant.pdf
abe1.pdf
abe2.pdf
�� retrograde concealed conduction �չ����Ը�����Ƴ
�ӥ֥��å��ζ�ʳ��Ƴ��¾¦�����Ť���Ȥ���ϰ��̿��ڤ���Ƴ�ˤʤ롥
���ο��ڶ�ʳ���չ����˻ɷ���Ƴ�Ϥ�ʳ�����뤿�ᡤ�Ƥӵӥ֥��å���
��³���뤳�Ȥ��̣���롥SVT�ΰ���Ū�ʽ긫�Ǥ��롥
�� IKur��IKs��æʬ�˽�λ�夹������K����ͥ���Ĥ��뤬��
IKr��K����ͥ�γ������֤����Ф餯��³���롥
��K��ɤˤʤ�ȡ����λ�³�������̤����夹�롥�������ä�LQT����K��ɤˤ�
���դ�ɬ�פǤ��롥
cf. Channel.pdf.
�� concealed conduction �Ը�����Ƴ
PVC�θ塤����ƶĴΧ����»�����硤PVC���չ�����AV Node��ɷ㤷��
�Ա����ˤʤ뤿�����ĴΧ����Ƴ����������뤿��Ǥ��롥
2:1��AFĴΧ����Phase 3�κ��ӥ֥��å������ѹ���Ƴ��3Ϣȯ³�������θ�1:1��AF��PSVT�ˤʤäƤ��롥
3Ϣȯ��QRS���������ʤ���ͳ�Ϻ��ӥ֥��å������δ֤˲������줿����Ǥ��롥
aberrant.pdf
abe1.pdf
abe2.pdf
�� retrograde concealed conduction �չ����Ը�����Ƴ
�ӥ֥��å��ζ�ʳ��Ƴ��¾¦�����Ť���Ȥ���ϰ��̿��ڤ���Ƴ�ˤʤ롥
���ο��ڶ�ʳ���չ����˻ɷ���Ƴ�Ϥ�ʳ�����뤿�ᡤ�Ƥӵӥ֥��å���
��³���뤳�Ȥ��̣���롥SVT�ΰ���Ū�ʽ긫�Ǥ��롥
�� IKur��IKs��æʬ�˽�λ�夹������K����ͥ���Ĥ��뤬��
IKr��K����ͥ�γ������֤����Ф餯��³���롥
��K��ɤˤʤ�ȡ����λ�³�������̤����夹�롥�������ä�LQT����K��ɤˤ�
���դ�ɬ�פǤ��롥
cf. Channel.pdf.
�� concealed conduction �Ը�����Ƴ
PVC�θ塤����ƶĴΧ����»�����硤PVC���չ�����AV Node��ɷ㤷��
�Ա����ˤʤ뤿�����ĴΧ����Ƴ����������뤿��Ǥ��롥
�찵�ʤɽ۴�ư�֤����ꤷ�����֤Ǥ�VT��ְ�ä�SVT��Ƚ�Ǥ���
SVT�ι�����̮���ޤ���Ϳ����ȴ֤���ξ��֤����˰����������礬¿����
���Τ����VT��SVT�Ȥδ��̤Ͻ��פǤ��롥
VT��SVT�δ��̡�
Welens p.47 Fig 3-7��p.49 Fig 3-9
Wide QRS Tachycardia�δ��̤ϡ����ޤͤˤ��롥
SVT�ξ��ϱ��ӥ֥��å��������ӥ֥��å��������롥
CRBBB���Ǥ�V1��rsR'���ǡ�V6��RS���Ǥ��ꡤV6��q�Ȥ������뤳�Ȥ⤢�롥
CLBBB���Ǥ�V1�����ζ���rS����V6��q�ȤΤʤ�R�ȤǤ��롥
�ܼ�Ū��Purkinje��Ƴ��Ԥ��Τǡ��ȷ��ϵԤǤ��롥
���ӥ֥��å�����VT��R�Ȥβ������˥Υå������뤳�Ȥ⤢�롥
Rs�ȡ�qR�Ȥˤʤ뤳�Ȥ⤢�롥V1��R�Ȥˤʤ���̮��rsR'�Ǥʤ����VT�Ǥ��롥
V6��ɬ��rS�ȤǤ��롥SVT�Ǥ�RS�ȤǤ��롥
���ӥ֥��å�����VT�����ι���r�ȤȥΥå��ޤ��ϥ��顼��ȼ��V1�Ǥ��ꡤ
V6�����ι���q�ȤǤ��롥V6��R�Ȥ�ĺ����1�ĤǤ��롥
�ܼ�Ū�˺�˦����Ƴ��Ԥ��Τǡ��ȷ�������Ǥ��롥
V1����V6�ޤ�����S����VT�Ǥ��롥Wellens: p.60 fig3-17
��7�Ǥ�B���������롥
V1����V6�ޤ�����R���Ϻ��������������Ǥ��ꡤ�̾ﺸ����������Ƴϩ�����ˤʤ롥
�ǥ륿�Ȥ�ȼ���ȳΤ�����˼��ư����˼��ư����˼����Ǥ��äƤ�褯��
AVN��չ�������Ƴ�����antidoromic circus movement ȿ����������ư�Ȥʤ롥
Wellens: p.61 fig3-18
orthodoromic conduction ����������Ƴ
antidoromic conduction ȿ��������Ƴ
circus movement ����ư
antidoromic circus movement ȿ����������ư
 Iipes & Jelife
Cardiac Electrophysiology Frim Cell to Bedside
Figure 80-6
Figure 80-4
Iipes & Jelife
Cardiac Electrophysiology Frim Cell to Bedside
Figure 80-6
Figure 80-4
AVNRT atrioventicular nodal reentrant tachycardia ˼������ꥨ��ȥ����
�̾﷿(Slow-Fast��)
���̾﷿(Fast-Slow����Slow-Slow��, ¿����Ƴϩ)
Slow pathway ����Ƴϩ
Fast pathway ®��Ƴϩ
Over View AVNRT-�����ο�-
fast-slow AVNRT��1��
�ŵ�������Ū�긫����ߤ�AVNRT��¿����
Lifeint
hefastlane.com-AVNRT
Accelerated Idioventricular Rhythm ¥�ʷ�������ͭĴΧ
BB p.157, fig12.26 AIVR��
I, aVR, aVL��QS���Ǥ���¾���������ι���R�ȡ�CRBBB���Ǥ��뤬��
���������θ�ȯ�δ������̤�Ϣ³�ȷ��Ǥ��ꡤ�����Τߤ�ñ�쿴¡���ͤ˸����롥
(V6�Ǥ�S�ȤϤʤ�)
���ӥ֥��å�����Purkinje��˦�μ�ưĴΧ�ǿ������70���١�
BB p.157, fig12.27 AIVR+�չ���P�ȡ�
�Դ������ӥ֥��å��˵չ���P�ȡ�
IMG_20180724_0002.png
IMG_20180724_0004.png
IMG_20180724_0006.png
aa1.gif
B��ȡ�������¦��ư�Ṳ̋��鿴����¦��ư�Ṳ̋�Ҥ��Ƥ��롥
R�Ȥ�STD�������Ǥ��Ƥ��뤬��T�ȤϾ�����ˤϤʤ�ʤ���
0.2, CRBBB+LPFB+�������MI��
���ǡ�peri-infarction block. #343��Ʊ���ȷ���
GE #1 IRBBB, V2-3��T�Ȥ���RVH������Ǥ��ʤ���
GE #2 LAFB+IRBBB, LAFB�ϼ�-70�Ǥ狼�롥IRBBB��V1��rSR'��V6��S�ȤǤ狼�롥
aVR��QR���礭����LAFB��PRR�ˤʤ롥
GE #3 long QT��LAA��T�Ȥ�Ω�������꤬��뤤���ǥ�˻��ѤǤ��롥
GE #4 1��AV�֥��å���LAFB��I��aVL��ȿž�о�T�ȡ�V5-6��T�Ȥ�����ǤϤʤ���
V2-3��STE�������ST�������Ȥ��ʿ�˸���ȵ�žT�Ȥˤʤ롥
������֤����첼���ɤβ�ǽ�������롥cf GE #283.
GE #5 I,II��STD��Tȿž��III��aVF��ȿžT�ȡ�V1-2��QS���Ű̡�PRPV4-6��ȿžT�ȡ�LVH��
���ǡ�AF������MI��digitalis effect
GE #6 ����30��3��A-V �֥��å��������佼ĴΧ��V1��qR, V6��rS������������
IVCD�Ȼ��Ƥ��롥T�Ȥ�ȿž���Ƥ��롥�����������̤�Ʊ����
GE #7 *�������¦�ɹ���AMI�����ɤ�ȿ������STE���۾�Q�ȡ�
GE #8 *I, aVL�ΰ۾�Q�ȡ�STE��II, III, aVF��STD��V2-6�ΰ۾�Q�ȡ�STE������¦�ɹ��¦�ɤ�AMI��
���ǡ���������4h��cf. #39�Ȥ��뤬#7�δְ㤤��#7�Ϸ㤷��ST�Ѳ���
GE #9 AVNRT, �չ���P�Ȥ�T�ξ����ʬ�ˤ��롥
���ǡ������180����̮��AF�Ǥ���а���Ū��300�Ǥ��뤫��1/2����150�ˤʤ롥
T�ξ����ʬ��upstroke of the T wave in the precordial leads.
GE #10 I, aVL��ȿžT�ȡ�V5-6�ο�ʿȿžT�ȡ�
���ǡ�1��AV�֥��å���ST�Ѳ��϶����ʤ�non-specific ST-T changes.P-R�ֳ֤�6mm.
GE #11 ��˼�����ڡ�����
GE #12 *CRBBB, LAFB, 2:1��AF, LVH
���ǡ�����90��NSR��T�ȤΥΥå���CRBBB�α�����ʳ�Ǥ��롥aVL��Q�ȤϹ��ɤΰ۾�Q�ȤǤ��롥
GE #13 AF��̮���Ť����ɹ��ɡ�������STD��
���ǡ�AF��LVH��LVH����̮�ˤ�뿼��STD��
GE #14 SNR, CRBBB.
���ǡ�CRBBB�����ɤȲ��ɤ�STE���鹼���ȷ��Ǥ��롥
the ST's are upwardly convex and T inversion and ST elevation.
GE #15 CLBBB����̮��NSR��
���ǡ�I��aVL��STD���LVH��V6��STD���ꡥ
GE #16 WPW, V1��V6�ޤǤ��٤Ʀ�R�ȡ�V1��RBBB�ȹͤ����V6��S�Ȥ��ʤ��Τ�
����Ǥ��롥ST�Ͽ�ʿ�⤷���ϲ��ߤ�����T�ȡ����졥
GE #17 QRS 0.13, CRBBB, P�Ȥ��ʤ�Nodal, QT��Ĺ����V6��ߤ��T�Ƚ�λ��Ĺ����
LQT��T�Ȥ�concodal. S�Ȥ��礭���ˤ�ؤ�餺2�����ǤϤʤ���
GE #18 V1-4��QS�Ȥ�STE���������AMI��
���ǡ�1��������MI�ǻ�³����ST�徺�Ͽ������פ碌�롥
GE #19 II,III,aVL�����V1��Q��V2�Ϻ������٤�R, V1��V4�ޤǿ����о���T��
������ֹ��ɡ�
GE #20 I, aVL���Ű̥��ȥ쥤��T�ȡ��������硥
���ǡ����Ʊ����
GE #21 ���
GE #22 LAH, II,III,aVF��ST��ʿ��V4��V6��ST��ʿ�����졥
���ǡ�IVCD��V1��V2��QRS�˥Υå����������뤿���IVCD�Ȥʤ롥
GE #23 NSTWC
GE #24 II,III,aVF�ΰ۾�Q�ȡ�ST���ߡ��Ť����ɹ��ɡ�
GE #25 LAH,ȿ���ײ�ž��������V1��
-30�������Ǥ⤢�뤫��ڡ��˿��Ǥ��٤��Ǥʤ���
GE #26 I��21mm, aVL��ޤ�ƥ��ȥ쥤�������ײ�ž��U�Ȥ�ޤ��LQT��
�������硥���ɹ��ɤβ�ǽ����������ֹ��ɤǤϤʤ���
III,aVF��QS��T�Ͼ�����ǥ��ȥ쥤��ȹͤ��롥II��RS�Ȥ�Q�Ȥ��ʤ���
���Τ���ɹ��ɤȿ��ǤǤ��ʤ���
GE #27 II,III,aVF�ξ�����Q�ȡ�III��aVF�ϲ���ST��V2,V3,V4�ι⤤T�ȡ�
��K��ɤǤϤʤ�Benign Early Repolarisation(BER)��
GE #28 Nodal, �ͻ�ե�åȡ�V1,V2��R/S�Ϥܤ�1��V2��RS���Ǥ��礭��PRP�Ǥ��롥
��������ˤ��Ƥ�V1��T��ȿž���Ƥ��ʤ�������������硥
V6���礭��Q�����ˤʤ롥
���ǡ�1��AV block, PQ 0.24, ���ɹ��ɡ�Axis -30.
LAH�ξ��II,III,aVF��r�Ȥ�ɬ�פ��������줬̵������۾�Q�ȤǤ��롥
LAH�Υƥ����Ȥ��ɤ�ȡ�I��qR�⤷����R�ȡ�III��rS�ȤǤ��롥
�Ȥ�����II��Qr�Ǥ���r�Ȥθ��ID��¸�ߤ��롥����ϱ���������¦�ɤ�
��ʳ�ȷ��Ǥ��롥
V1�ι⤤R�Ȥϸ��ɹ��ɤαƶ��ȹͤ����Ǽ���Ǥ��롥������ͳ��
V5,V6��Q�Ȥ�¸�ߤ��뤫���������ɹ��ɤ�ȼ�äƤ���ȹͤ���٤���
II,III,aVF�ι��ɤα�Ĺ�Ǥ��롥
GE #29 V3-5��NSST-TWC.
���ǡ�V3-6�ޤ�sagging T�ȡ�
GE #30 CRBBB+LVH����˼���硤LQT��
���ǡ����Ʊ����
GE #31 I,aVL��Tȿž��I,III,aVF�����V1��V3Q�Ȥ�T��ȿž��V4��V6��ʿST��Tȿž��
V2��ST�徺��������ֹ��ɡ����Ǥˤ���ֹ��ɤϤʤ���
GE #32 QRS�����������Ƥ�ͶƳ��R��T��ȿž�����ӥ֥��å����ο����佼ĴΧ��
���Ǥ�AF��IVCD��LVH��������V6��S�ȤϤʤ���ILBBB�Ǥ��롥
GE #33 PR0.28�äǤ��뤬WPW��V1��R�ȡ����ϡݤ����鱦������Ͽ��ǤǤ��ʤ���
���Ǥ�IRBBB��1��֥��å���LVH�������礲�롥V6��S�˵����Ĥ��Ƥ��ʤ���
GE #34 1��֥��å���V1-3��1���ܤ�WPW�;弼���������̤˸����뤬���Ǥ�
���Ҥʤ���
GE #35 Af��V1��QR��V2��rSR'������V6��s�Ȥˤ��IRBBB��
V1��Q�ȤϹ����ȷ��ǤϤʤ���V2�Ǥ�rSR'�ˤʤäƤ��뤿�ᡥ
GE #36 Af, digitals, LVH��
GE #37 II, III, aVF��STD, digitaris��T�ȡ�1��AV- Block, V2-V4�ζ���STD��
Puls 125�ˤ������Ѳ���old ������ֹ��ɡ�
���ǡ���ǹ�äƤ��뤬�������ꥹ�ǤϤʤ���
GE #38 normal ECG��
GE #39 tachy, lafb, old a-s MI,
���ǡ�P�Ȥʤ���SVT��¾�Ϲ�äƤ��롥
GE #40 ��˼���硤V1-2��QS�������狼��
���ǡ��Ť���ֹ��ɤȤ��Ƥ�褤��V5-6, I, aVL���Ƥ�٨ʿT�ȡ�
GE #41 �����а̡�LAE,RAE, V1��rsR'��T���ȥ쥤���ž��V6���礭��RS�ȡ��������硥
����V1��IRBBB�ȴְ㤦��V6��S�Ȥ����顼�Ǥʤ����Ȥ����ա�
QRS 0.9���֥��å��Ǥʤ��ڵ�ΰ�ĤǤ��롥
������
GE #42 ξ��˼���硤��90�롤II,III,aVF��q�ȡ�1SQ3T3�����ײ�ž��
V6��Tʿó��I�����Ű̡����ɹ��ɤȤ����T�Ȥ��Ѳ������ʤ���
������rS��걦�����硥
���ǡ��ٵ���
�����������Q��
GE #43 AF��II,III,aVF�������礭��QS����I,II��꿴���ڡ�����
V1��V1-5�ޤ�QS����V6��rS����V6��R�Ȥˤʤ�ʤ�����LBBB�Ȥʤ餺
IVCD�Ȥʤ롥�����������ڡ������Ⱥ��ӥ֥��å�������-60�ʲ��ˤʤ롥
GE #44 �Ť����ɹ��ɡ��Ṳ̋�꺸�����硥�������ꥹ��
���ǡ�II,III��r�Ȥ������뤫�鲼�ɹ��ɤǤϤʤ���
GE #45 ����ʿ��V5-6, I, aVL��ȿžT�ȡ�II, III, aVF��ȿžT�ȡ�P�ȤϤʤ���˼��ĴΧ��
���ǡ�accelerated nodal rhythm. ���ɤ�Non-Q-MI�ȿ��Ǥ����ǽ���⤢�뤬��
���ɾ����ʤ������ꡤ����ȤϿ��ǤǤ��ʤ���
GE #46 V1-3��QS��STE��PVC¿ȯ��V6, I, aVL��flat T�ȡ�������ֹ��ɡ�������β�ǽ���⤢�롥
���ǡ����Ʊ����
GE #47 1��AV Block, ��̮��³��VT��
���ǡ�����150������2:1��AF�Ȥ�ͤ����뤬QRS���������������SVT�ǤϤʤ�VT�Ǥ��롥
GE #48 ��˼�������ڡ��������ӥ֥��å�����
���ǡ��ڡ�����CRBBB��LAFB����
GE #49 ��˼���硤IVCD��III, aVF��ȿžT�ȡ��������Ű̡�
���ǡ�IIIͶƳ�ο���ȿžT�Ȥ�� non-Q-MI��פ魯��
GE #50 V5��QS�˸����뤬���Ŷˤΰ�ְ㤤��V6, I, aVL��flat T�Ȥ����ˤʤ롥
GE #51 3��AV Block, ¥��˼��ĴΧ����̮V4-6�Ȼͻ�ͶƳ�Τ�STD��
���ǡ�Af����̮����̮�ˤ��STD��
GE #52 II, III, aVF�ΰ۾�Q�ȡ�v2-6�ζ��٤�STD��T�ȤϾ������I,aVL�Υߥ顼STD�����ɱ������ɡ�
���ǡ�����ư̮�ܴ��ι��ɡ��������ɤε��ҤϤʤ���II���III��STE��������
V6��STD�Ǹ��ɹ��ɤϽ����Ǥ��롥
GE #53 �����а̡�ȿ���ײ�ž��ST����ʿ��LQT��
���ǡ��ۤ����flat ST's in inferolateral leads�Ͻ긫��
GE #54 PVC��ȯ���߾�T�ȡ��������ꥹ���̡�
���ǡ�P�Ȥ�����ĴΧ���Ѳ��Ϥʤ���������PVC�Ǥ��롥II��V1����LAA�Ǥ��롥
GE #55 II,III,aVF��STE��ȿžT�ȡ�V5-6��ȿžT�ȡ��۾�Q�ȤϤʤ�����������ǤϤʤ�������MI�β�ǽ����
���ǡ����ɹ��ɤη����ϲ�塥
GE #56 I��aVL��STD�����ΤĤ��Ǥߤ�ȡ�II��III��aVF��STE��ȿžT�ȡ�V5��STD��
V6�ο�ʿ��ȿžT�ȡ��������ɹ��ɡ�
���ǡ��������ɹ��ɡ�
GE #57 V1��V3�ޤ�RS�ǹ⤤T�ȡ�V4��V6�˽��ä�R�ȤϾ�����V6��QS��STE��
�ߤ����Ȥ�̵���ȷ����������硩�ͻ����Ű̡�
���ɤ�AMI��V1��R�Ȥϸ��ɹ��ɤΤ��ᡤ�⤷���ɹ��ɤ�STE��ȯ������
�ޤǤδ֤Ǥ���С�V1��V3�ޤǤΥߥ顼STD��ȯ�����ʤ���V5��V6��STE��
������AMI����II,III,aVF���Ѳ��Ϥʤ����鱦��ư̮�����
���äơ��������ޤ��ĺɤˤ��¦�ɸ��ɹ��ɰʳ��˹ͤ����ʤ���
GE #58 Nodal, P�Ȥ������ʤ���I, aVL�β���ST����žT�ȡ�V4-6�ޤǤε�žT�ȡ�
���ǡ�II,III,aVF�ε�žT��ͭ�٤ȹͤ���Non-Q-MI���θ����.
GE #59 I��aVL�ο�ʿȿžT�ȡ�V1-3�ΰ۾�Q�Ȥ�STE��PVC���������ɹ��ɡ�
���ǡ��������ɹ��ɡ�
GE #60 AF�ȱ�������
P�Ȥ������ʤ���V1���4:1��AF�Ǥ��롥
110��α����а̤�V1���Դ������ӥ֥��å���T�ȵ�ž��V1-v3�ޤǤ��ꡤ
V6��S�Ȥ�ͭ�դ��礭�����ͻ�ͶƳ�ϱ����а̤����Ű̡�II, III, aVF��
���ߤ���ST�������ȤȾ����T�ȤϿ��ڵ����פ魯�����礿��긫�ǤϤʤ���
GE #61 I,aVL��ȿžT�ȡ�V1-4��STE��ȿžT�ȡ�������ֹ��ɤν����
���ǡ�V2��r�Ȥ����뤿���nonQ-MI�β�ǽ�����ꡥ
GE #62 I,aVL��STD��II,III,aVL��STE��ȿžT�ȡ�V3-6��STD�����ɹ��ɡ�
���ǡ����ɹ��ɤε�������
GE #63 ��˼�ڡ�����ñ�˥ڡ����������Ṳ̋��礭�����ѥ������ơ�����롥
GE #64 �������ӥ֥��å���
GE #65 1��AV�֥��å����������ꥹ����
U�Ȥ�QTc�˲û����Ƥ��롥��ʿST�䲼��ST�ϥ������ꥹ���̡�
GE #66 ��̮��II,III,aVF��STE��I,aVL��STD��V5-6��ȿžT�ȡ����ɹ��ɤε�������
���ǡ�V6�˾�����STE�����뤿��˲���¦�ɹ��ɤǤ��롥V4��STD�ϥߥ顼���̡�
GE #67 ��̮��I,aVL, V2-5�ζ���ȿžT�ȡ�nonQ-MI.
���ǡ��嵭��Ʊ����non-Q infarction.
GE #68 ���ӥ֥��å���II,III,aVF��STE��V5-6��STE��V2-3��STD���������ɡ�¦�ɡ����ɹ��ɡ�
���ǡ�����¦�ɹ��ɡ����ɤε��ҤϤʤ����ޤ����ӥ֥��å��ε��Ҥ�ʤ�����
I��V2-3���礭��R�Ȥϱ��ӥ֥��å������롥
GE #69 �����а̡�LAFB��PRP��ʿó����T�ȡ�
���ǡ�1��AV�֥��å���NSTWC's��
GE #70 ��̮��1��AV�֥��å���V5-6��STD���߾�T�ȡ��������ꥹ���̡�
���ǡ����Ʊ����
GE #71 �������ȷ�
RBBB������¦��AMI��ȯ����II��aVF��STE�����顤�������ɹ��ɤ�ȯ�����Ƥ��롥
V1-5�ޤǰ۾�Q�ȡ�
GE #72 1��AV Block��LQT��
���ǡ����Ʊ����
GE #73 ��-60 V1-V5�ޤ�rS�ǻ����ȷ���V6��RS����S�������礭����
LAFB, QRS����0.14������,�ޤ��Υå������뤿��IVCD��
GE #74 WPW��
GE #75 *I��aVF��걦���а̡��ͻ����Ű̡��ͻ�Ǥ������Ƥ���V1��P�Ȥ�걦˼���硥
V1��R�Ȥ�V1-3��ȿžT�Ȥ��RVH��
���ǡ�V6��S�Ȥ���ס������������Ȥ���IRRB�ǤϤʤ���cor pulmonale.
GE #76 Axis -30�ʲ����ĵ���������ֹ��ɡ�
���ǡ���̮��LAA����������ͽ�ۤ��ʤ���Фʤ�ʤ���
GE #77 ?��̮��CLBBB����̮�ˤ��STD��V6��S�Ȥ��ʤ���
���ǡ�2:1��AF��V5-6,I�Ͼ��������۾�Q�ȤǤ��롥II,III,aVF��۾�Q�ȡ��������äƲ���¦�ɹ��ɡ�
GE #78 ?4:1��AF��PVC��IRBBB��CLBBB��V4-5�ΰ۾�Q�Ȥ�����Ǥ��������ɹ��ɤ���
���ǡ�AF�Ǥ��뤬R-R�ֳ֤��������IRBBB�ˤĤ��Ƥε��ҤϤʤ���
GE #79 �ĵ������ɹ��ɡ����ײ�ž��
���ǡ����Ʊ����
GE #80 CLBBB�˸����뤬i, aVL��q�Ȥ�¸�ߤ��롥
���ǡ�LAFB��IVCD��PAP��LAA��
GE #81 QRS 0.16, I,aVL��CLBBB��V6���ͤ�����R�ȡ�II,III,aVF��QS�ȡ�
V1��CLBBB��rS�ȡ�V6��rsR'S'�DZ��ӥ֥��å��͡�IVCD��Long-QT��
���ǡ��Ų������ɬ�ס�
GE #82 II,III,aVF��QS��I,aVF�Ͽ�ʿST��I�ΰ۾�Q�ȡ�V5,V6��QS�ȡ���T�ȡ�
�Ť�����¦�ɹ��ɡ�LAFB��
���ǡ�II,III,aVF��QS�ϼ�<-60�Ǥ��뤫�顤LAFB��Ŭ���ˤʤ뤬��
���ɤξ��LAD��LAFB�Ͽ��ǤǤ��ʤ��Ȥ�����������peri-infarction block
���ʤ�LAFB�Ͽ��Ǥ��ʤ���Фʤ�ʤ��Ȼפ���
GE #83 Af, QRS 0.8, I��R��II��III��rS��aVL�˾�����q�ȡ��ͻ��T�����Ƶ�ž��
V1�Ϻ��ӥ֥��å���rS�ޤ���S�ȡ�V2��V4��rS�ȡ�V5,V6��Rs�ȡ�IVCD��LAFB��
���ǡ��嵭��Ʊ����
GE #84 normal ECG
GE #85 ����Ū�����Ű̡�STʿó��T����
���ǡ�cardiomyopathy���ðۤʽ긫�Ϥʤ���
GE #86 II,III,aVF������Q�ȡ�V4��V6STD��ʿT�����졤�Ť�IWMI����
���ǡ�STD�ϥ������ꥹ��sagging��Q�Ȥ�ͭ�٤ǤϤʤ���
GE #87 QRS 0.12, II,III,aVF��Qr��Af��V1��V6�ޤ�rS�ȡ�T��V6�ʳ��������
����-50�롥Af������P�Ȥο��Ǥ��Ǥ��ʤ�����IWMI��
���ǡ�IWMI��IVCD��V6��rS�Ǥʤ�������QS�Ǥ��뤬��IVCD�ˤ��롥
Ge #88 ƶ����̮��V5,V6��STD��
���ǡ�wandering P, digoxine��sagging T.
Ge #89 BER.
���ǡ���K��ɡ�
GE ?#90 IVCD�ͤ�VT����K��ɡ�
���ǡ�aVR��P�Ȥ������뤫��SVT��
GE #91
GE #92 II, III, aVF�ξ����ʰ۾�Q�Ȥ�T��ȿž���Ť����ڹ��ɡ�V1��
R�Ȥ������ϰϡ�ȿ���ײ�ž��������U�Ȥ������뤬�����ϰϡ�
GE #93 �������ײ�ž������ͶƳ�Ͽ���ȿžT�ȡ�Non-Q MI.
GE #94 ƶ����̮�Υڡ�����
���ǡ����Ʊ����
GE #95 �ͻ����Ű̡�II,III,aVF��STE��aVL�Υߥ顼STD��V2-3�Υߥ顼STD��V5-6��STE����������¦�ɹ��ɡ�
���ǡ����Ʊ�����������Ǥϥߥ顼STD��ȯ�����ʤ���
GE #96 LAE, CRBBB���ѹ���Ƴ��V2-4��STDȿžT�ȡ�����¦�ɤ�non-Q IM�ε�����
���ǡ��ѹ���Ƴ�ǤϤʤ�PVC�Ȥ��Ƥ롥
GE #97 LAA, PVC, �ĵ���������ֹ��ɡ�ILBBB.
���ǡ�Axis -50��LAFB��P�Ȥ�QRSľ��˾�ä�ectopic beat(�۽�����ư)��V6��S�Ȥ��ʤ���
? II,III,aVF��ȯ����������T�Ȥ����狼�۾狼��
�������۾�T�ȤǤ��롥I,IIͶƳ�ǤϾ����R�Dz�����T�ȡ����������ʤ�II,III,aVF������
�۾��ȿžT�ȤǤʤ���Фʤ�ʤ���
GE #98 ƶ������̮��ȿ���ײ�ž��
���ǡ����Ʊ����
GE #99 aVR��Τ������Ƥ�ͶƳ��STE��PR�ֳ֤��㲼��������ꡥ
���ǡ����Ʊ����
GE #100 ������ֹ��ɤˤ��CRBBB+LPFB��1��AV block
���ǡ�¿����ʬ�ޥ֥��å���MI�ȴط��ʤ����������"peri-infarction block"�Ǥ��롥
GE #101 PR 0.24, ȿ���ײ�ž��V3��V5��STD�����졥
���ǡ�L-QT, NSSTWC. paroxysmal AF��ͽ�ɤ�quinidine�����ѡ�
T�ȤΥơ�������ա�
GE #102 wanderling P, PAC, LAD,
���ǡ�Multifocal atrial tachycardia (MAT)
GE #103 Junctional rhythm
���ǡ�Nodal bradycardia, rectrograde P.
GE #104 I,aVL��STE��II��RS�Ǿ����T��III,aVF��STD�����T�Ȥǥߥ顼��
V1��rS��STDȿžT�ȡ�V2,V3���������T�ȡ�V4,V5,V6��STE������T�ȡ�
����¦�ɹ��ɡ�
GE #105 LAFB+CRBBB, V2����STE�Ǥ��뤬��CRBBB�ˤ���Ѳ���
���ǡ�V2�Τߤʤ餺��V1����V3�ޤ�STE�Ǥ��뤫�顤����������ֹ��ɤǤ��롥
GE #106 GE #106 CLBBB��LVH��Axis -60���LAD��������LAFB�ȤϿ��Ǥ��ʤ���
V1��r�Ȥ����餫�ǤϤʤ���V6��R�ȤΤߤ�s�ȤϤʤ��������ɤ�s�Ȥϱ��Ӥ�����
�Ǥ��뤿��ˤ��Ǥ�æʬ�ˤ��Ƥ��롥�������¦�ɤζ�ʳ�Ͽ�������Ʊ��
�����ߥǤ��뤫��s�Ȥ�ȯ�����ʤ���
GE #107 LAFB��PRP��
GE #108 ����Τ褦�˸����뤬II, III, aVF��STE��I, aVL, V2��STD������β��ɹ��ɡ�
GE #109 Eisenmenger, �������硤�����а̡��Դ������ӥ֥��å��˸����뤬��VͶƳ�ǥ��㡼�פ�S�ȷ���
GE #110 ξ��˼�����STȿž��ȼ��LVH��
GE #111 AF, IRBBB��
���ǡ�V5,V6��R�Ű̡�STD��꺸����ĥ��Marfan's syncrome��AR��
GE #112 P�ȤϤʤ���˼��ĴΧ�ν�̮��V2-5�α���T�ȤǤ��뤬�������ʤ������첼���ɤǤϤʤ���
���ǡ���̮���ܹ���ĴΧ��PRP��NSST-TWC's.
GE #113
GE #114
GE #115
GE #116 Accerated juctional rhythm, pericarditis
GE #117 4:1AF��LVH��V1��Q�Ȥ�����������ꥹ���̡�
���ǡ�STD�Ǥ��äƤ�T�ȤϾ����������LVH�αƶ���
GE #118 1��AV �֥��å���CLBBB��PVC��
���ǡ�3:2 Wenckebach��
GE #119 *CLBBB
GE #120 LAE, RAE, LVH
GE #121 *II, aVF���ݤ����鼴��-30��ʲ���V1��PVC�Τ褦�˸����뤬�����rsR'
�Ǥ��롥V1-V3�ޤ�rsR'��ȿžT�ȡ�V4-V6��rS�Ȥ�����T�ȡ�
���ǡ�LAFB+CRBBB������RBBB�ϱ�������ο��ǤϽ���ʤ�����
V1�ΰ۾�ʹ⤵��R'��V6��S�ȡ�������ȿžT�Ȥ�RVH�碌�롥
�̾��CRBBB�Ǥ�V6��R�Ȥ�������S�ȤǤ��뤬��RVH�Ǥ�R�Ȥ���������
S�ȤϱԤ�������
GE #122 II��III��aVF�ξ�����q�ȡ�ST�������ȷ���VͶƳ��ȿ���ײ�ž�����ƶĴΧ��PR��160ms���ۤ������ȷ�
���ǡ��۾�Q�ȤȤ��Ƹ��뤫�ɤ���������
GE #123 I��aVL�����V1-6�ޤǤ�ȿž�о�T�ȡ������칼�ɡ�
���ǡ���Q�������ɹ��ɡ�LQT�����ꡤVT�ˤʤ�䤹����
GE #124 II��III��aVF�ΰ۾�Q�Ȥ�STE��I��aVL��STE��ȿžT�ȡ�������V1��RS�Ȥǰܹ��ӡ���ü��ȿ���ײ�ž��
�������ɹ��ɡ�
���ǡ��������ɹ��ɡ�V1-2��STD��긫������롥
GE #125V1��걦����Ƴ�ٱ䡥
����ſޡ�
GE #126 II��III��aVF��STE��V2-4��STD��I��aVL��STD���������ɹ��ɡ�
���ǡ��������ɹ��ɤȿ��Ǥ��Ƥ��뤬���狼���
GE #127 ƶ����̮����˼���硤LQT��LVH�����ȥ쥤��T�ȡ�
���ǡ�aortic stenosis�ˤ��LVH��
GE #128
GE #129
GE #130 V1-2��QS�ȷ�������ɹ��ɤβ�ǽ�������뤬�����狼�⤷��ʤ���
GE #131 IRBBB�Ǥ��뤬��V1��T�Ȥϵ�ž���Ƥ��롥�����а̤Ǥ����
��������β�ǽ�������뤬�������ŵ�����45������顤���ɾ���ȼ��ʤ��������뤷�ʤ���
GE #132 PRû�̡�����̮ĴΧ��ȿ���ײ�ž��WPW�β�ǽ���Ϥ��롥
���ǡ�low atrial or coronary sinus pacemaker�Ǿ��Ʊ����
GE #133 ��-30�ٰʾ塤LAFB�Ϳ��Ǥ���������V1-6�ޤ�rS�Ǥ��롥���Ȥ��Ƥ�IVCD�Ǥ��뤬����QRS����������
���ǡ�����Ū�˲��ɹ��ɤξ���II��III��aVF��QS�Ȥˤʤ뤿�ᡤLAFB�ȤϿ��Ǥ��ʤ���
������Ǥ�II��r�Ȥ����뤫�鲼�ɹ��ɤǤϤʤ����ޤ�V2��r�Ȥ����뤿�ᡤ���ɹ��ɤǤϤʤ���
��ĥ�����ھɤǤ��롥
GE #134 *AF����̮��II��III��aVF��STD��V2-6�ι��Ű̡�STD�����ꡤLVH���줷������
���ǡ�AF����̮�˰�¸����STD���������Ṳ̋Ϥʤ����ͻ�ͶƳ��R�Ȥβ�����ʬ����Ĺ���ƻ��ѷ��˸�����Τϡ�
������¦æʬ�ˤ��ٱ䤹�뤿��Ǥ��롥LVH��Ʊ���ͤ������Ѥ��롥����ͶƳ�Ǥ�S�Ȥαƶ���¿�Ͳ������
�Ԥˤʤ롥
GE #135 *II�Ǧ��ȤΤ褦�˸����뤬���������ӥ֥��å���PAC�ˤ���佼ĴΧ��
���ǡ�ST����̮��PAC�����롥V3-5��STE��AMI��Ƚ�Ǥ��롥
���䡧PAC�ˤ��HIS¦���դ��佼ĴΧ�θƤ�����
GE #136 �����������ֹ���
���ǡ�QT��Ĺ��Ҥ٤Ƥ��뤬��V1-5�ξ���̤�ST�������Ȥˤϵ��Ҥ���Ƥ��ʤ���
GE #137 PAC��³��QRST�������ȷ���
GE #138 ƶ��ߡ�
GE #139 �����ڡ�����
GE #140 ����ƶĴΧ
GE #141 ƶ������̮
GE #142 ƶ����̮
GE #143 �����֥졼�����calibratin pulses.
GE #144 �ϥࡤAC interference.
GE #145 ��ư��Mucle Tremor (Somatic).
GE #146 ����ư�ɤˤ�������ư
GE #147 �ڡ���������ȤΥե塼�����
GE #148 �ڡ���������ɷ�����
GE #149 �ڡ���������������ɡ�
GE #150 �ڡ���������������ɡ�
GE #151 ��˼������ߡ�
GE #152 AF�ȿ����ڡ�����
GE #153 ��˼�ڡ�����
GE #154 ��˼�����ڡ�����
GE #155 ��������
GE #156 �����ե塼�������̡�
ñ�ʤ�������̤��狼��ʤ���P�Ȥ�³���ƿ����������̤�����褦�ˤ⸫���롥
GE #157 ƶ��ߤˤ�뿴�����佼ĴΧ��
GE #158 VF
GE #159 ƶ�����II, III, aVF��STD���Դ������ӥ֥��å���short PRI
���ǡ�Lown-Ganong-Levine Syndrome.
GE #160 WPW��V2-4�ޤ�T�ȵ�ž��
���ǡ�T�ȵ�ž��WPW������Ƴϩ�αƶ���������Ū�ʤ�Τ�������
GE #161 ξ��˼���硤LQT��
���ǡ�IVCD�Ȥ���Ƥ��뤬��R�Ȥ�Ω������Ϣ³�����Ƥ���Τ���
GE #162 MAT��PRP��RAD
���ǡ������а̡�PRP��V6��S�Ȥ���RVH����Ǥ��Ƥ�褤�������120�ϰ۾�Ǥ��롥
GE #163 R on T��
���ǡ����Ҥ���Ƥ��ʤ�����MAT�Ǥ��ꡤ3���ܤϦ��ȤǤ��롥
GE #164 PVC2Ϣȯ��
GE #165 3Ϣ³PVC��
GE #166 PVC��2��̮��
GE #167 P�Ȥ��ʤ��ȿ��Ǥ��Ƥ��뤬��ƶĴΧ�Ǥ��롥PVC��
GE #168 �츻��������������
GE #169 ¿����������������
GE #171 Nodal �չ���P�ȡ�V3-6��T�ȵ�ž�� ���ǡ�I��aVL��STE��¦�ɹ��ɤΤ褦�˸����롥
GE #172 �������AMI���������ȷ���
���ǡ�V1��qR����RBBB��AMI�Ǥ��롥II��III��rS����LAFB��
GE #173 AF�ν�̮��II��III��aVF��STE��I��aVL�Υߥ顼�ˤ��STD��
���ǡ�junctional escape rhythm. �ܹ����佼ĴΧ��SA arrest.
GE #174 WPW, III, aVF�ΰ۾�Q�Ȥ�WPW��¦����Ƴϩ��ȯ�����Ƥ��롥���Ȥ�³��QRS����Ϣ³�Ǥ��롥
GE #175 I��rS��STE��II,III,aVF��STE�����˾�����q��V1��R'�Ƕ���STD��
V2��V4�ޤǤ�RSr'�Ƕ���STD��V5��RS��STD�Ⱦ����T�ȡ�V6��
R��STE�����ɹ��ɡ�¦�ɹ��ɤȸ��ɹ��ɤǤ��뤬���ߥ顼������뤿��
������֤����첼���ɤ�ʻȯ���Ƥ��롥
GE #176 II,III,aVF�ΰ۾�Q�ȡ�V2��V4���������ȷ���V5��V6��Q��STE��
�Ť����ɤȵ���������¦�ɹ��ɡ�
GE #177 II, aVF��STE��V2-4��STE�Ǥ��뤬�������̤�ST�������ȡ��������ɹ��ɤ���
���ǡ�����Ѹ�ο�����ꡥ
GE #178 V2-4�ζ��٤�STE�Ⱦ���̤�ST�������ȡ��������ɹ��ɡ�
���ǡ����ɤ�ޤ�������ɹ��ɡ�aV��STD�ϥߥ顼��������������ǤϤʤ���
#177�Ǥ�aVL�Ǥ�STE�Ǥ��롥
GE #179 PVC3��̮��Trigeminal PVC's.
GE #180 4�����PVC��
GE #181 ������ͭĴΧ��idioventricular rhythm.
GE #182 ¥�ʷ�������ͭĴΧ��accelerated idioventricular rhythm.
GE #183 ƶ����̮����˼���硤V-3�۾�Q�ȡ������а̤Ǥ��뤬��LAFB�ǤϤʤ���(V6��S�Ȥ��ʤ�����)��
�������Ǥ��뤬��MI�Ȥϴط����ʤ���
GE #184 �����janctonal tachycardia, I, II, III, aVF, V5, V6��ST�徺�Ͽ������Τ��ᡥ
��������ST��AF, JT�Ǥ褯ȯ�����롥
GE #185 Wenckebach 4:3 ��AV B;ock, �������ɹ��ɡ�II, III, aVF�ΰ۾�Q�Ȥ�ST�徺��
V2��STD�ȹ�T�Ȥϸ��ɹ��ɡ�����̮��¦��ϩ�β������������Фζ�ĥ�㲼�Dz������롥
GE #186 �ַ���WPW��ȿžT�Ȥ�WPW�ˤ��۾��ʬ�ˡ�
GE #187 ����ſޡ�
GE #188 1��˼���֥��å���I,aVL�ε�ž�о���T�ȡ�aVL�ϰ۾�Q�ȡ�V2,V3��STE
��ʿST������ȿžT�ȡ�V4��ȿžT�ȡ�V5�Ͽ�ʿST��T�ȤϤʤ���
V6��STD����ʿST�����������T�ȡ�
���ǡ�Lateral ST and T abnormality.�ȤʤäƤ��뤬�����¦�ɹ��ɤν����������ֹ��ɤ�
����ȸ����II��III��aVF�Υߥ顼STD����������롥
GE #189 P�Ȥ�QRS�θ塤II,III,aVF�ΰ۾�Q�Ȥ�T��ȿž��ST��II���III�������⤤��
I��aVL��STD�Ǿ����T�ȡ�v1��V3�ϰ۾�Q�ȡ������ľ��ST������T�Ⱦ������
V4��V6��STD�������T�ȡ�
���ɹ��ɡ�������ֹ��ɡ�V5-6.I,aVL¦��(�ߥ顼STD)����
GE #190 II,III,aVF���۾�Q�ȤΤ褦�˸�����WPW��ST������T�Ȥ����
GE #191 ̮��120���ͻ�ȶ������Ű̡�PRD��ST���������
Acute pericarditis
GE #192 ̮��75��I,aVL��ST����ȿž��LVH��LAH������������ֹ��ɡ�
������� �ڡ���������ˤ������̮.
���Ǥϲ��ɹ��ɤȤʤäƤ��뤬��II,III,aVF���Ѳ��Ϥʤ������ǡ�
GE #193 I,aVL��STD��T��ž��II,III,aVF�ΰ۾�Q��STE��V2��V6�ζ���STD�Ⱦ����T��
���ɡ��������ɡ�����ư̮���ĺɤ�Ƚ�äƤ��뤫�鱦�����ɤǤ��롥
V1���Ѳ������ʤ���V2,V3��STD���������Ȥ����դ��롥
GE #194 Poor P wave��Sinus Rhythm. LAFB��V1-3��Poor R Progression�Ǥ��ꡤMI�ǤϤʤ���VͶƳ��3���ܤ�SVT��
GE #195 �������ӥ֥��å��Ǥ��ꡤ����ͶƳ��T�Ȥϵ�ž������ϴ������ӥ֥��å��Ǥ�������Ѳ��Ǥ��롥��������Ϥʤ���
GE #196 ��90�ʾ塤����P�ȡ�V1��rsR'�Ǥ��뤬��rs�����˾�������R'�ϥ��㡼�פ�
�̾�α��ӥ֥��å��Ȱۤʤ롥V2��V6�ޤǤ϶������ζ���S�ȡ����ӥ֥��å�
�Ǥ����S�������������顤���������鸫�Ƥ�RBBB�Ȥϰۤʤ롥V1��
����T�Ȥǡ�V2��ʿó��V3-V6���̾��T�ȡ�R�Ȥ�V3���Ǥ�⤯��
V6�˹Ԥ��ˤ������ä��ȹ�Ͼ������ʤ롥����P�Ȥȱ������硥
GE #197 PSVT��T�ȤλϤޤ�˵չ���P�ȡ�STD�������롥
GE #198 COPD, Wandering AT, ����ͶƳ��COPD����ħ�� cf��BB p.75, fig7.17
GE #199 I,aVL��STE��II,III,aVF��ST���ߤ�2����T�ȡ�V6���Ѳ��Ͼ��ʤ���
���¦�ɤ�AMI��
GE #200 �����а̡�V1��R/S>1, ���ȥ쥤��T��RVH��RAA�Ϥʤ���
V4��TR������T�Ȥ�V6�ˤʤ뤬��V6�Ǥ�RS�ȤǤ��롥
GE #201 ƶ����̮����˼���硤II��III��aVF�ΰ۾�Q�ȡ�STE��VͶƳ���LVH��
���ǡ�AS�ˤ��LVH�����ɹ��ɤ��ɤ߲��������I��aVL��STD��T��ȿž�Τ褦�˸����롥
GE #202 1��AV�֥��å���IVCD���������ӥ֥��å���V6��rS��������IVCD��������
���ǡ�LBBB��I��aVL��q�Ȥ��ʤ����顤LBBB��
GE #203 V2-6���о�����žT�Ȥ�ꡤ�����첼���ɡ�
���ǡ������첼���ɡ�ST�������Ȥα�Ĺ�Ϥ褯�����롥QTD�ˤʤꡤ���̻��֤α�Ĺ���̣���롥
GE #204 I,aVL��ST����II,III,aVL��r���ꡤV1��QS��V2��V6�ˤ�R�ȡ�
���ײ�ž�����Ǥˤϵ��Ҥ���Ƥ��ʤ�LAH�Ǥ��롥
GE #205 I,aVL��STD����II,III,aVF��STE�̡�V1,V2��STD����T�ȡ�V5,V6��STE����T��
���ɸ���AMI��
���ǡ�V1,V2�β��ʤ������Ϥʹ��ɤǤ��ꡤ�������ɤ�ޤ�Ȼפ��롥
GE #206 I,aVL��STD��II,III,aVF�ΰ۾�Q�ȡ�STE��T��ž��V1,V2�ι⤤T�ȡ�
V2��STD��V6��STʿó��T�ȡ�ξ��˼���硤���ɹ��ɡ����ɤ˵ڤ֡�
���ǡ����Ʊ����#213�ν긫�μ�������ECG�ȽƤ��뤬������
GE #207 I,aVL��STD����II,III,aVF�ΰ۾�Q�Ȥȿ�ʿ�����ʱ�T��V1��STE����T��
V2��STD����T��V6ST�Ͽ�ʿ���Ť����ɹ��ɡ�
���ǡ�V2,V3�����˼P�ȡ�V2��R���⤤��ȿ���ײ�ž�����ɹ��ɤˤ��Ƥ�V1��r�Ȥ����롥
GE #208 4:1��AF��PRP��V4-5��STD
���ǡ��������ꥹ���̡�
GE #209 I, aVL��flat T�ȡ�V5-6�α���T�ȡ�
���ǡ�ξ��˼���硤�������Ű̡�
GE #210 I, aVL��STD��II, III, aVF��STE���������ɹ��ɡ�
GE #211 Mobitz II��2��AV �֥��å���
GE #212 3��AV �֥��å���
GE #213 WPW��T�ȵ�ž��WPW�Ǥ������Ѳ���
GE #214 1��AV �֥��å���
GE #215 CLBB
GE #216 WPW
GE #217 1��AV �֥��å���
GE #218 Mobitz I (Wenckebach) 2��AV �֥��å���
GE #219 ¥�ʷ�AV �ܹ���ĴΧ��
GE #220 �ܹ�������չ���P�ȡ����ա�
GE #221 Wandering Pacemaker ����Ū�˿������60�ʲ��ˤʤ롥���ա�
GE #222 ���ӥ֥��å���
GE #223 ��˼����
GE #224 ��˼��ư��
GE #225 ��˼��ư����ư����٤ƿ�������������
GE #226 �ܹ���ĴΧ�����ӥ֥��å���STE��
GE #227 ��˼�������̡�
GE #228 ��˼������������̮��
GE #229 3th Phase ���ӥ֥��å����ѹ���Ƴ��
GE #230
GE #231
GE #232
GE #233
GE #234 II,III,aVF�ΰ۾�Q�ȡ�III,aVF��ST���ߡ�ȿžT���Ť����ɹ���
II��ST��������ǡ��������MI��Ƚ�Ǥ��롥����q�Ȥ��⤷��ʤ���
GE #235 �������AMI��III��Q�Ȥ����Ǥϲ��ɹ��ɤο��ǤϤǤ��ʤ���
GE #236 I,aVL���ȥ쥤��T�ȡ���˹P�ȡ�LVH��
GE #237 LAH, V1��qR, V6��RS���IRBBB.
���ǡ��嵭���ɲä���1st AV block, LAH.
I,aVL�ι��Ṳ̋Ϻ�������ξ���Ŭ�����롥
GE #238 ����P��I�㿶������90, ���ײ�ž��ξ��˼���硤��̮���������硥
���ǡ��ٵ���Ǥ��ꡤ��������Ȥϸ����ʤ���
GE #239 ��̮��P�Ȥʤ���Af, II,III,aVF���礭��Q�ȡ�CLBBB.
���ǡ�IVCD, CLBBB�ʤ�V6��R�Ȥ�ɬ�ס�������V5��rSr', V6��QS�Ǥ��롥
IVCD��QRS����0.12sec�ʾ塢V1�Ǻ��ӥ֥��å���(rS)��V6�DZ��ӥ֥��å���(Rs)�Ǥ������
Af��Nodal��Ŭ���ʿ�����ݾڤ��뤬����̮�ˤʤ��sick AV node�Ȥ�����
GE #240 CRBBB,LAFB,LVH,LQT
GE #241 LAFB, IRBBB, PRP
GE #242 WPW
GE #243 QRS 0.12, Axis <-60, LAFB, PRP��V1��V6�ޤ�rS�ѥ�����IVCD��aVL��q�Ȥ������뤫��LBBB�ǤϤʤ���
���ǡ�������ֹ��ɤν����
GE #244 1��AV block, II, III,aVF�β���ST�Ⱦ����T�ȡ�digitalis�ˤ���߾�T�ȡ�
GE #245 ��̮��CRBBB��
���ǡ�2:1�ο�˼��ư��STD����̮�ˤ��ƶ�����˼��ư�Ϥ褯�狼��ʤ���
GE #246 AF����̮����̮�ˤ��STD��LVH��
GE #247 NSST-TWC. digitalis���̡�
GE #248 axis -30, SN, ¦�ɡ����¦�ɵ���ǤϤʤ�NSSTC��IVCD�Ǥ��롥
GE #249 I,aVL��Q��STE��V1��V6�ޤ�QS��STE��ST�Ͼ�������Ǥ��롥���ɹ��ɡ�
�����ϲ��4���֡�III, aVF�˥ߥ顼STD��������ǤϤʤ���
GE #250 I��aVL STD��II, III, aVF��STE��III����Q�ȡ�V1��rR��STD����T�ȡ�V2-3��RS��STD������T�ȡ�
V5-6��R�ȤϾ�������STE�˸����롥���ɸ��ɹ��ɡ�
���ǡ����ɹ��ɤϳΤ���V5-6��STE���¦�ɹ��ɡ����ɹ��ɤ�¦�ɹ��ɤ�Ϣ³�ȸ��Ƥ�褤��
GE #251 normal ECG.
GE #252 V1-2�ΰ۾�Q�Ȥ��Ť���ֹ��ɡ�
���ǡ����ɡ���ֹ��ɤϵ��䡥I, aVL, V5-6��ʿóT�Ȥ����ա�
GE #253 I, aVL V2-V5�ޤǤα���T�Ȥ�꿴���첼���ɡ�
���ǡ�non-Q infarction.
GE #254 AF, IVCD, LVH. AF��LVH�ϳΤ��Ǥ��롥CLBBB�ǤϤʤ�IVCD�������Ϥ狼��ʤ���
GE #255 3��AV Block��CRBBB����̮��
���ǡ�̮��30��entricular escae rhythm. CRBBB�ͤǤ��뤬AV NodeĴΧ�ǤϤʤ���
V1��qR����CRBBB�Ȥ����V2��r�ȡ�I��aVL��r�Ȥ��������Ǥ��ʤ���
GE #256
GE #257
GE #258 I,aVL��Q�ȡ�STE��PRD��II,III,aVF��STD��V1��r�Ȥ�����QS���⡤V2-6��
QS��STD���������¦��AMI�����ɤΥߥ顼��
���ǡ�AMI�Ǥ�QT-long�ˤʤꡤVT��ȯ�����䤹����
GE #259 PR 0.20, QT-long, V2-6��STD�������T�ȡ���̮�ˤ��ȿ�������졥
���ǡ����Ʊ����PR��0.24�ȿ��ǡ�
GE #260 ¦�ɸ��ɹ��ɡ���������I, aVL��Q�Ȥ�ST�徺��V6��Q�Ȥ�ST�徺��
V1-3�ι⤤R�Ȥ��о�����T�ȡ�
GE #261 AF��V2���⿶���Ǥ��ꡤLVH
GE #262
GE #263
GE #264 Axis -40�롤�����а̡�PRP��LAFB��idiopathic, dilated cardiomyopathy. R�ȤΤߤʤ餺��
S�Ȥ⾮�����ʤꡤV6�Ǥ��Ṳ̋����˾�������
GE #265
GE #266
GE #267
GE #268
GE #269 I,aVL��STD,ȿžT��II,III,aVF��STE��Q�Ȥʤ���V4STD��T�ȡ�V5,V6T�ȵ�ž��
IWAMI��
���ǡ�V6��STE������¦�ɹ��ɡ�V4��I,aVL��Ʊ�ͤΥߥ顼�Ѳ���
GE #270 I,aVL��STD�������T�ȡ�II,III,aVF��STE��V1��V4�ޤ�STD��V4���Ǥ����
V6��STE������¦�ɸ���AMI��
���ǡ����β��ϴְ�äƤ��롥
GE #271 V1,V2��r�ȤϤʤ��������
���ǡ��Ƹ��η�̡�V2��r�Ȥ��ǧ������ſޡ�
GE #272 Nodal, �ͻ��T�Ȥ�ʿó��V1��rS��T��ʿó��V2�ʹߤ�R�Ȥ����оξ����
T�ȡ���ü��ȿ���ײ�ž������-30���⡥
���ǡ�����̮ƶĴΧ������ͶƳ�������ʤ���
�丫��������¦�ȿ�����¦���ȷ������פ����ST������T�Ȥ�ʿó�ˤʤ롥
����ͶƳ�Ǥ�V2�ʹߤξ����ST�����T�Ȥ����ꤷ��V6�ǥե�åȤ�
�ʤ�Τ�Ǽ���Ǥ��롥
GE #273 ��20, �ͻ��STT��ʿó��V1��V5�ޤ�rS��V6��R���Դ������ӥ֥��å���
���ǡ������˴ؤ��륳���ȤϤʤ���
GE #274 I,aVL�Ǻ������硥V1,V2��QS��V6��RS�����ײ�ž��
���ǡ��������硤V1,V2��QS������ˤ��Ƥ��ʤ���V6��RS�Τ���
���������ŵ��Ū�긫�������Ƥ��ʤ���
GE #275 SN, ��̮��I,aVL��STD��III��Q�Ȥ�STE��V1��V4��STE�Ǥ��뤬��ST������
��˱���������ֹ��ɤν���ޤ��ϲ��ɸ��ɹ��ɤν���ʳ���
���ǡ�V5-6��STE�ȽҤ٤Ƥ��뤬��̣���狼���
GE #276 ƶ��̮��LAH��V1-3�ޤ�QS��Tȿž��V4-6��R�����⡤�����T��
���ǡ�SVT��LAH��
GE #277 V1��V6�ޤ�rS�ȡ�����ľ���˥ڡ����Υ��������롥T�Ȥ�����ȿž��
���ӥ֥��å����ο�˼���������ڡ�����
GE #278 I,aVL��STDȿžT��II,III,aVF��STE�о�T�ȡ�V1,V2��STD�Ⱦ����T��
V5,V6�Ϥ��STD���礭���Ѳ��ʤ���
���ǡ�����AMI. ���Ҥˤʤ�������������(���ɹ���)��ͤ����롥
final�Υߥ顼�������22��Ʊ���긫�Ǥ��롥
GE #279
GE #280 ����P�ȡ��������硥V1��rsR����V6��RS���� V3-6�ޤ�S�Ȥ��礭������˼�������硥
���ǡ��������ĺ������ˤ�뱦˼��˼�������硥��˼�����V1��ȿžT�ȡ�
GE #281
GE #282
GE #283 I,aVL�о���Tȿž��V1-4���о���Tȿž��V5�����о�Tȿž��V6�Ͽ�ʿ��
�ðۤʺ�ʬ�˥ѥ�����
���ǡ�������֤�Non-Q MI. �����첼���ɡ�
GE #284 #43��Ʊ�����ſޡ�I,II�˥ڡ�������å���CLBBB��IVCD��
��˼�ڡ���������100. II,III,aVF��STE��
���ǡ����Ʊ����ñ�˿�˼�ڡ�����
GE #285
GE #286
GE #287
GE #288
GE #289
GE #290 PR 0.2, QRS 0.14, CLBBB,
���ǡ���̮�ˤ��CLBBB�ǡ�̮���㲼����в������롥
GE #291 PR 0.24, PAC�����뤬��V1-3�ϻ��ײ�ž�ͤǤ��롥TR�� V4-5�ʳ��˰۾�ʤ���
���ǡ��嵭��Ʊ����isoelectric�Ȥ�R/S�椬1���̣���롥
GE #292 CLBBB�ͥڡ�����
���ǡ���˼�����ڡ�����
GE #293 SN ��̮��II,III,aVF��QSȿžT��V5-6��QS��ȿžT���ͻ����Ű̡�����¦��MI��
���ǡ��嵭��LAD���ɲá����Ͼ�˹ͤ��롥
GE #294 �����ڡ�����ŵ��Ū�ʺ��ӥ֥��å��ȷ��ˤʤ롥V6��QS�ѥ�����
���ǡ��ڡ����ɷ������P�Ȥ����ꡤP����V�ڡ�����
GE #295 LAFB. ȿ���ײ�ž��
���ǡ��ܡ������饤���������Ǥ��ƤϤ����ʤ���
GE #296 I,aVL��STD��II��Q�ȤϾ�������III��Q�Ȥ��礭����V5��STD��V6��Tȿž��
���ǡ���̮��II,III,aVF��ȿžT��AMI�Ǥ��롥
GE #297 ƶ����̮��
���ǡ�V2-4��TU�Ȥ��ɤࡥ2�����ǤϤʤ������ȷ��Ǥ��뤳�Ȥ����ա�
GE #298 I,aVL���LVH��TR��V4-5������ȿ���ײ�ž��V1-2��QS�������ϰϡ�
���ǡ����Ʊ�����⤤I,aVL��LVH��V6��RS��������ײ�ž��PRP�Ǥ��롥
���Τ����V1,V2��QS�ȷ������ɹ��ɤ�Q�ȤǤϤʤ���
I,aVR,aVL,V1,V2�ʤ�R��ñ���ȷ���late intrinsicoid deflection�������롥
�Դ������ӥ֥��å��ȿ��Ǥ��Ƥ�褤��
cf 11-10.
GE #299 LAD, CRBBB,CRBBB�Ǥ�LVH��V5�ޤ���V6��R��V1�ޤ���V2��S�Ȥ��礭����
Ƚ�Ǥ��롥2������ST�˴ؤ��Ƥϡ����ȥ쥤���ͤ�ST�������Ȥ�Ƚ�ǡ�
���̤�RS�ȷ��Ǥ����T�ȤˤĤ��Ƥϲ���ε�žT�Ȥˤʤ롥
GE #300 V1��CRBBB�͡�V6��CRBBBB�ͤˤ��IVCD��
���ǡ����Τˤ�IVCD�ȵ��Ҥ��Ƥ��ʤ������Ų��Kǻ�ٸ���ɬ�פȽҤ٤롥
GE #301 I,aVL��STD�ȥ��ȥ쥤��T��II,III,aVF�ζ���STE��겼��AMI��V1�⤤RS��
V2-3��RS��STD��V6�ϼ夤STD������T�ȡ�
���ǡ�����AMI��V1-2�ι⤤R�ε��Ҥʤ���¦�ɤ䱦���ι��ɤϤʤ��ȹͤ��롥
GE #302 CLBBB. II��>0������LAFB�Ͽ��ǤǤ��ʤ���
���ǡ�AMI�Ƿ����ϲ���ECG��
GE #303 ȿ���ײ�ž������ſޡ�
GE #304 IRBBB, QT����
���ǡ���˲ä���Nodal��V1-3�ǵչ���P��QRS�θ�˸����롥
GE #305 PQû�̡�IVCD�Ȼפä���WPW�Ǥ��롥
���ǡ�WPW��V4-6��S�Ȥ�����Ǥ��ꡤIVCD������Ǥ��롥
IVCD�Ǥ�R�Ȥ�Ω��ꡤΩ�������궦�˥��顼�ˤʤ롥CLBBB�Ǥ�V6��S�ȤϤʤ���
GE #306 LAH, ȿ���ײ�ž��
���ǡ����Ʊ��������-30�Ǥ��뤫����ǤϿ��Ťˡ�
GE #307 LAH, CRRB, V1-3�ο���Q�ȡ�������ֹ��ɡ�
���ǡ�������ֹ��ɤˤĤ��Ƥϵ��Ҥʤ���
GE #308 �������륪���С���CRBBB��T�Ȥν���˵չ���P�ȡ�ƶ����̮
���ǡ�CRBBB�Ǥ�LVH��LAH�Ͽ��ǤǤ��ʤ����������륪���С����Ƥ��뤿���
LVH�Ȼפ��롥
GE #309 ��>90���ͻ趻�����Ű̡�V1��qR��V2-4��qrS, V5-6��RS��COPD�α������硥
���ǡ�4:1��AF��nodal��RVH�������а̤����Ṳ̋Ǥʤ����IRBBB������
���뤳�Ȥ��Ǥ��ʤ���������S�Ȥ����Ϻ�˦����Ƴ�Ȥ��ɤ�롥
GE #310 I,aVL���ȹ���LVH, IWMI��
���ǡ�LAD���LAH�ο��Ǥ뤫�ɤ�����������
GE #311 Af�ˤ�����STD��ȿ������
GE #312 V1-5�ΰ۾�Q�ȡ�V2-V6��STE��II,aVF��STE��������ֲ���AMI��
���ǡ�QRS 0.16������֥��å���������V1��R�Ȥ��������뤿���CRBBB��
V6�ޤ�STE������¦��AMI��V6�ޤ�STE�������II��aVF��STE�������η�̡�
V1��STD��ȿžT�ȤǤ��ꡤAMI��STE���ʤ���CRBBB���������AMI��
�����STE�ˤʤ롥cf ecg 15-13.
�������ڹ��ɤǤ�����T��ȿž�Ǥ�ST�徺�Ⱦ����T�Ȥˤʤ롥
tombstone�ȷ���GE #331��Ʊ����
GE #313 ��������� 20�������ϰϡ�
GE #314 II,III,aVF�ΰ۾�Q�ȡ��ͻ��ST�Ͽ�ʿ������QRS0.12, V1�Ϲ⤤R�ȡ�
ȿ���ײ�ž��V5-6�ΰ۾�Q�ȡ��Ť�����¦�ɹ��ɡ�V1��R�����ɹ��ɡ�
���ǡ�PR��Ĺ����-30, �Ť�����¦��h�����ɡ����ɤε��Ҥʤ���
GE #315 PR 0.2, III�Τ�Qr��, I,aVL�ι�R�ȡ�����ȿ���ײ�ž��NSSTWC, �������硥
���ǡ�V3-5��ST��sagging.
GE #316 I,aVL��ʿST��Tȿž��V1-4�Ͼ���̤�ST��Tȿž��V3��STE���������AMI��
���ǡ�Non-Q MI.
GE #317 SN��̮ PR 0.16, ���Τ�sagging ST������T�Ȥ����ΤǤʤ���V2-4��STD��
��̮�ˤ�����ȿ����
���ǡ��嵭�˲ä���V1-2�ϰ۾�Q�Ȥ�����������ֹ��ɤ����롥
GE #318 ��̮��CRBBB���Υ��������ץꥺ��
GE #319 normal.
GE #320 I,aVL��ʿST��T��ž��II,III,aVF��ʿST��V6��žT���������硥
���ǡ�NSSTWC.
GE #321 IWAMI, I,aVL�ߥ顼��V1-v5��ʿST������T�ȡ�V6STE��¦�ɤ�MI�ȵڡ�
���ǡ������Ȥ��̤�ECG�Ǥ��롥
GE #322 IRBBB,LAH
LAH��PRP��ȼ����PRP��V3-6��R/S������ä����ʤ����Ȱ�̣���롥
GE #323 #320��Ʊ����
GE #324 CRBBB+LAFB, II,III,aVF�ˤϾ�����R�Ȥ�¸�ߤ��롥
���ǡ�V1-3��r�Ȥ�̵���Τ�������ֹ��ɤ�ȼ�äƤ��롥
qR'����RBBB������������ֹ��ɤ���
GE #325 II,III,aVF��STD��SN��̮����˼��١�IRBBB��LongQT, V2-V6�����T�ȡ�
���ǡ���˲ä���PRû��LGL�ɸ�����PR 0.8��
GE #326 V1-6��rS�ȷ���P�Ȥ�¸�ߡ�QRS�λϤޤ�˥��ѥ�����DDD�ڡ�������̮��
GE #327 sagging ST, PAC,
���ǡ��������ꥹ���ǡ�
GE #328 SN, V1-4�ΰ۾�Q�Ȥ�STE���������AMI��
STE�Ͼ����ľ��Ū�Ǥ��ꡤ�����Ѳ��ǤϤʤ������������ɿ����
GE #329 V1�Dz�����P�ȡ�rS�����T��V2��rS��ST�徺��V3-6�ϰ۾�Q�Ȥ�ST�徺��
II,III,aVF��QR��ʿST�����������T�ȡ�����¦��AMI��
���ǡ��嵭�˲ä��Ʋ��ɤθŤ����ɡ�V1��P�Ȥ��LAA��
AMI���������ȷ�
GE #330 Wenckebach, V4-6��poor T.
���ǡ�II,III,aVF��Q�ȡ�STE��ȿžT�Ȥ��AMI��
GE #331 tombstone )�������ȷ�)
GE #332 �����а�V1��qR�ȷ����Դ������ӥ֥��å����¤�RVH��Eisemenger's.
V6�Ǥ�S�Ȥ��礭����V1��rsR'�ˤϤʤäƤ��ʤ���
GE #333 VͶƳ��ޤ���ͶƳ��STE -> ������� (��¡��Ѹ�ǤϾ�˸�����)
GE #334
GE #335
GE #336
GE #337
GE #338
GE #339
GE #340
GE #341
GE #342 1��AV �֥��å���ƶ����̮��PVC��LAFB��PRP��
���ǡ�PVC��2��̮��
GE #343 V1��QR'��V6��RS��CRRB��V2,V3���礭��QR'������������ֹ��ɡ�
����120����LPFB��II��P�Ȥϲ�������Junctional��0.12����ˤʤ뤫��
��˼ĴΧ�β�ǽ�����礭�������ɤ�ȼ��2�ޥ֥��å��Ǥ��뤫��
peri-infalction block�Ǥ��롥
�̾�qR����RBBB�Ǥ�V2�ʹߤ�R�Ȥ���Ԥ��뤫�鹼��Q�ȤǤ��롥
GE #344 I, aVL��STE��III, aVF��STE��V3-6��STE��¦�ɡ����¦��AMI��
���ǡ����Ʊ�������㡼�Ȥ�1���ܤ�PVC��
GE #345
GE #346
GE #347
GE #348
GE #349
GE #350
GE #351
GE #352
GE #353
GE #354
GE #355
GE #356
GE #357
GE #358
GE #359
GE #360
GE #361 I,aVL��STD��II,III,aVF��STE��V4-V6��STE�Ⱦ����ST�������ȡ�
�������ɹ��ɡ�I,aVL�ϥߥ顼����������ǥ����Ȥϴְ㤤��
GE #362
GE #363
GE #364
GE #365
���Τ����Purkinje�ϺǤ�Ĺ��æʬ�ˤ��Ƥ��롥�ޤ���TTX�����Ѥ��ʤ���
������HF��av1.8���礭����Ϳ���롥
��������Nav1.8
AF��Nav1.8
Shaker�Ȥϰ�����̾�Ǥ��ꡤ���ΰ����Ҥ������륿��ѥ���Shaker����ͥ�Ȥ�����
Shaker����ͥ�Ȥ�K, Rb, Se�ʤɤΥ��륫���°���̲᤹�륤�������ͥ�Ǥ��뤬��
���K����ͥ����4���ΤΥݥ�ڥץ��ɤǤ��롥
���ޤΤ褦��æʬ��(����)���Ƥ���Ǥ���ĸ�����Τ�Shaker�ǡ�
������ή���٤���Ʊ�����ĸ����٤��K����ͥ뤬���롥
IKur��KV1.5��IKr��KV11.1��IKs��KV7.1
(���������ͥ� A to Z p.62���)
IKur: Ķ��®�������ٱ���ή��K+����ͥ�
IKr: ��®�������ٱ���ή��K+����ͥ�
IKs: �˽��������ٱ���ή��K+����ͥ�
K+��ή�����鳰�����ǡ������Ǥ��롥
Shab��Shaw�ϳ������٤������ʤ��ʤ��ĸ����ʤ���
���ˡ�IKr��IKs���٤�롥
 wakaru3.1pdf p.41��ꡥ
wakaru3.1pdf p.41��ꡥ
IKur��Ķ��®�������ٱ���ήK����ͥ롧
IKr��KV11.1����̾hERG�Ǥ��롥wakaru3.1 p.59.
IKr�ϵ�®�������ٱ���ήK����ͥ롧
æʬ�˸夹������K��ή��ȯ��������ʬ�ˤ˸�������
�����������Ȥ�������Ʊ�����Գ����������ȤⳫ������
�ɷ㤬�����ȵդ�K��ή�����ʤ��ʤ�(0 V �ʾ�ξ��)��


IKs�ϴ˽��������ٱ���ήK����ͥ롧�¥�˥åȤ�minK���դ���
æʬ�˸夷�Ф餯���Ƥ���K��ή��ȯ��������ʬ�ˤ˸�������
KV7.1��IKs�Ǥ��롥�¥�˥åȤ�minK��ź�ä����ȡ���3-17�Τ褦��
���Ϥ��ٱ���ή�ˤʤꡤ��ʬ�ˤ���ǽ�ˤʤ롥(wakaru3.1 p.57)
��̮�ˤʤ��K��ή�γ������֤Τ����APD��û���ʤꡤ�Թ礬�褤��
(���Ѹ��� ���������ͥ� Ato Z p.65���)
���Τ��Ȥϵդ�LQT1�ξɾ��Ǹ��졤��̮��APD��û�̤��ʤ���
minK(KCNE1)��S5-S6�֤�p�롼�פ��������Ǥ��롥

�Ż��Ṳ̋����������ήK����ͥ�ϥ�������S5,S6�����ʤ�
�Ű̴�����S4���ʤ���S5,S6��M1,M2�ȸƤ֡�
p loop��������������������Ȥ�¸�ߤ��뤬��PIP2�ˤ��
��˳������֤Ǥ��롥����������˦����ˤʤ�ȡ����̤����������
�������ˤ�ꡤPIP2�����פ������η�̳����������Ȥ�
�ĺ����롥���Τ���˺�˦����Ǥ��Ż��Ṳ̋��徺���롥
(��¡���������ͥ� A to Z p.73���)
Lysophosphoglycerides������̮Ͷȯ����
���ڵ����K+����ͥ�
T-wave alternans��TWA�˸�����(������������)T��
T�Ȥ��ȹ⡤�ȷ����������Ѥ��ȷ�����
�������Ito���Գ���������β������٤�����˳�ư�Ű̻�³����(APD)��
�Ѳ��������롥��³���֤���Ĺ�����T�Ȥ��㤯��û�̤����T�Ȥ��⤤��
(���������ͥ� A to Z p.62)
T-wave alternans��TWA��
U wave LITFL
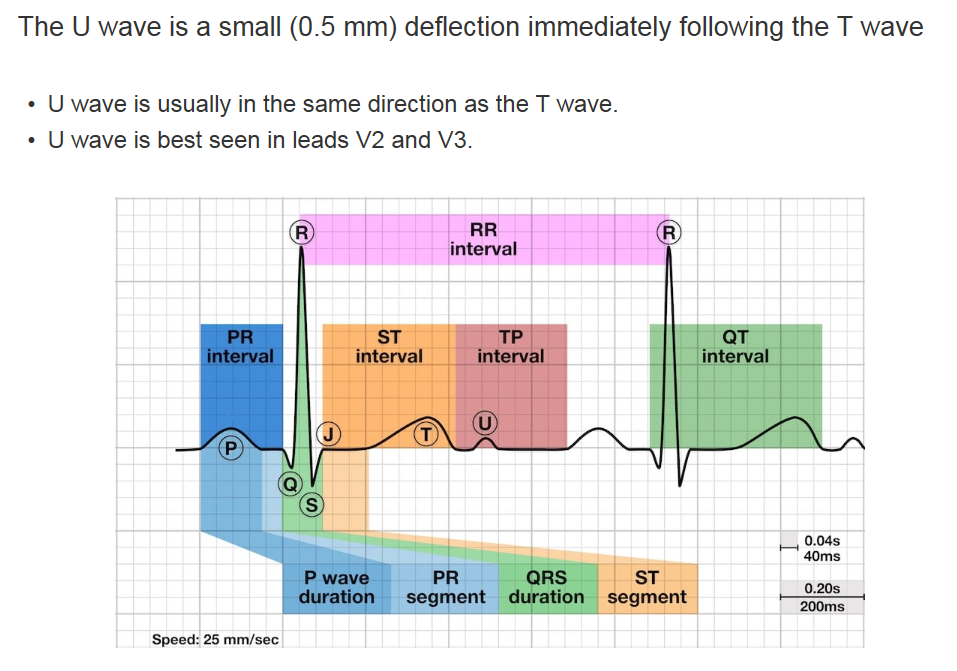 U�Ȥ�ȯ�������������Ǥ��뤬��Purkinje fiber���ٱ�����ʬ�ˡ�
M-cell���ٱ�����ʬ�ˡ�
�����ɤ�ʪ��Ū��ư�������Ƥ��롥
U�Ȥ�ȯ�������������Ǥ��뤬��Purkinje fiber���ٱ�����ʬ�ˡ�
M-cell���ٱ�����ʬ�ˡ�
�����ɤ�ʪ��Ū��ư�������Ƥ��롥
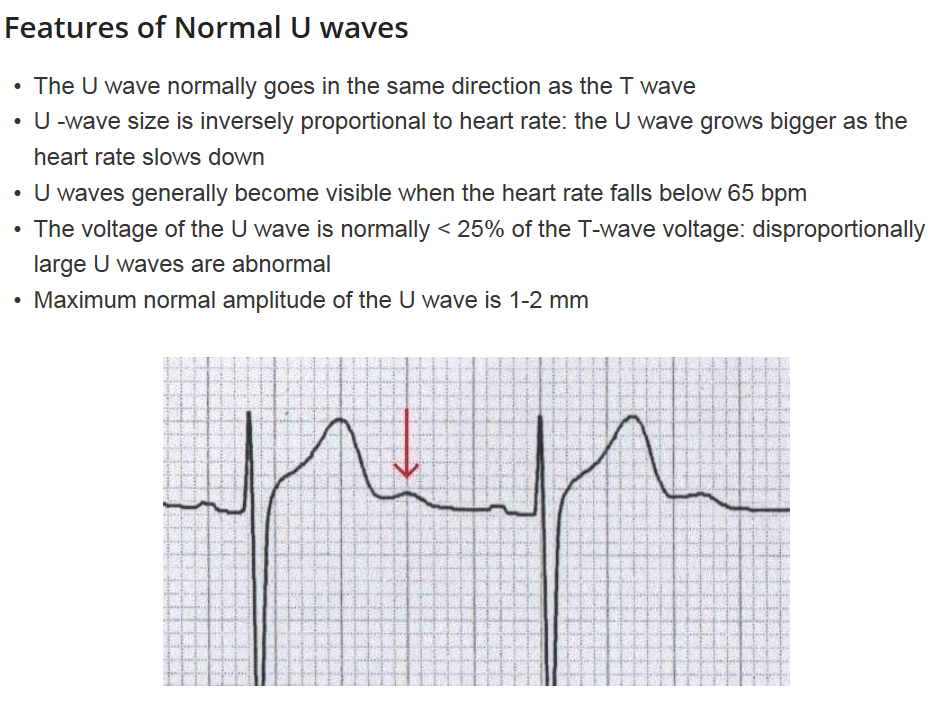 �۾�U�ȤȤϡ�
�۾�ˤ�������U�� (Prominent U waves)
>1-2mm �ޤ��ϡ� T�Ȥ� 25�۾�ι⤵��
������
����̮�����٤���K���
������¾����Ca��ɡ���Mg��ɡ����β���Ǿ��ж�ʡ��������硤���������ھ�
���������ˤ�
��Digoxin, Phenothiazines (thioiazine),
��Ia ������̮�� (quinidine, procainamide),
III ������̮�� (sotalol, amiodarone)
��žU�� (iInverted U waves)
������
����ư̮��������찵���ۼ�������ŷ�������������ھɡ���þ�����
��Prinzmetal angina(�۷�������)
U wave ��ư̮����
uwave.pdf
�۾�U�ȤȤϡ�
�۾�ˤ�������U�� (Prominent U waves)
>1-2mm �ޤ��ϡ� T�Ȥ� 25�۾�ι⤵��
������
����̮�����٤���K���
������¾����Ca��ɡ���Mg��ɡ����β���Ǿ��ж�ʡ��������硤���������ھ�
���������ˤ�
��Digoxin, Phenothiazines (thioiazine),
��Ia ������̮�� (quinidine, procainamide),
III ������̮�� (sotalol, amiodarone)
��žU�� (iInverted U waves)
������
����ư̮��������찵���ۼ�������ŷ�������������ھɡ���þ�����
��Prinzmetal angina(�۷�������)
U wave ��ư̮����
uwave.pdf
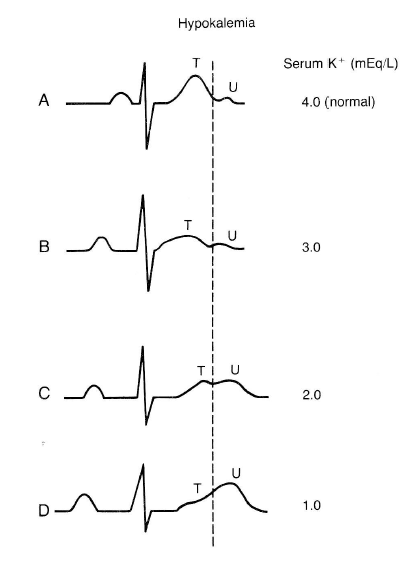 ��K��ɤˤʤ��U�Ȥ��и���PR�ֳ֤ϱ�Ĺ���롥
�̾����K��ɤ�U�Ȥ�ȯ�����뤬������ʳ���Ǿ�����ȯ�����롥
��K��ɤˤʤ��U�Ȥ��и���PR�ֳ֤ϱ�Ĺ���롥
�̾����K��ɤ�U�Ȥ�ȯ�����뤬������ʳ���Ǿ�����ȯ�����롥
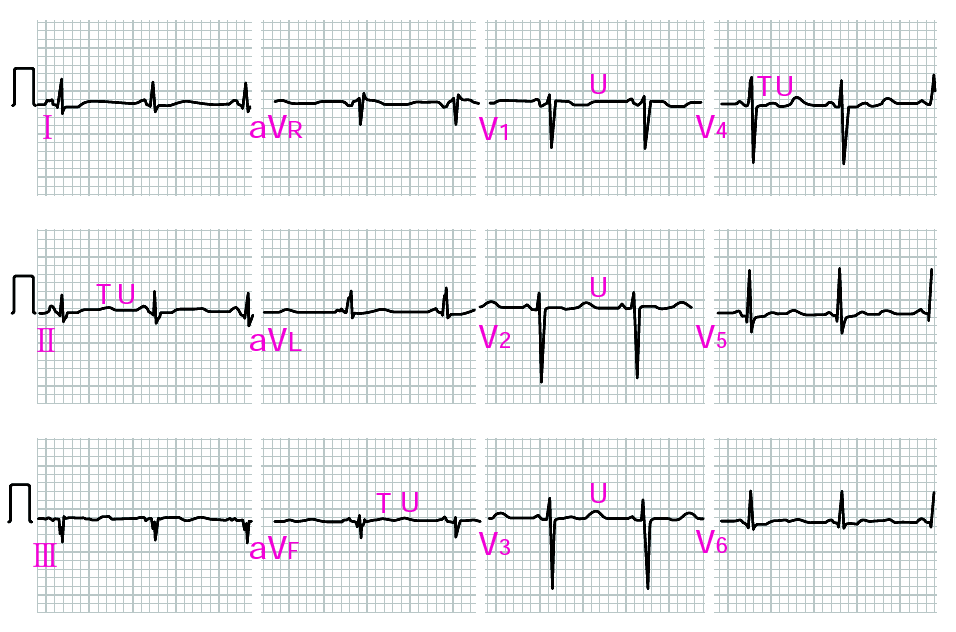 ����K+ǻ�٤�1.4mEq/L���㲼������ȯ������ɥ��ƥ��Ԥο��ſޡ�
Utah ECG Uwave
The U wave is the only remaining enigma of the ECG, and probably not for long. The origin of the U wave is still in question, although most authorities correlate the U wave with electrophysiologic events called "afterdepolarizations" in the ventricles. These afterdepolarizations can be the source of arrhythmias caused by "triggered automaticity" including torsade de pointes. The normal U wave has the same polarity as the T wave and is usually less than one-third the amplitude of the T wave. U waves are usually best seen in the right precordial leads especially V2 and V3. The normal U wave is asymmetric with the ascending limb moving more rapidly than the descending limb (just the opposite of the normal T wave).
����K+ǻ�٤�1.4mEq/L���㲼������ȯ������ɥ��ƥ��Ԥο��ſޡ�
Utah ECG Uwave
The U wave is the only remaining enigma of the ECG, and probably not for long. The origin of the U wave is still in question, although most authorities correlate the U wave with electrophysiologic events called "afterdepolarizations" in the ventricles. These afterdepolarizations can be the source of arrhythmias caused by "triggered automaticity" including torsade de pointes. The normal U wave has the same polarity as the T wave and is usually less than one-third the amplitude of the T wave. U waves are usually best seen in the right precordial leads especially V2 and V3. The normal U wave is asymmetric with the ascending limb moving more rapidly than the descending limb (just the opposite of the normal T wave).
Persistent giant U wave inversion with anoxic brain injury
����Ǿ�����ǤϾ������U�Ȥ�ȯ��������찵�ʤɤν۴Ľ����Ǥϲ�������U�Ȥ�ȯ�����롥
����ϵ���Ǿ�����Ǥβ�������U�Ȥ���Ǥ��롥�ߴɤ�ȴ����U�ȤϾä�����
uwave/uw1.png
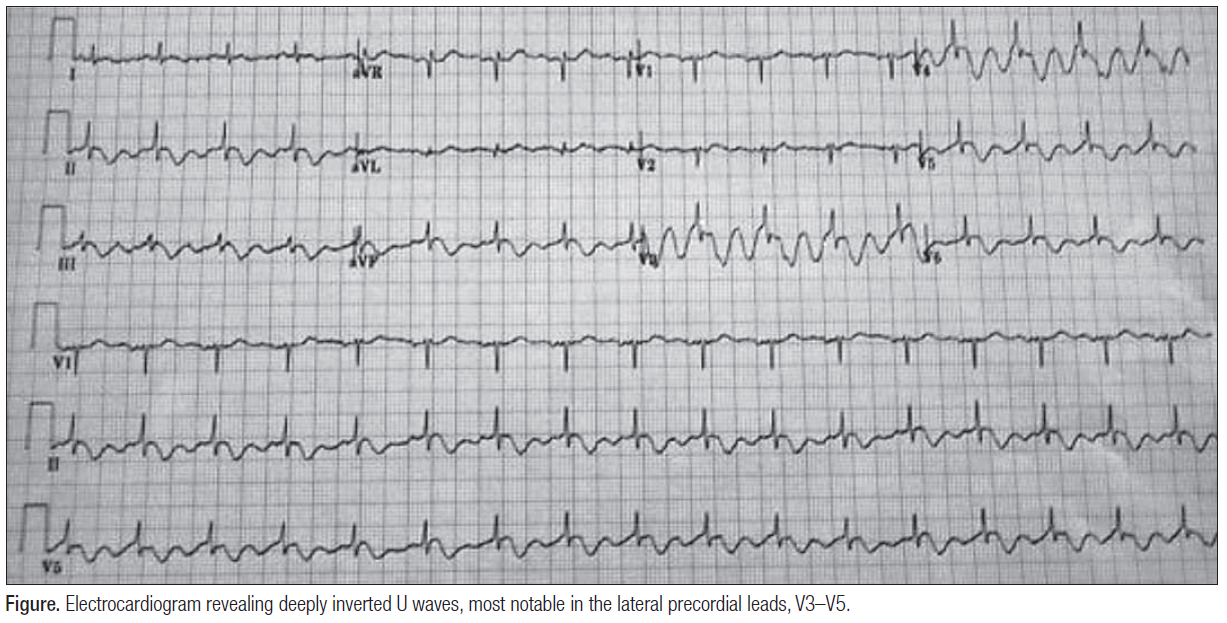 Giant U waves: an important clinical clue
The patient U wave
Book�����Ѥ���U�ȵ���
Google:
Hypothesis 2: delayed repolarization
���Ǥ�����줿������
uwave/uwave1.png
Giant U waves: an important clinical clue
The patient U wave
Book�����Ѥ���U�ȵ���
Google:
Hypothesis 2: delayed repolarization
���Ǥ�����줿������
uwave/uwave1.png
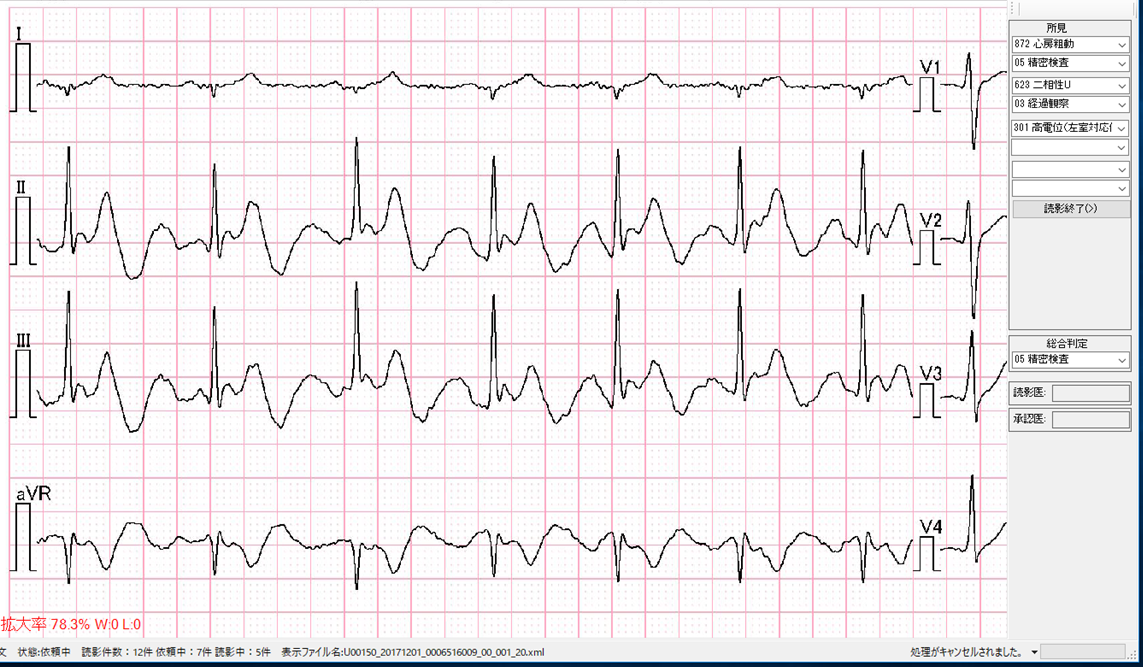 uwave/uwave2.png
uwave/uwave2.png
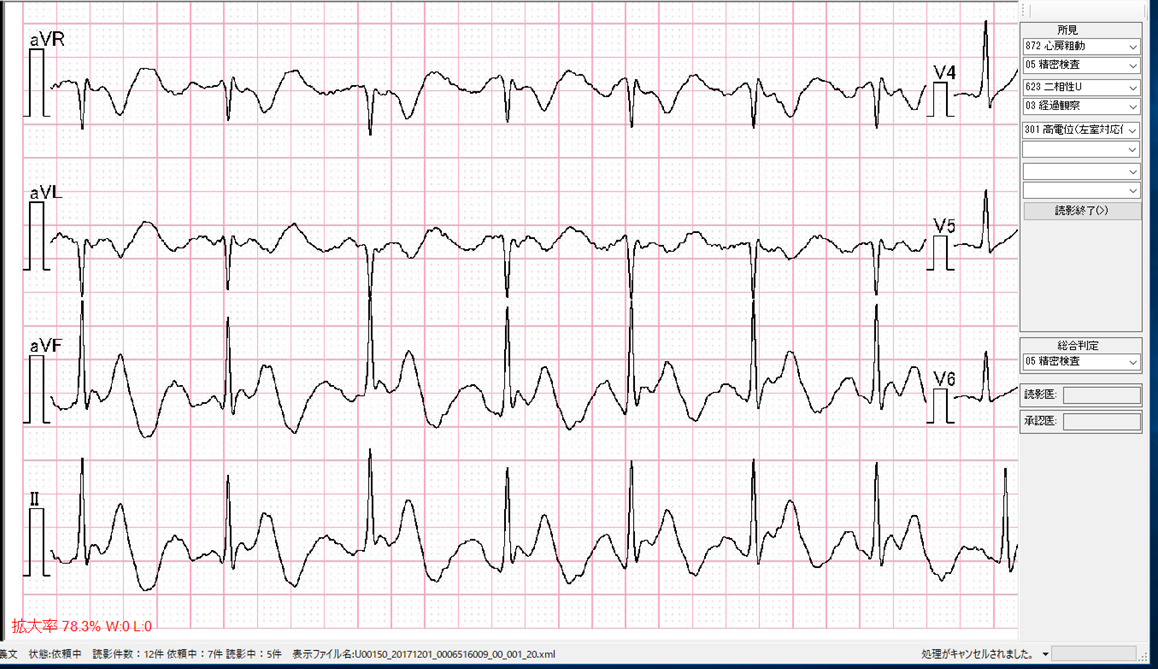 uwave/uwave3.png
uwave/uwave3.png
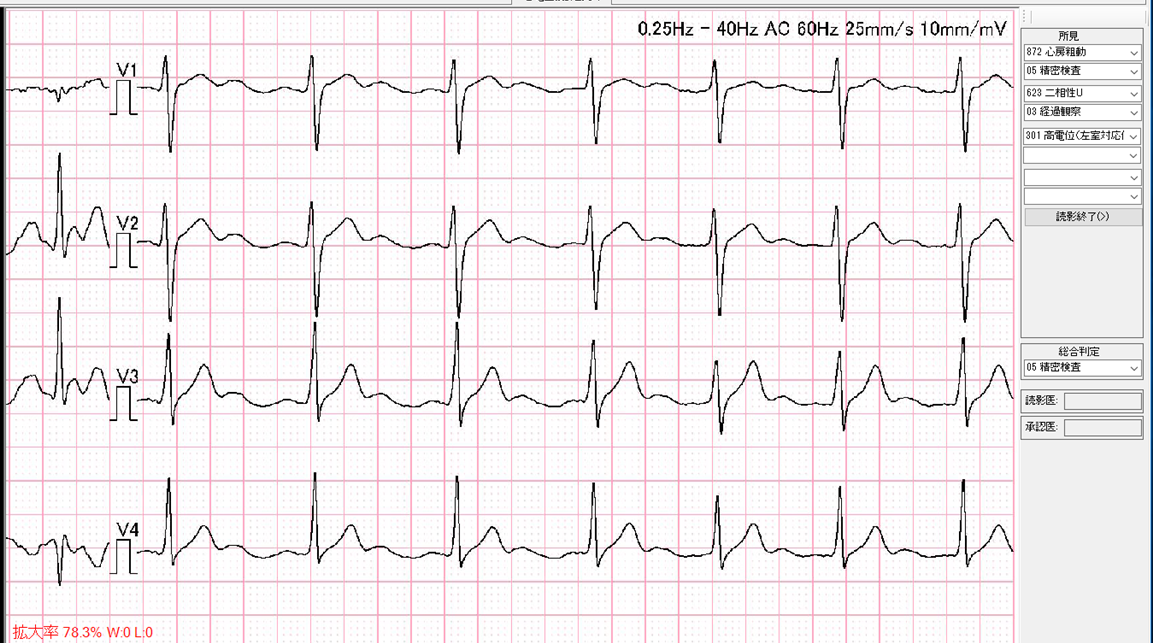 uwave/uwave4.png
uwave/uwave4.png
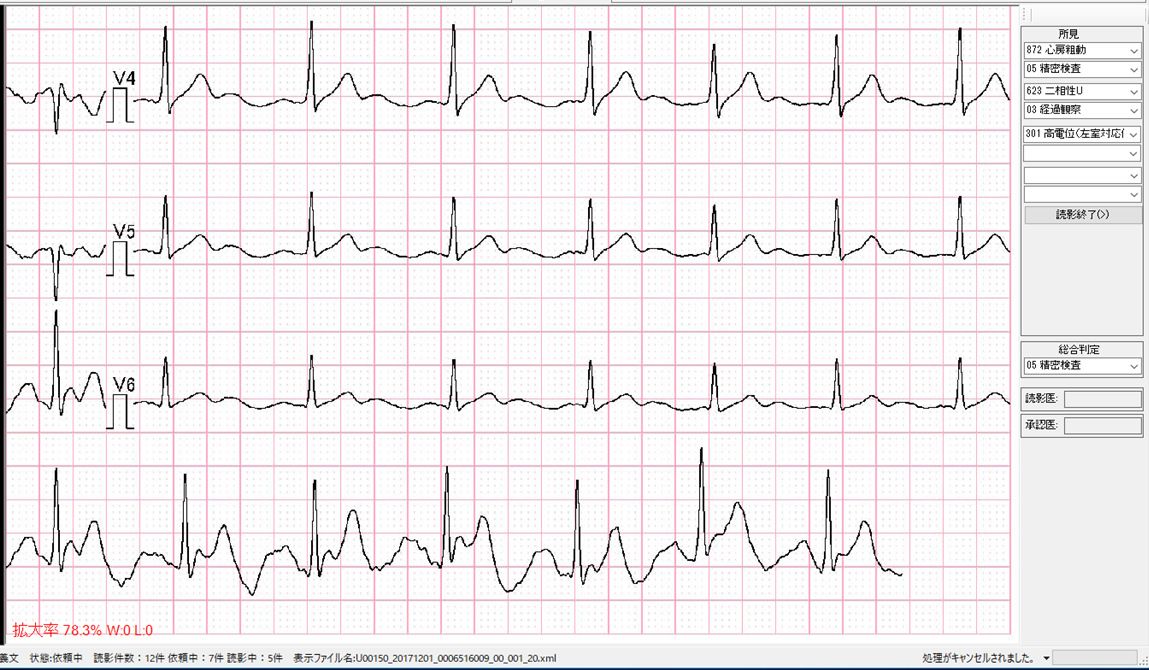
Ŭ�ڤ���Ū���ץ������ˤ��J�Ⱦɸ����ο���
�ޤ����ʬ����褦��0.2mV�ʾ��J���Υå��ϴ����������ST�������Ȥ�
��ʿ��ʬ���ʤ��������˾徺���Ƥ����ͻҤϿ�����¦���ڤ������ʬ�ˤ�
�����Ǥ���Phase 2��R on T��ȯ�����פ��ʤ롥
 35_195.pdf��ꡥJ�ȤϥΥå��ͤǤ��롥����ľ��������T�ȤˤʤäƤ��ꡤ
��ʿ��ʬ���ʤ���0:00�Ǥ�J�ȤϾ�������2:00���礭����Ĺ���Ƥ��롥
3:00�Ǥ�T�Ȥν�λ����R�Ȥ�ȯ�������줬R on T�Ǥ��ꡤvf�˰ܹԤ��롥
���͡�final p.76 Ito�ˤ���ʬ�ˤ�Brugada 2�����롥
35_195.pdf��ꡥJ�ȤϥΥå��ͤǤ��롥����ľ��������T�ȤˤʤäƤ��ꡤ
��ʿ��ʬ���ʤ���0:00�Ǥ�J�ȤϾ�������2:00���礭����Ĺ���Ƥ��롥
3:00�Ǥ�T�Ȥν�λ����R�Ȥ�ȯ�������줬R on T�Ǥ��ꡤvf�˰ܹԤ��롥
���͡�final p.76 Ito�ˤ���ʬ�ˤ�Brugada 2�����롥
lqt.gif
early repolarization syndrome
early1.gif
�����ʬ�˾ɸ�����12ͶƳ
early2.gif
�����ʬ�˾ɸ�����R on T
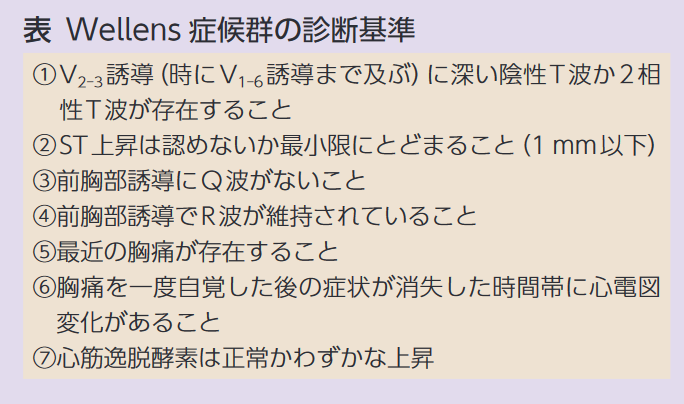
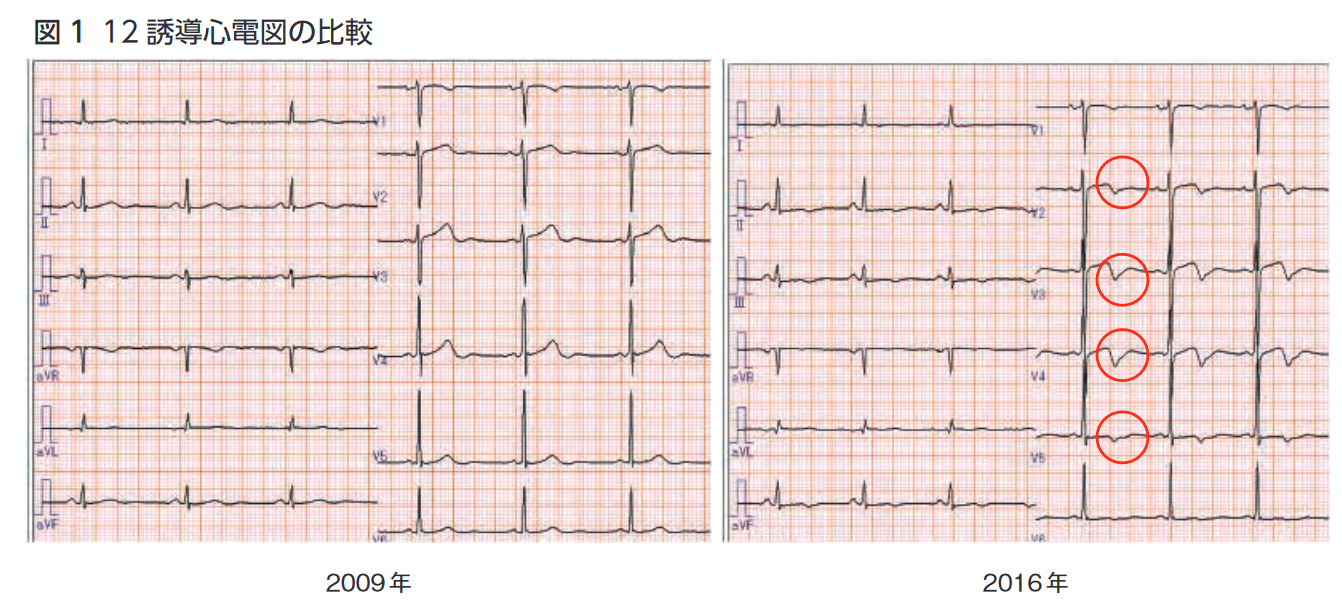 ������Ǥ���������Wellens�ɸ�����3����
������Ť��ΤäƤ�������Tips
Rhinehardt J, et al. Electrocardiographic manifestations of Wellens�� syndrome. Am J Emerg Med. 2002;20��7��:638-43.
����Wellens�ɸ����ˤĤ��Ƥ���ʸ
������Ǥ���������Wellens�ɸ�����3����
������Ť��ΤäƤ�������Tips
Rhinehardt J, et al. Electrocardiographic manifestations of Wellens�� syndrome. Am J Emerg Med. 2002;20��7��:638-43.
����Wellens�ɸ����ˤĤ��Ƥ���ʸ
Brugada�ɸ�����ȯ������
GE #331 (tombstone) IMG_20180625_0002-a.png
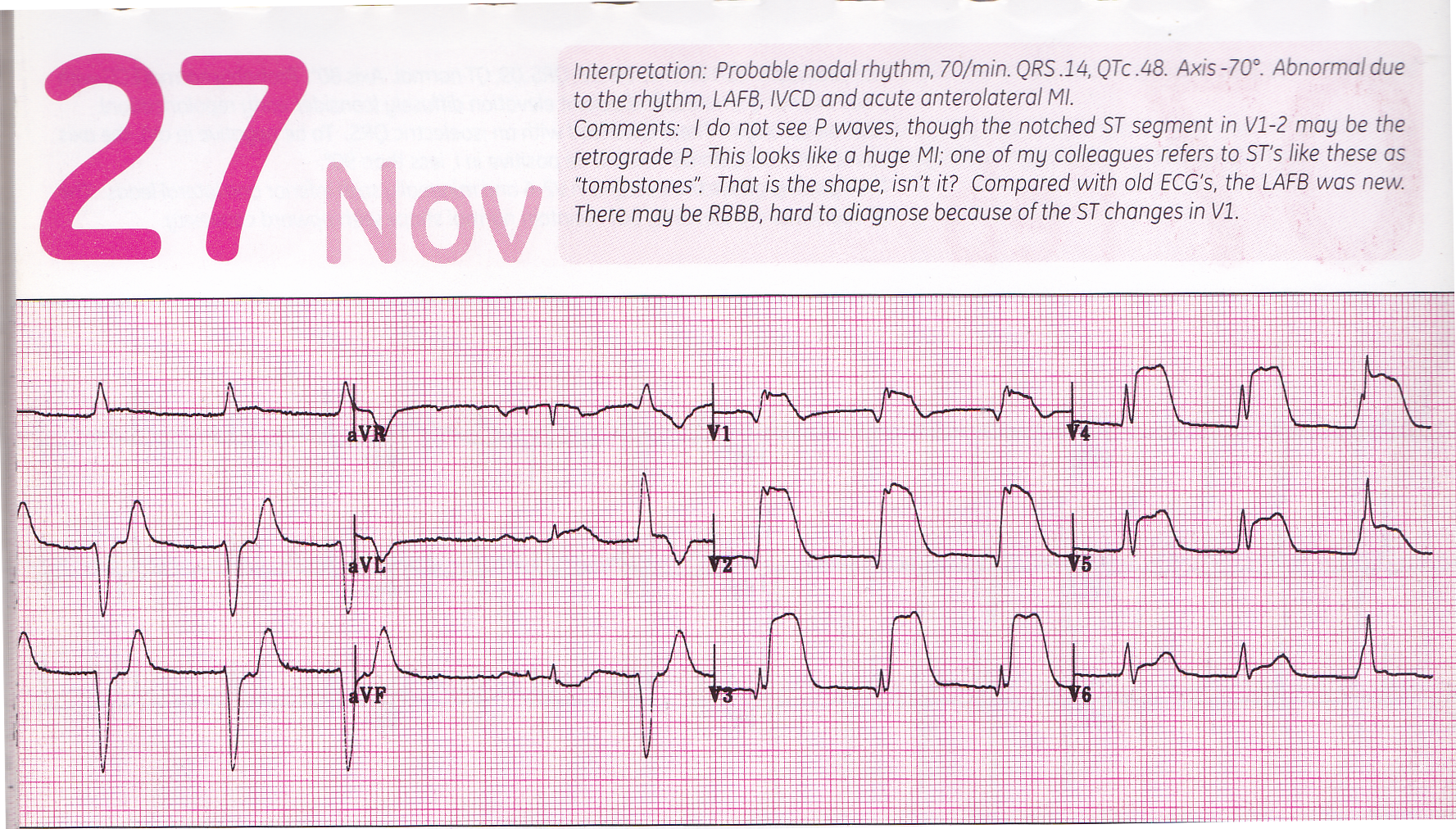 GE #312 (tombstone) IMG_20180625_0001-a.png
GE #312 (tombstone) IMG_20180625_0001-a.png
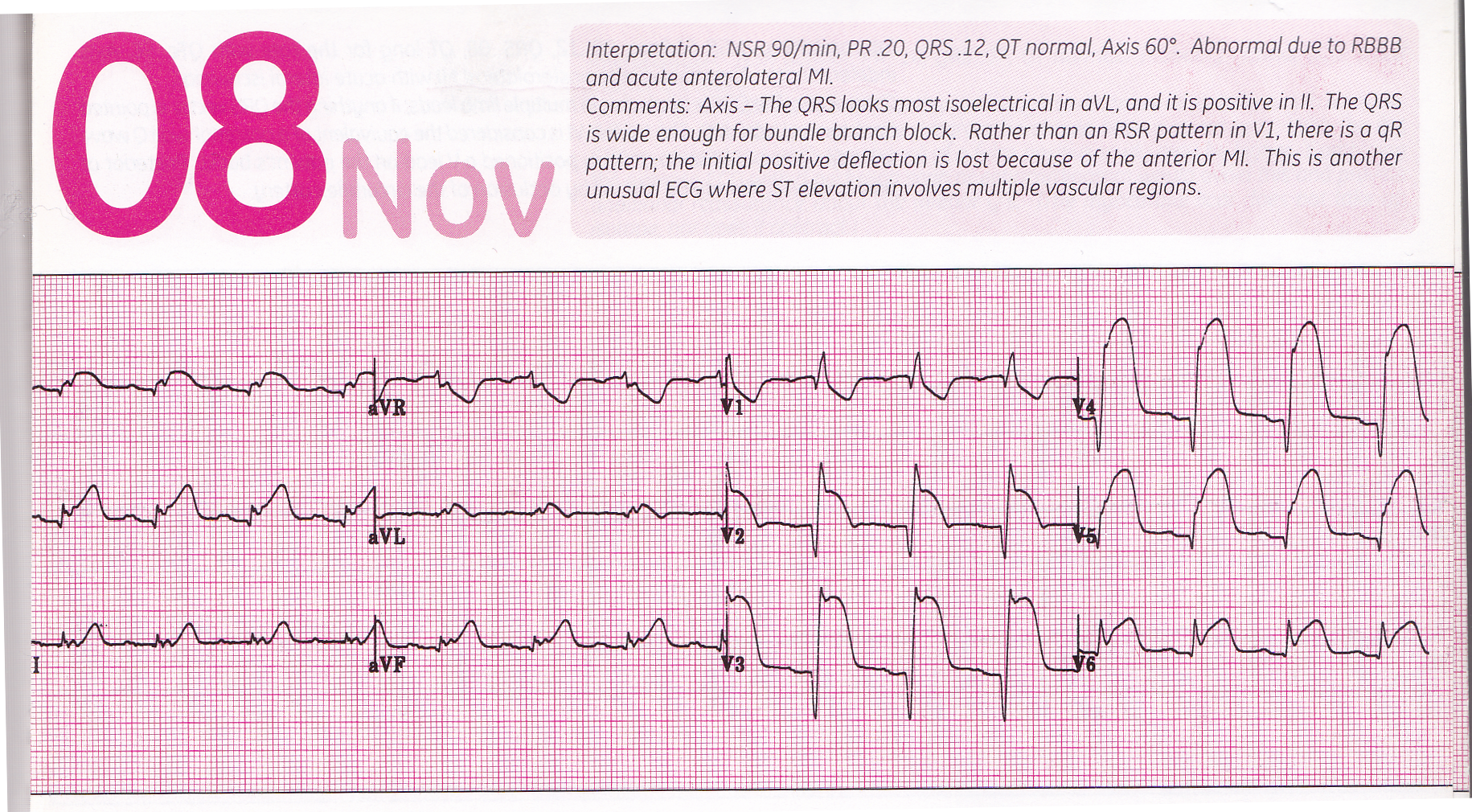
uwave/delta1.png
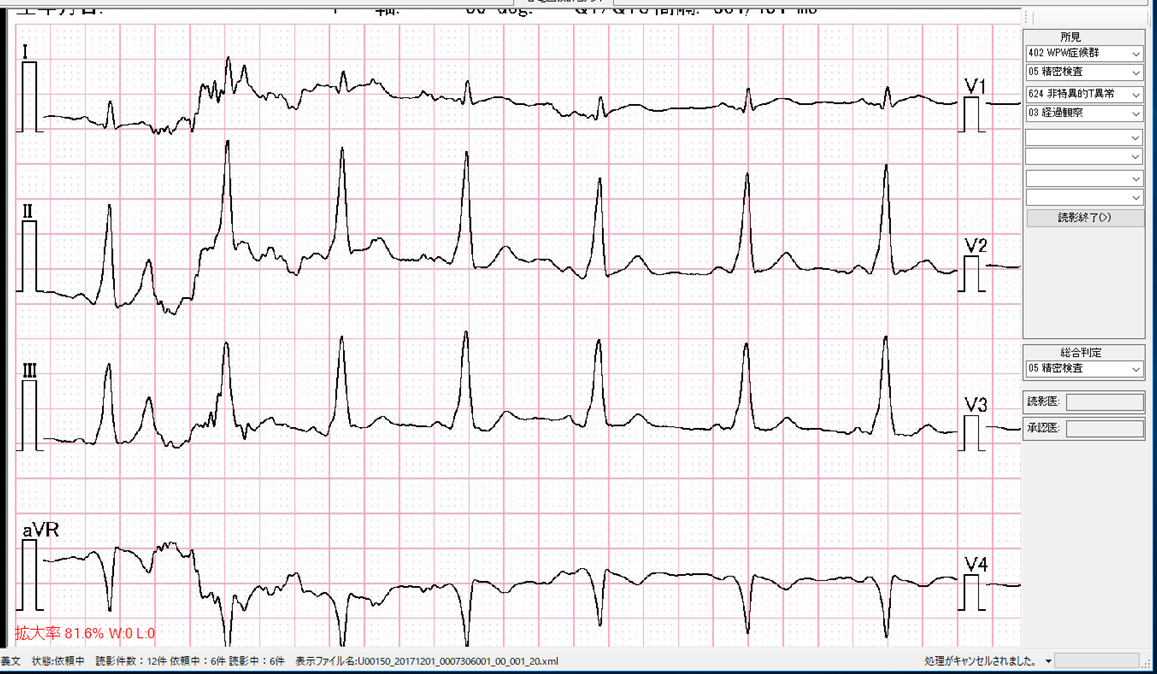 uwave/delta2.png
uwave/delta2.png
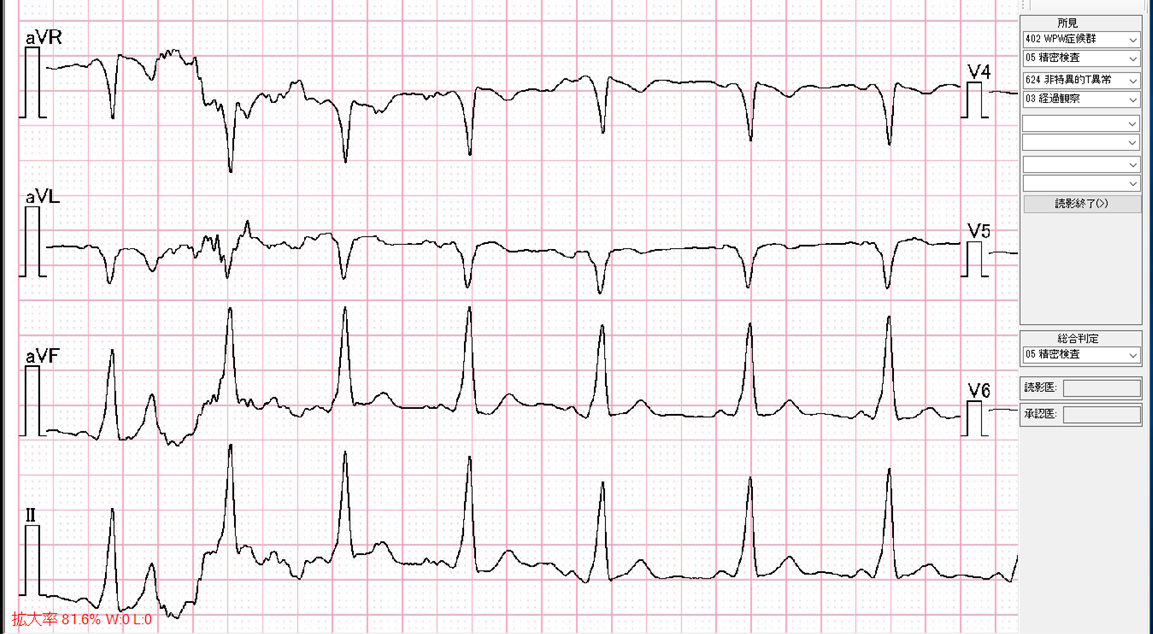 uwave/delta3.png
uwave/delta3.png
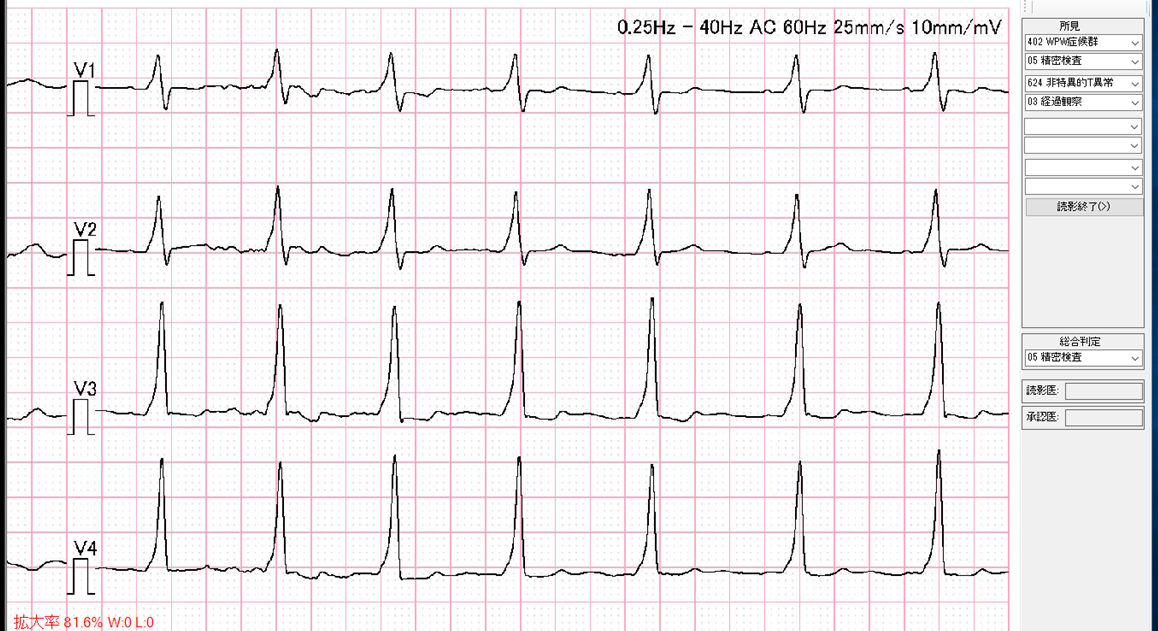 uwave/delta4.png
uwave/delta4.png
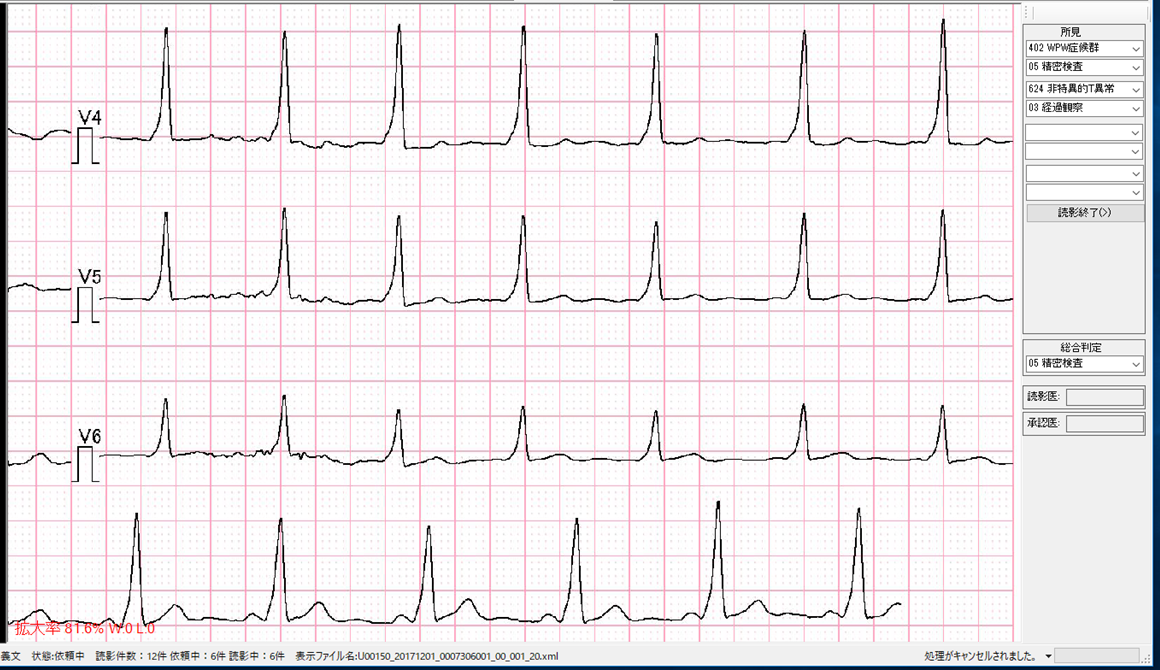
https://www.ionadventure.com/content.html
�ɲû������������ͥ�
Mechanisms of sodium channel inactivation
google sodium inactivation bedside cell physiology
���������ͥ롡�ǡ����١���
http://www.guidetopharmacology.org/GRAC/FamilyIntroductionForward?familyId=82
�� ���������ͥ�ϻ����������̤����쥿��ѥ��ǡ���˹��������Ƥ��롥
�������������Ϲ����礭������ޤꡤk+ < Na+ < Ca++�Ǥ��롥�������äơ�
K����ͥ��k+�������̲ᤷ�ʤ�����Na����ͥ�� k+��Na+�������̲᤹�롥
��˦���ˤ�˭�٤�Na+�����ꡤk+�Ͼ��ʤ���
�ޤ�������ͥ���ϡݤ����Ť��Ƥ��뤿�ᡤ�ۥ�������Ф��ƾ�۰��Ϥ���ġ�
���äơ�Na����ͥ��Na+��ή�����䤹�����֤ˤ��롥
����������Ca++������ˤĤ��Ƥ�Ʊ�ͤǤ��ꡤCa����ͥ볫�����ˤ�
Na+�������Ʊ����ή�����롥����Na+��æʬ�˻��ξ㳲�ˤϤʤ�ʤ���
Na����ͥ�
Heartland p.163
Readers will understand and retain
how the heart functions at the ionic-molecular level including:
�� The teleology of the ion-kinetic mechanisms of the ionic-molecular microcosm
�� How three little ions produce conduction through, and contraction of, the heart
�� The simple ionic mechanism of cell-to-cell myocardial conduction
�� How ion movement translates into vectors
�� The movement of ions that produces EKG recordings
�� How the atria contract without backflow into the great veins and pulmonary veins
�� Why there are automaticity foci in the large vein ostia of the atria
�� The homeostatic necessity of automaticity foci in emergency situations
�� A simplified methodology for understanding autonomic function
�� How troponin components participate in myocyte contraction and relaxation
�� TnC, TnI, and TnT function
�� Size of ions matters
�� Why ion-kinetic (ion-moving) structures like ion channels are essential to cell function
�� How the ion pumps produce the gradients that drive ions through ion channels and ion exchangers
�� Evolution of the Na/Ca ATPase pump
�� How the Autonomic Nervous System (ANS) controls ion-kinetic structures by phosphorylation and dephosphorylation
�� The nature of sympathetic stimuli and parasympathetic inhibition on the ionic-molecular level
�� Voltage versus ligand activation of ion channels
�� The peculiar Cl- channels and their purpose during the Action Potential
�� How ion channels select certain ions
�� How Ca++ ions produce myocyte contraction on the ion level
�� The function of the CICR
�� How the CICR produces effective myocyte contraction and generates an outward Ca++ ion gradient
�� The necessity of ryanodine Ca++ channels
�� The tandem function of L-type and ryanodine-type Ca++ channels
�� How the sarcoplasmic reticulum (SR) functions
�� How the SR stores and releases Ca++ ions
�� How myocytes employ Ca++ binding proteins
�� The ionic-molecular function that initiates and maintains the myocyte power stroke
�� Why T tubules are necessary in the myocyte yet absent from Purkinje cells
�� Why myocytes need both superficial and deep cisternae
�� The ionic-molecular physiology of myocyte relaxation (diastole) following contraction (systole)
�� Why both the cell membrane and the sarcoplasmic reticulum need Ca++ ATPase pumps
�� The functions of Na/Ca exchangers
�� How and why Na/Ca exchanger function is linked to Na+ channel function
�� Explanation of why Na/Ca exchanger function fluctuates during the Action Potential
�� Although the cell membrane Ca++ATPase pump and the Na/Ca exchanger remove free Ca++ ions from the myocyte, most Ca++ ions go elsewhere
�� Why the myocardium acts like a syncytium to conduct with negligible resistance
�� Why gap junction terminology is being replaced by the more specific connexon/connexin protein model
�� How gradients move ions through connexons
�� The exact nature of cell-to-cell conduction
�� The fascinating mechanisms of cell-to-cell depolarization
�� How ion channel threshold potential perpetuates cell-to-cell conduction
�� Homeostatic function of the Na/H pump and its emergency response
�� How myocytes, AV node cells, and Purkinje cells depolarize
�� How advancing Na+ ion waves produce the vectors of myocardial conduction
�� The nature of \u201cfast\u201d and \u201cslow\u201d Na+ currents
�� The anatomy, physiology, and kinetics of Na+ channel opening
�� Why ion channel flow is described in terms of open probability
�� Why ion channel function requires three operational states
�� The necessity of closed versus inactivated ion channel status
�� The specific peptide loop dynamics of fast and slow inactivation
�� Why ion channels have periods of refractoriness and responsiveness
�� The clinical importance of ion channel recovery from inactivation
�� The ionic-molecular dynamics of repolarization
�� How K+ channels repolarize the myocyte to baseline potential
�� Methodology of rectification of ion channel currents; how and why
�� The repolarizing K+ channels and the K+ channels that maintain baseline potential
�� The teleology of the delayed-rectifier K+ channels
�� The physiological reason for the extended plateau of the action potential
�� IK1 function and baseline potential
�� The ion-kinetic structures that participate in the plateau
�� The pathophysiology of Long QT (LQT) syndromes
�� Autonomic modulation via G protein intermediaries
�� How autonomic function affects automaticity
�� How autonomic function affects myocardial conduction and contraction
�� How the autonomic nervous system (ANS) regulates AV node conduction
�� Discovery of the ionic-molecular etiology of Wenckebach conduction
�� ANS input via sensor-receptors provides the data for cardiac homeostasis
�� How sympathetic and parasympathetic receptors modulate the function of ion-kinetic structures
�� How sympathetic and parasympathetic receptors affect each other\u2019s function
�� How parasympathetic influence interferes with sympathetic phosphorylation of ion-kinetic structures
�� Bouton-bouton parasympathetic inhibition of sympathetic stimulation
�� Parasympathetic inhibition of sympathetic ganglia
�� G protein participation in phosphorylation and dephosphorylation activity
�� Adenosine \u2013 where and why it originates, and how it works
�� Phospholamban and Ca++ sequestration in the sarcoplasmic reticulum
�� Homeostatic parasympathetic-sympathetic interaction and interdependance
�� Wenckebach conduction as vital homeostatic emergency mechanism
�� How K+ channel modulation modifies the action potential and affects the heart
�� The function of A1 receptors and M2 receptors
�� Na/K ATPase pumps produce and maintain of K+ and Na+ gradients
�� The AV node as a homeostatic necessity
�� Filtering effects of the AV node
�� The role of automaticity foci
�� Why AV node cells lack Na+ channels, but Na+ ion influx initiates AV node depolarization
�� How Ca++ channels select Ca++ ions from a sea of Na+ ions
�� Ca++ channel: structural kinetics of activation
�� Fast and slow inactivation kinetics of Ca++ channels
�� Slow AV node conduction at the ionic-molecular level
�� Calmodulin-assisted fast inactivation of Ca++ channels
�� Peptide loop slow inactivation of Ca++ channels
�� Sympathetic stimulation of ion-kinetic structures of AV node cells and their parasympathetic inhibition
�� Parasympathetic IK(ACh) channel activation inhibits AV node conduction
�� Purkinje cell conduction and the ventricular conduction system
�� Ionic-molecular mechanisms that facilitate rapid conduction through Purkinje cells
�� Na+ channel and Na/Ca exchanger participation in Purkinje depolarization
�� Refractoriness of Purkinje cells and Mobitz AV block
�� How Mobitz block at normal sinus rates or high degree Mobitz block causes dangerous bradycardia
�� Purkinje repolarization and K+ channel activity
�� The relation between Purkinje depolarization and conduction
�� Ionic-molecular explanation of refractoriness of the ventricular conduction system
�� LQT3 and Na+ channel function
�� Autonomic regulation of the SA node and automaticity foci
�� Autonomic sensor-receptors and SA node homeostasis
�� The ion-kinetic structures of the P (pacing) cells of the SA node
�� Autonomic modulation of P cell pacing
�� Sympathetic/parasympathetic modulation of ion-kinetic structures of the SA node
�� IK(ACh) channels and parasympathetic inhibition of the sinus pacing rate
�� Ion-kinetic structures are responsible for every aspect of cardiac physiology and pathophysiology.
---------------------------------------------------
 final p.18���
final p.18���
 final p.136���
final p.136���
��Ca��ɤǤ�2��ץ�ȡ��꤬û�̤���ST��û�̡�QT��û�̡�U�����礬�����롥
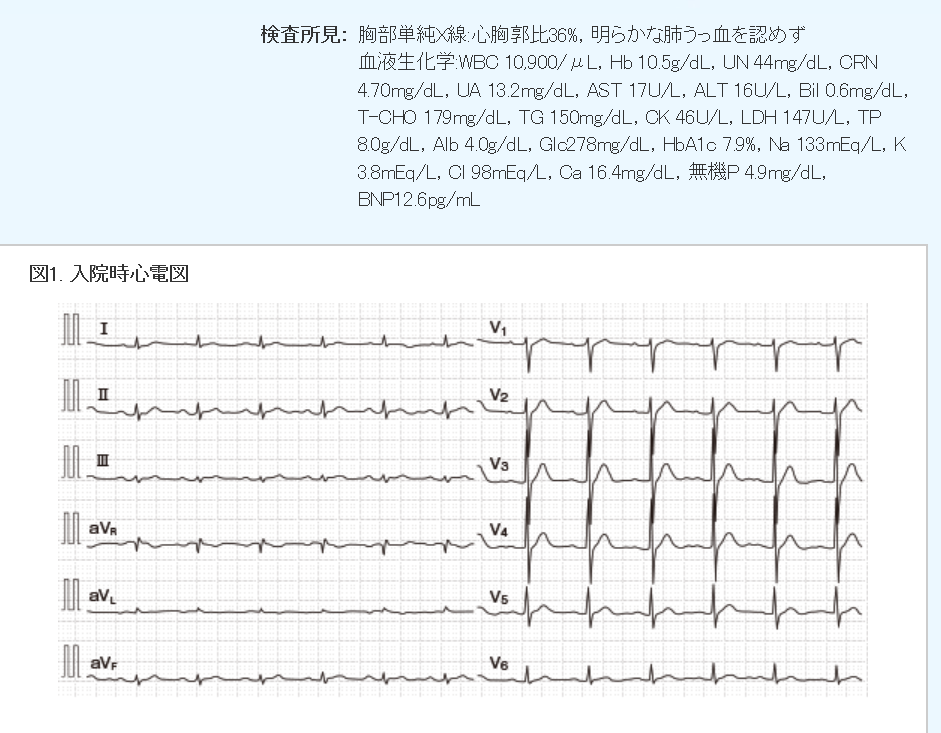 Ca�����������塤16.4mg/dl����10.2mg/dl�ˤʤä������ޤ��Ѳ��Ϥʤ���
Ca�����������塤16.4mg/dl����10.2mg/dl�ˤʤä������ޤ��Ѳ��Ϥʤ���
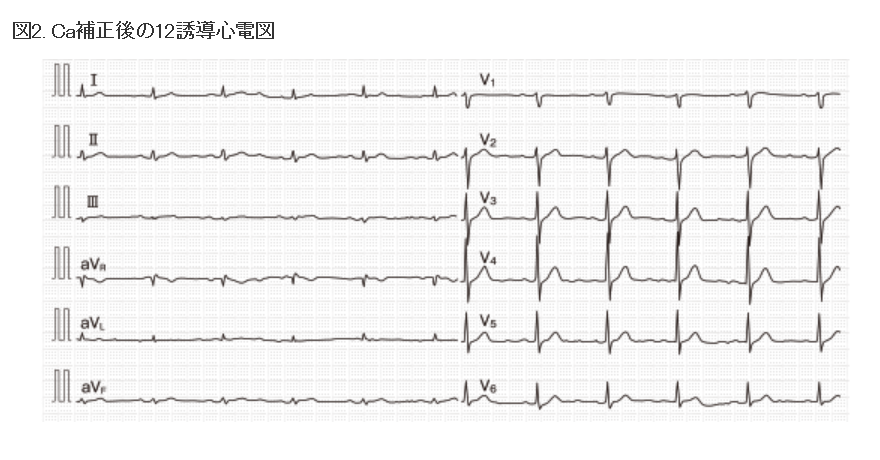
�ܼ�����롣
 II < 0 �ʤ� -30��ʲ�
III <0 �ʤ� 30��ʲ�
II < 0 �ʤ� -30��ʲ�
III <0 �ʤ� 30��ʲ�
II < 0 �ʤ� -30��ʲ� III <0 �ʤ� 30��ʲ�
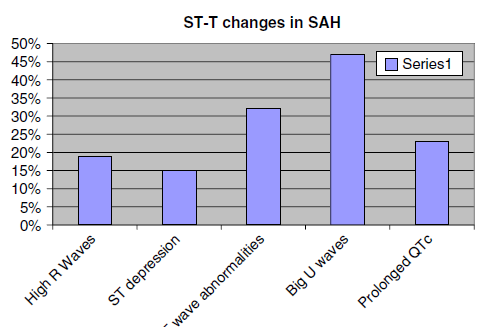
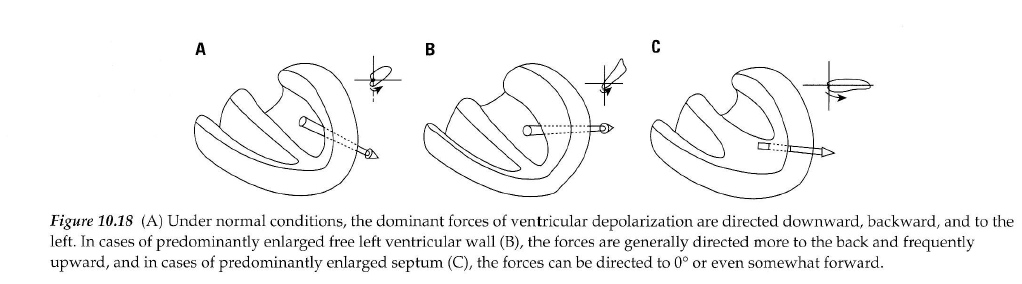 Luna��� A�����B�Ϻ�����ͳ�ɤ������C�Ϻ�����֡����������������p.138
Luna��� A�����B�Ϻ�����ͳ�ɤ������C�Ϻ�����֡����������������p.138
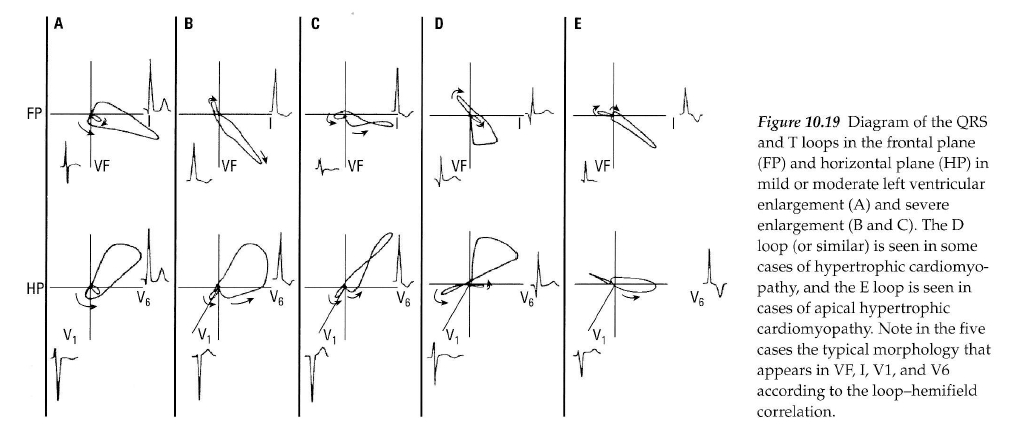 Luna��� ��������Υ٥��ȥ뿴�ſ� p.138
Luna LVH.pdf
V1�ޤ���V2��S�Ȥ�V5�ޤ���V6��R�Ȥ��¤���35mm�ʾ塥
�ɤ줫�ζ���ͶƳ����45mm�ʾ塥
aVL��R�Ȥ���11mm�ʾ塥
I��R�Ȥ���12mm�ʾ塥
aVF��R�Ȥ���20mm�ʾ塥
�嵭�Τɤ줫����������Ⱥ�������ޤ��Ϻ�����ĥ�Ǥ��롥
(PRD(PR�ֳ֤β��ߤ�0.8mm�ʲ��ʤ�����Ǥ��롥p.180)
11-4 ��������ˤ��LVH
11-5 ������ĥ�ˤ��LVH��I, II, III, aVF, V5, V6�Ǥ�
1mm�ʲ��ξ�����Q�ȤϺ�����ĥ����ħ��
������˱���ST�������Ȥ�T�Ȥϥ��ȥ쥤��(strain)�ȷ��Ǥ��롥
11-6 ŵ��Ū��LVH�ǤϤʤ���U��
11-7 �������Ű̡��ͻ�ͶƳ�Υե�åȤ�T�ȡ����ð�ŪST�Ѳ�
11-8 LVH, ���ȥ쥤��ѥ������žT�ȡ�
V1, V2��concave upward T�ȡ�V3�Ͼ����ST�����ǵ�žT�ȡ��褤��Ǥ��롥
11-9 LGL�ɸ�������̮��LVH������P�ȤǤϤʤ���
11-10 LVH, RAE, LAE, late intrinsicoid deflection, GE #298
I��R�Ȥ����˥��������������롥II�˦����ͤˤߤ��뤬WPW�ǤϤʤ���
11-11 RAE��LAE��LVH���ͻ�ͶƳ��flat��T�ȡ����ð�ŪST�Ѳ���
Luna��� ��������Υ٥��ȥ뿴�ſ� p.138
Luna LVH.pdf
V1�ޤ���V2��S�Ȥ�V5�ޤ���V6��R�Ȥ��¤���35mm�ʾ塥
�ɤ줫�ζ���ͶƳ����45mm�ʾ塥
aVL��R�Ȥ���11mm�ʾ塥
I��R�Ȥ���12mm�ʾ塥
aVF��R�Ȥ���20mm�ʾ塥
�嵭�Τɤ줫����������Ⱥ�������ޤ��Ϻ�����ĥ�Ǥ��롥
(PRD(PR�ֳ֤β��ߤ�0.8mm�ʲ��ʤ�����Ǥ��롥p.180)
11-4 ��������ˤ��LVH
11-5 ������ĥ�ˤ��LVH��I, II, III, aVF, V5, V6�Ǥ�
1mm�ʲ��ξ�����Q�ȤϺ�����ĥ����ħ��
������˱���ST�������Ȥ�T�Ȥϥ��ȥ쥤��(strain)�ȷ��Ǥ��롥
11-6 ŵ��Ū��LVH�ǤϤʤ���U��
11-7 �������Ű̡��ͻ�ͶƳ�Υե�åȤ�T�ȡ����ð�ŪST�Ѳ�
11-8 LVH, ���ȥ쥤��ѥ������žT�ȡ�
V1, V2��concave upward T�ȡ�V3�Ͼ����ST�����ǵ�žT�ȡ��褤��Ǥ��롥
11-9 LGL�ɸ�������̮��LVH������P�ȤǤϤʤ���
11-10 LVH, RAE, LAE, late intrinsicoid deflection, GE #298
I��R�Ȥ����˥��������������롥II�˦����ͤˤߤ��뤬WPW�ǤϤʤ���
11-11 RAE��LAE��LVH���ͻ�ͶƳ��flat��T�ȡ����ð�ŪST�Ѳ���
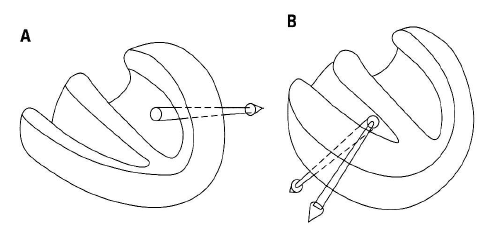 A�����B�ϱ������硥
��������ˤ��ŵ������������а̤ȸ屦���а̤���Ȥ��꤬���롥
�������ϱ��ӥ֥��å�����R'���礭����
��������V1��rS�ˤʤ롥��������������V6��S�Ȥ��礭����
S1S2S3�ϸ����������꼴�Ȥʤ롥
�Ǥ�����Ū���������Ƥ��롥
A�����B�ϱ������硥
��������ˤ��ŵ������������а̤ȸ屦���а̤���Ȥ��꤬���롥
�������ϱ��ӥ֥��å�����R'���礭����
��������V1��rS�ˤʤ롥��������������V6��S�Ȥ��礭����
S1S2S3�ϸ����������꼴�Ȥʤ롥
�Ǥ�����Ū���������Ƥ��롥
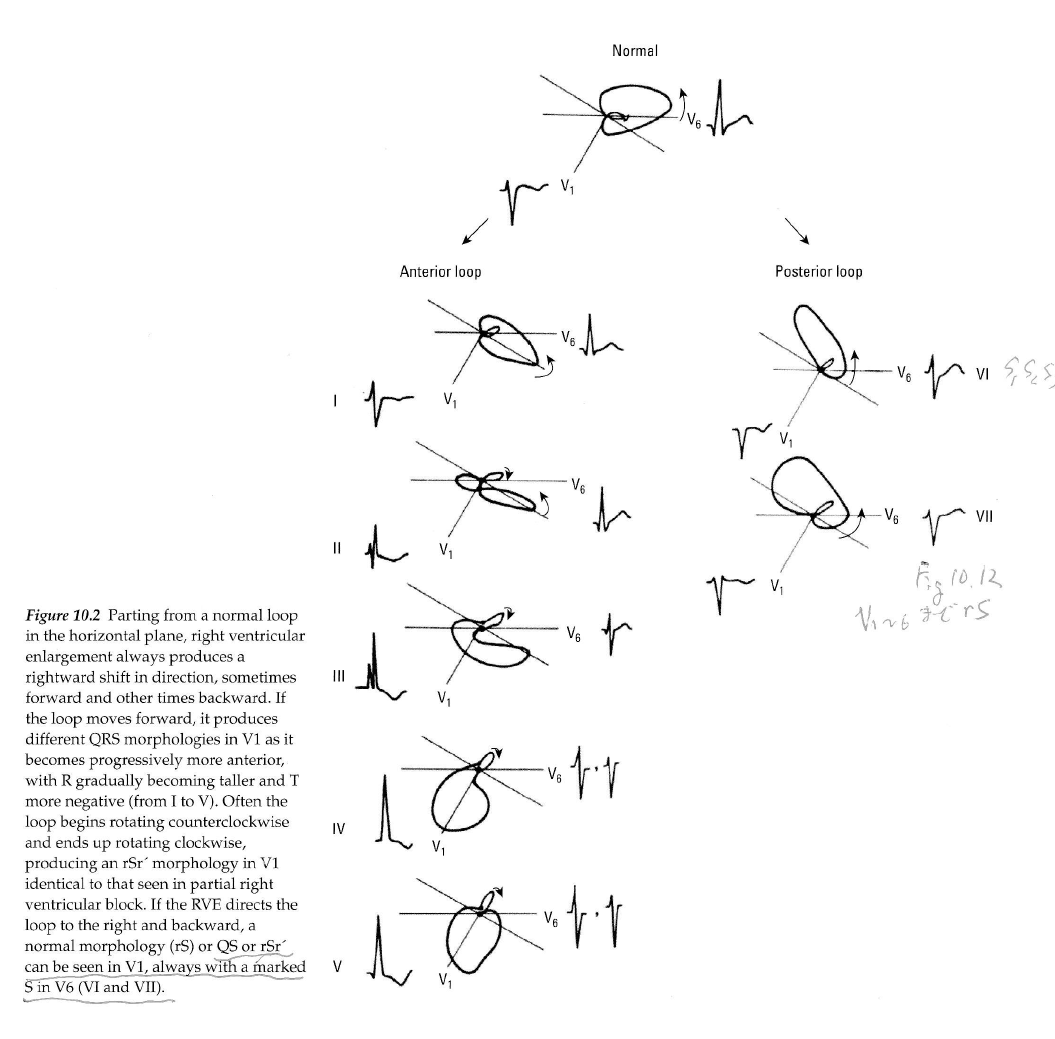 �� �����Ѱ̤�V1���礭��R�Ȥ�RVH��ͤ��롥V1���ܼ�Ū��rSr'�Ǥ��롥
����2���ܤ�r'���礭���ʤ�ȱ��ӥ֥��å�����RVH�ˤʤ롥���ӥ֥��å���
���ϱ�����Ƴ�����ܿ��ڤ���Ƴ�ˤʤ뤿�ᡤ���������ޤ��������礭����
��������������ϥץ륭�����ݤ���Ƴ�Ǥ��뤫����Ƴ���֤�û��S�Ȥ�
���ⶹ���ޤ롥rSr'�κǽ��r����ֿ��ڤζ�ʳ��S�ȤϺ�����ʳ�Ǥ��ꡤ
�Ǹ��r'�ϱ������ڤζ�ʳ�Ǥ��ꡤ�̾��r'��������ɽ���ä�ɽ��ʤ���
�֥륬���ξ��ϱ���ή��ϩ�ο������礬���뤿�ᡤ�礭��r'�ȹͤ����
Ǽ����������
�� �̾��RBB��¸�ߤ����RVH�ο��ǤϤǤ��ʤ�����GE #121��RVH�ο��Ǥ���ǽ�Ǥ��롥
�� BB p.73�Ǥ�3�����RVH��ɽ������Ƥ��롥
���������3 type
Utah ECG Uwave
Right Ventricular Hypertrophy
General ECG features include:
* Right axis deviation (> 90 degrees)
* Tall R-waves in RV leads; deep S-waves in LV leads
* Slight increase in QRS duration
* ST-T changes directed opposite to QRS direction (i.e., wide QRS/T angle)
* May see incomplete RBBB pattern or qR pattern in V1
* Evidence of right atrial enlargement (RAE) (lessonVII)
Specific ECG features (assumes normal calibration of 1 mV = 10 mm):
* Any one or more of the following (if QRS duration < 0.12 sec):
o Right axis deviation (> 90 degrees) in presence of disease capable of causing RVH
o R in aVR �� 5 mm, or
o R in aVR > Q in aVR
* Any one of the following in lead V1:
o R/S ratio > 1 and negative T wave
o qR pattern
o R gt; 6 mm, or S < 2mm, or rSR' with R' > 10 mm
* Other chest lead criteria:
o R in V1 + S in V5 (or V6) 10 mm
o R/S ratio in V5 or V6 < 1
o R in V5 or V6 < 5 mm
o S in V5 or V6 > 7 mm
* ST segment depression and T wave inversion in right precordial leads is usually seen in severe RVH such as in pulmonary stenosis and pulmonary hypertension.
BB�Υ��饤�ƥꥢ p.73
* QRS���ŵ�����90��ʾ�����о��Ǥ��롥
a. qR ��V1
b. V1��R��7mm�ʾ塥
c. V1��R/S�椬1�ʾ塥
d. V1��ID��0.03sec�ʾ塥
e. V1��V6��QRS��rS�ȷ���
f. ��ͤ�S1S2S3�ȷ���
* ����P�ȡ�
* V1��V2��STD��ȿžT�ȡ�
9-14 LAE��IRBBB���ĵ���������ֹ��ɡ�RVH? �����а̡�II, III, aVF��T�ȵ�ž��
RVH��ɬ�ܡ�cf 11-12.
V1�϶���QR�ȷ���V2�Ͼ�����rS���̾��V1�Τ褦�˸����롥V1-V4�ϱ���
���ȥ쥤��T�ȡ������褦���Ǥ����ζ���S�Ȥϱ����������ħ��
11-12 ŵ��Ū��RVH��strain pattern��S1Q3T3�������롥RVH��V1��q�ȤϤʤ���RAE, LAE
11-13 ���귿ŪRVH��V2�� R/S ratio��1�ʾ塥
������ֹ��ɤ�ʻȯ���Ƥ��뤿���V1�ˤʤ�ʤ��������硥���̿��ǡ�
GE #121 II, aVF���ݤ����鼴��-30��ʲ���V1��PVC�Τ褦�˸����뤬�����rsR'
�Ǥ��롥V1-V3�ޤ�rsR'��ȿžT�ȡ�V4-V6��rS�Ȥ�����T�ȡ�
���ǡ�LAFB+CRBBB������RBBB�ϱ�������ο��ǤϽ���ʤ�����
V1�ΰ۾�ʹ⤵��R'��V6��S�ȡ�������ȿžT�Ȥ�RVH�碌�롥
�̾��CRBBB�Ǥ�V6��R�Ȥ�������S�ȤǤ��뤬��RVH�Ǥ�R�Ȥ���������
S�ȤϱԤ�������LAFB����ʻ�����V6��S�ȤϤ���˿����ʤ롥
GE #196 ��90�ʾ塤����P�ȡ�V1��rsR'�Ǥ��뤬��rs�����˾�������R'�ϥ��㡼�פ�
�̾�α��ӥ֥��å��Ȱۤʤ롥V2��V6�ޤǤ϶������ζ���S�ȡ����ӥ֥��å�
�Ǥ����S�������������顤���������鸫�Ƥ�RBBB�Ȥϰۤʤ롥V1��
����T�Ȥǡ�V2��ʿó��V3-V6���̾��T�ȡ�R�Ȥ�V3���Ǥ�⤯��
V6�˹Ԥ��ˤ������ä��ȹ�Ͼ������ʤ롥����P�Ȥȱ������硥
11-14 ventricular escape beat��35 BPM��IVCD,
T�Ȥ�QRS��2�����Ǥ��äƤ��ž���롥��K��� 8.7 mEq/L��
final�Ǥ�Af��ȼ����Ƴ��1ͶƳ����ɽ������Ƥ��ʤ���final p.169
11-15 qR'��RBBB
11-16 VT, ��K��� 9.4mEq/L
11-17 ����P�ȡ�3��AV�֥��å���CLBBB��CRBBB������QRS
2�����P�ȡ�PAC�θ���Ѳ����Ƥ��롥
11-18 VTach (VT)��LAH���а�����V1��V2�δ֡�
11-19 ����q�ȤȰ۾�Q�ȡ��ͻ�ͶƳ
11-20 ����q�ȤȰ۾�Q�ȡ�����ͶƳ
11-21 IIIͶƳS�ȤθƵ۰�ư���ܹ��Ӥ�V1��V2��V1�ο�������������NSSTC��PR���㲼
���ǤϽ줺��
�� �����Ѱ̤�V1���礭��R�Ȥ�RVH��ͤ��롥V1���ܼ�Ū��rSr'�Ǥ��롥
����2���ܤ�r'���礭���ʤ�ȱ��ӥ֥��å�����RVH�ˤʤ롥���ӥ֥��å���
���ϱ�����Ƴ�����ܿ��ڤ���Ƴ�ˤʤ뤿�ᡤ���������ޤ��������礭����
��������������ϥץ륭�����ݤ���Ƴ�Ǥ��뤫����Ƴ���֤�û��S�Ȥ�
���ⶹ���ޤ롥rSr'�κǽ��r����ֿ��ڤζ�ʳ��S�ȤϺ�����ʳ�Ǥ��ꡤ
�Ǹ��r'�ϱ������ڤζ�ʳ�Ǥ��ꡤ�̾��r'��������ɽ���ä�ɽ��ʤ���
�֥륬���ξ��ϱ���ή��ϩ�ο������礬���뤿�ᡤ�礭��r'�ȹͤ����
Ǽ����������
�� �̾��RBB��¸�ߤ����RVH�ο��ǤϤǤ��ʤ�����GE #121��RVH�ο��Ǥ���ǽ�Ǥ��롥
�� BB p.73�Ǥ�3�����RVH��ɽ������Ƥ��롥
���������3 type
Utah ECG Uwave
Right Ventricular Hypertrophy
General ECG features include:
* Right axis deviation (> 90 degrees)
* Tall R-waves in RV leads; deep S-waves in LV leads
* Slight increase in QRS duration
* ST-T changes directed opposite to QRS direction (i.e., wide QRS/T angle)
* May see incomplete RBBB pattern or qR pattern in V1
* Evidence of right atrial enlargement (RAE) (lessonVII)
Specific ECG features (assumes normal calibration of 1 mV = 10 mm):
* Any one or more of the following (if QRS duration < 0.12 sec):
o Right axis deviation (> 90 degrees) in presence of disease capable of causing RVH
o R in aVR �� 5 mm, or
o R in aVR > Q in aVR
* Any one of the following in lead V1:
o R/S ratio > 1 and negative T wave
o qR pattern
o R gt; 6 mm, or S < 2mm, or rSR' with R' > 10 mm
* Other chest lead criteria:
o R in V1 + S in V5 (or V6) 10 mm
o R/S ratio in V5 or V6 < 1
o R in V5 or V6 < 5 mm
o S in V5 or V6 > 7 mm
* ST segment depression and T wave inversion in right precordial leads is usually seen in severe RVH such as in pulmonary stenosis and pulmonary hypertension.
BB�Υ��饤�ƥꥢ p.73
* QRS���ŵ�����90��ʾ�����о��Ǥ��롥
a. qR ��V1
b. V1��R��7mm�ʾ塥
c. V1��R/S�椬1�ʾ塥
d. V1��ID��0.03sec�ʾ塥
e. V1��V6��QRS��rS�ȷ���
f. ��ͤ�S1S2S3�ȷ���
* ����P�ȡ�
* V1��V2��STD��ȿžT�ȡ�
9-14 LAE��IRBBB���ĵ���������ֹ��ɡ�RVH? �����а̡�II, III, aVF��T�ȵ�ž��
RVH��ɬ�ܡ�cf 11-12.
V1�϶���QR�ȷ���V2�Ͼ�����rS���̾��V1�Τ褦�˸����롥V1-V4�ϱ���
���ȥ쥤��T�ȡ������褦���Ǥ����ζ���S�Ȥϱ����������ħ��
11-12 ŵ��Ū��RVH��strain pattern��S1Q3T3�������롥RVH��V1��q�ȤϤʤ���RAE, LAE
11-13 ���귿ŪRVH��V2�� R/S ratio��1�ʾ塥
������ֹ��ɤ�ʻȯ���Ƥ��뤿���V1�ˤʤ�ʤ��������硥���̿��ǡ�
GE #121 II, aVF���ݤ����鼴��-30��ʲ���V1��PVC�Τ褦�˸����뤬�����rsR'
�Ǥ��롥V1-V3�ޤ�rsR'��ȿžT�ȡ�V4-V6��rS�Ȥ�����T�ȡ�
���ǡ�LAFB+CRBBB������RBBB�ϱ�������ο��ǤϽ���ʤ�����
V1�ΰ۾�ʹ⤵��R'��V6��S�ȡ�������ȿžT�Ȥ�RVH�碌�롥
�̾��CRBBB�Ǥ�V6��R�Ȥ�������S�ȤǤ��뤬��RVH�Ǥ�R�Ȥ���������
S�ȤϱԤ�������LAFB����ʻ�����V6��S�ȤϤ���˿����ʤ롥
GE #196 ��90�ʾ塤����P�ȡ�V1��rsR'�Ǥ��뤬��rs�����˾�������R'�ϥ��㡼�פ�
�̾�α��ӥ֥��å��Ȱۤʤ롥V2��V6�ޤǤ϶������ζ���S�ȡ����ӥ֥��å�
�Ǥ����S�������������顤���������鸫�Ƥ�RBBB�Ȥϰۤʤ롥V1��
����T�Ȥǡ�V2��ʿó��V3-V6���̾��T�ȡ�R�Ȥ�V3���Ǥ�⤯��
V6�˹Ԥ��ˤ������ä��ȹ�Ͼ������ʤ롥����P�Ȥȱ������硥
11-14 ventricular escape beat��35 BPM��IVCD,
T�Ȥ�QRS��2�����Ǥ��äƤ��ž���롥��K��� 8.7 mEq/L��
final�Ǥ�Af��ȼ����Ƴ��1ͶƳ����ɽ������Ƥ��ʤ���final p.169
11-15 qR'��RBBB
11-16 VT, ��K��� 9.4mEq/L
11-17 ����P�ȡ�3��AV�֥��å���CLBBB��CRBBB������QRS
2�����P�ȡ�PAC�θ���Ѳ����Ƥ��롥
11-18 VTach (VT)��LAH���а�����V1��V2�δ֡�
11-19 ����q�ȤȰ۾�Q�ȡ��ͻ�ͶƳ
11-20 ����q�ȤȰ۾�Q�ȡ�����ͶƳ
11-21 IIIͶƳS�ȤθƵ۰�ư���ܹ��Ӥ�V1��V2��V1�ο�������������NSSTC��PR���㲼
���ǤϽ줺��
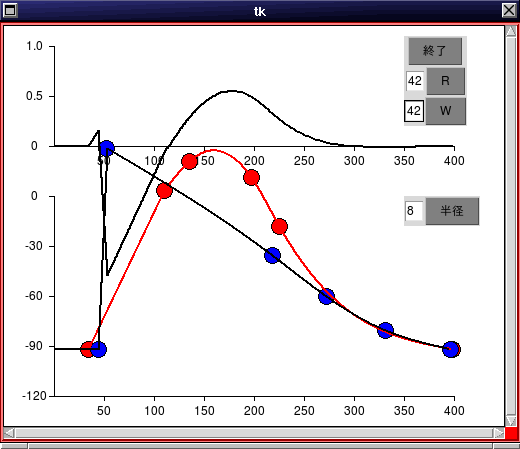
 GE #248��QRS����0.10��IVCD�����ײ�ž�Ǥ��뤬��S�Ȥ�Ω���ǥΥå������롥
GE #305�ϰ츫IVCD�˸����뤬WPW�Ǥ��롥
intraventricular conduction defect p.94 ecg 9-5
�̾��QRS�δ֤˥���������ȯ���������ࡼ���ʶ�ʳ��Ƴ���Ǥ��ʤ����֡�
ecg 9-5��IVCDdelay�Ǥ⤢�롥V1�Ϻ��ӥ֥��å�����V6�Ͽ������������Ƥ�RS���Ǥ��롥
�ޤ�V1�ޤ���V2��S�Ȥ��Ǥ��礭��R�Ȥ��������ɤΤޤ�V6������Τⶦ�̤��Ƥ��롥
intraventricular conduction delay (IVCD) 12 LEAD ECG p.289
QRS����0.12sec�ʾ塤V1��LBBB�ͤ�V6��RBBB�ͤ��ȷ����������롥
��K��ɤ�����Ū�ȷ���
141f ecg 10-7, WPW Type A����Ǥ��뤬��III��aVF��P�Ȥ���������
ʣ����QRS�ȷ��Ǥ��롥�����IVCD�ȿ��Ǥ��롥(�ü����)
p.336 ecg 14-8�ϥƥ�Ⱦ�T�ȡ�IVCD��V5, V6��RS�ȷ��ˤʤ�ʤ�����IVCD�ȿ��ǡ�
198f ecg 11-14, ��K��ɤˤ��IVCD��QRS��������������̮��������ͭĴΧ��
V1�Ϻ��ӥ֥��å��η��Ǥ��뤬��V4�ޤ��Ѳ������ʤ���V6��RS�ȷ��ΤޤޤǤ��롥
QRS����6mm (ŵ��Ū����)
12 lead ECG pp. 289-293
13-21 PR 0.2sec, 77 bpm, IVCD
13-22 P�Ȥʤ���48 bpm, QRS 0.24sec IVCD��QT�ֳ֤ϱ�Ĺ�����Ż߾��֤����롥
p.336 14-18�ϥƥ�Ⱦ�T�ȡ�IVCD��V5, V6��RS�ȷ��ˤʤ餺���ȷ������Ƥ��롥
13-23 �����ڡ����ˤ�뿴���ȷ���IVCD�ͥѥ�����
14-57 IVCD, QRS 0.18, ����Ū��I��V6�ϻ����ȷ��Ǥ��뤬��V6��RS�ѥ�����QRS��0.12sec�ʲ�����LAFB�ˤʤ롥T�ȤˤĤ��ƤϺǸ��S�Ȥ���˹ͤ����Ʊ��(concordant)�ˤʤ뤬�֥��å�������۾�Ǥ��롥
GE #248��QRS����0.10��IVCD�����ײ�ž�Ǥ��뤬��S�Ȥ�Ω���ǥΥå������롥
GE #305�ϰ츫IVCD�˸����뤬WPW�Ǥ��롥
intraventricular conduction defect p.94 ecg 9-5
�̾��QRS�δ֤˥���������ȯ���������ࡼ���ʶ�ʳ��Ƴ���Ǥ��ʤ����֡�
ecg 9-5��IVCDdelay�Ǥ⤢�롥V1�Ϻ��ӥ֥��å�����V6�Ͽ������������Ƥ�RS���Ǥ��롥
�ޤ�V1�ޤ���V2��S�Ȥ��Ǥ��礭��R�Ȥ��������ɤΤޤ�V6������Τⶦ�̤��Ƥ��롥
intraventricular conduction delay (IVCD) 12 LEAD ECG p.289
QRS����0.12sec�ʾ塤V1��LBBB�ͤ�V6��RBBB�ͤ��ȷ����������롥
��K��ɤ�����Ū�ȷ���
141f ecg 10-7, WPW Type A����Ǥ��뤬��III��aVF��P�Ȥ���������
ʣ����QRS�ȷ��Ǥ��롥�����IVCD�ȿ��Ǥ��롥(�ü����)
p.336 ecg 14-8�ϥƥ�Ⱦ�T�ȡ�IVCD��V5, V6��RS�ȷ��ˤʤ�ʤ�����IVCD�ȿ��ǡ�
198f ecg 11-14, ��K��ɤˤ��IVCD��QRS��������������̮��������ͭĴΧ��
V1�Ϻ��ӥ֥��å��η��Ǥ��뤬��V4�ޤ��Ѳ������ʤ���V6��RS�ȷ��ΤޤޤǤ��롥
QRS����6mm (ŵ��Ū����)
12 lead ECG pp. 289-293
13-21 PR 0.2sec, 77 bpm, IVCD
13-22 P�Ȥʤ���48 bpm, QRS 0.24sec IVCD��QT�ֳ֤ϱ�Ĺ�����Ż߾��֤����롥
p.336 14-18�ϥƥ�Ⱦ�T�ȡ�IVCD��V5, V6��RS�ȷ��ˤʤ餺���ȷ������Ƥ��롥
13-23 �����ڡ����ˤ�뿴���ȷ���IVCD�ͥѥ�����
14-57 IVCD, QRS 0.18, ����Ū��I��V6�ϻ����ȷ��Ǥ��뤬��V6��RS�ѥ�����QRS��0.12sec�ʲ�����LAFB�ˤʤ롥T�ȤˤĤ��ƤϺǸ��S�Ȥ���˹ͤ����Ʊ��(concordant)�ˤʤ뤬�֥��å�������۾�Ǥ��롥
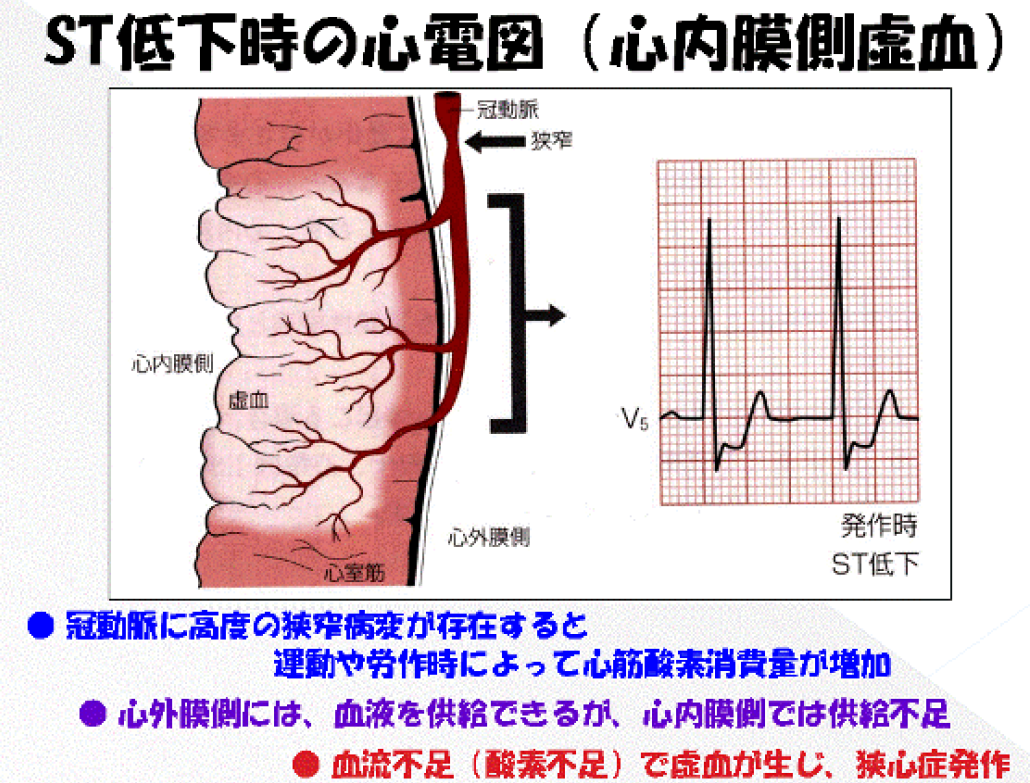
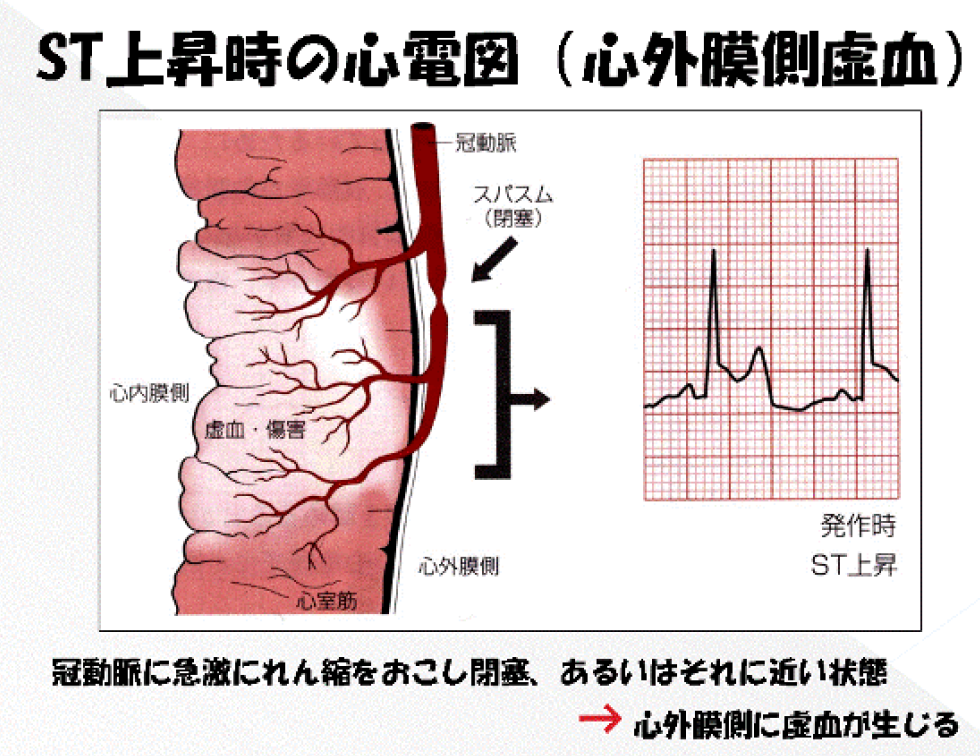
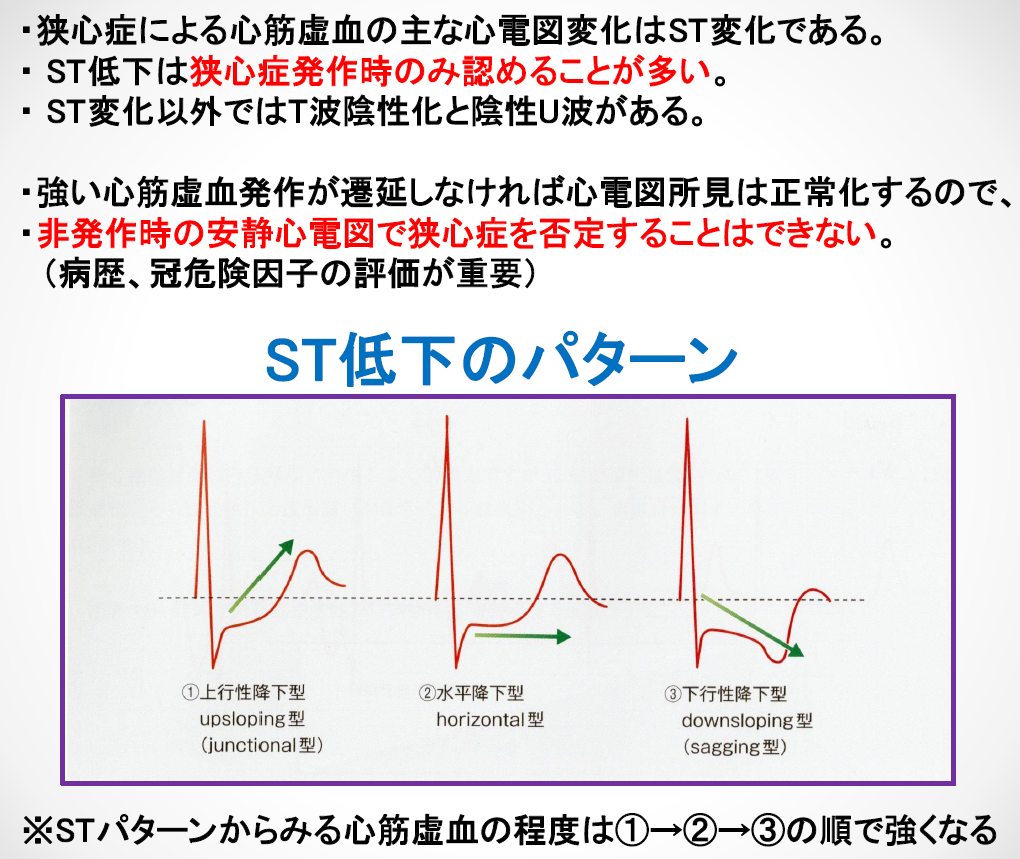
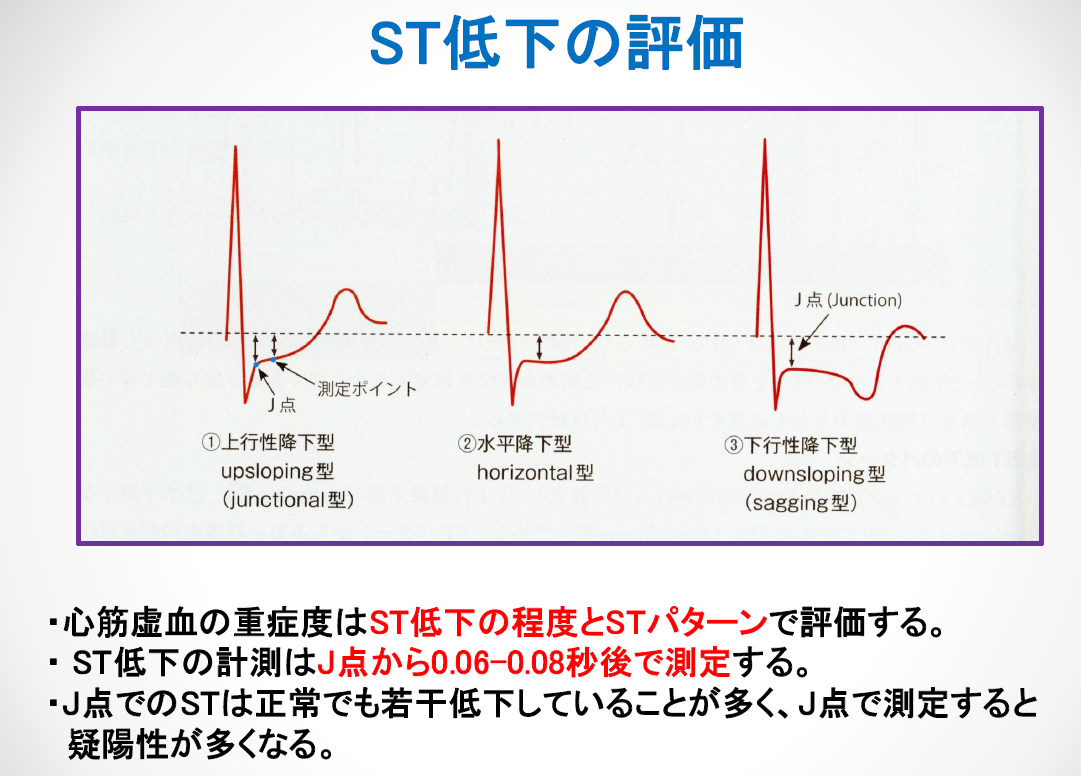
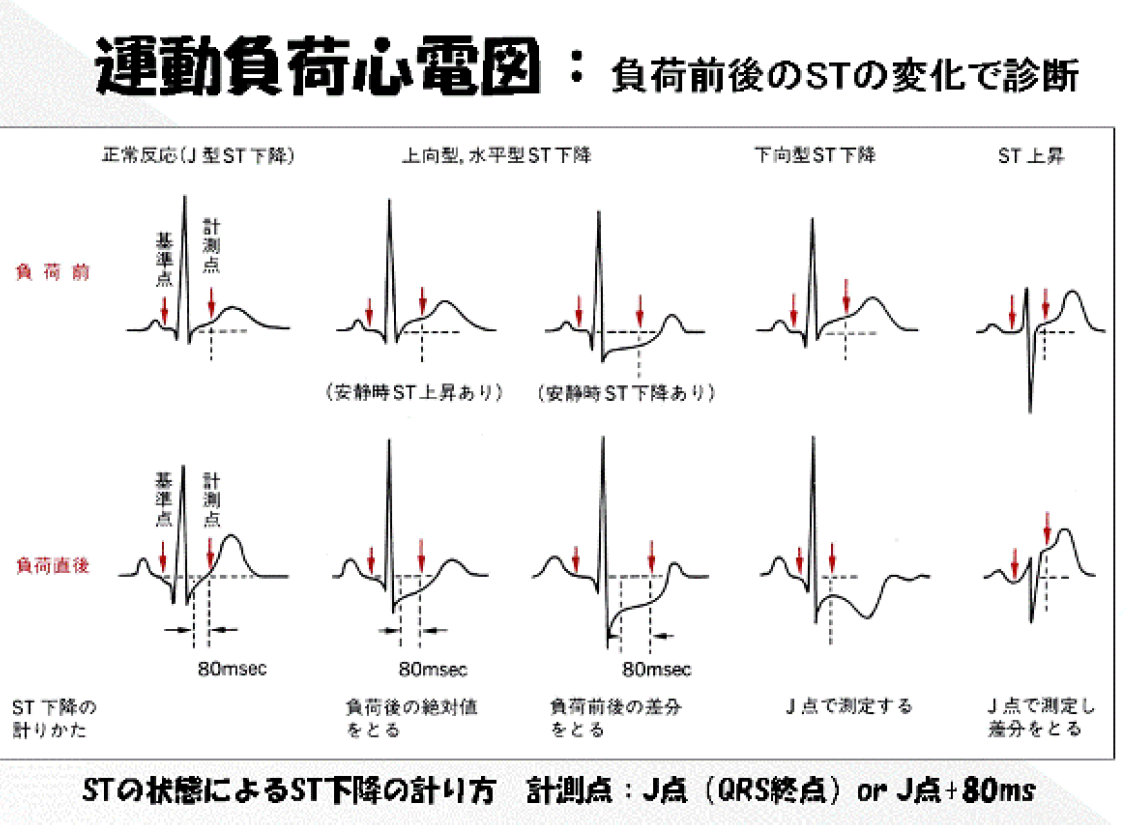
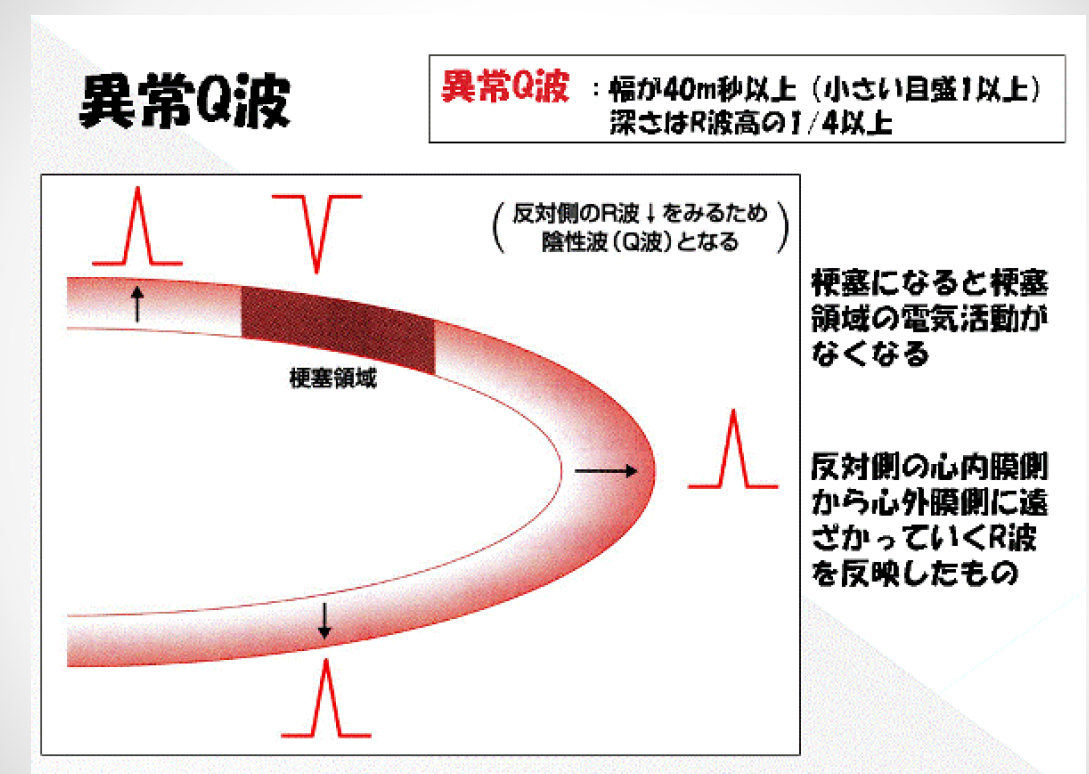
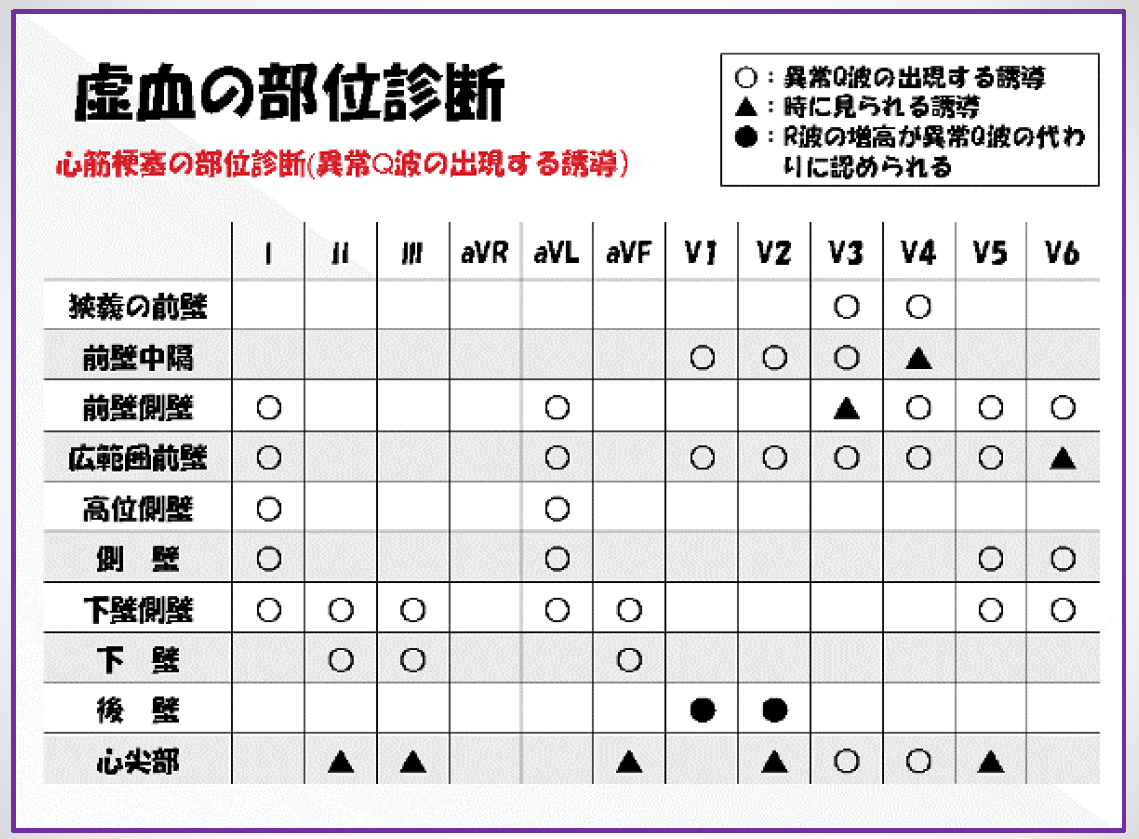
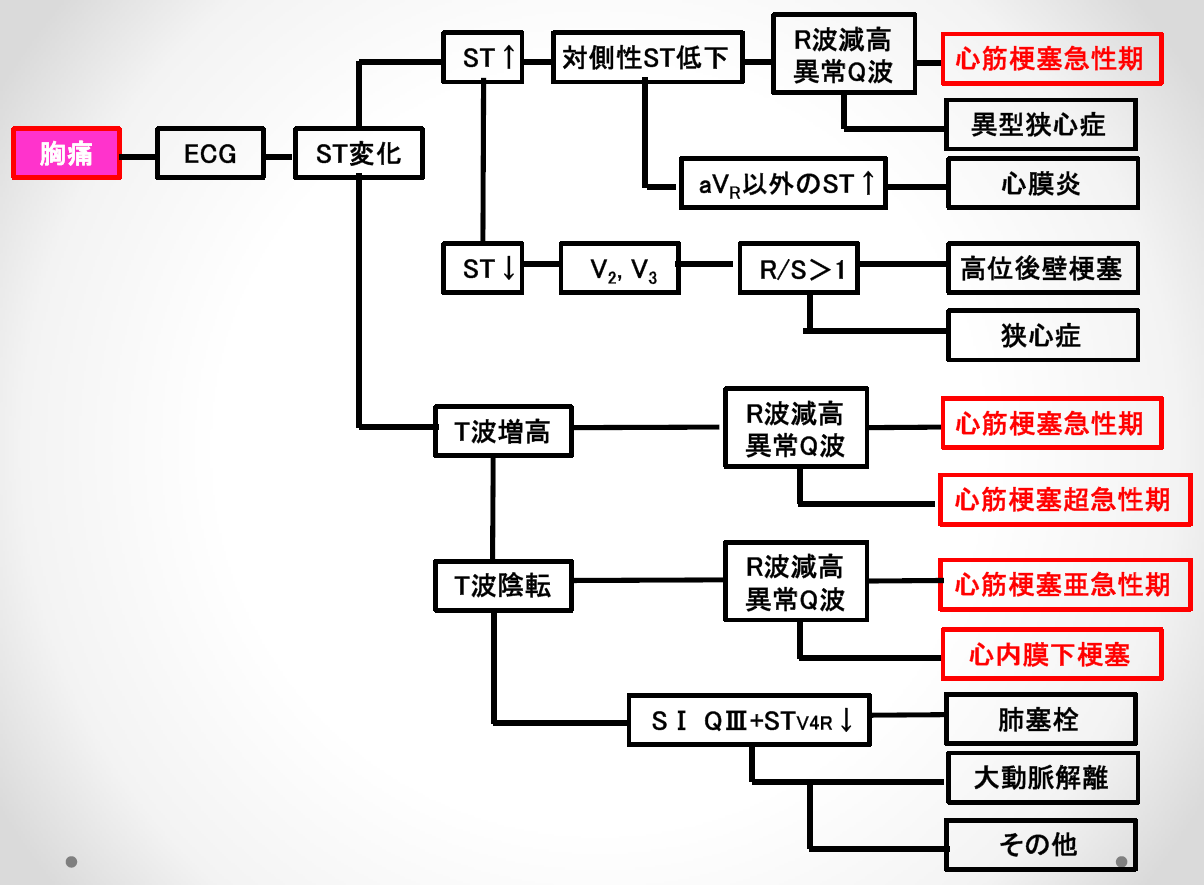
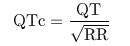 QT (msec), RR (sec)
QT (msec), RR (sec)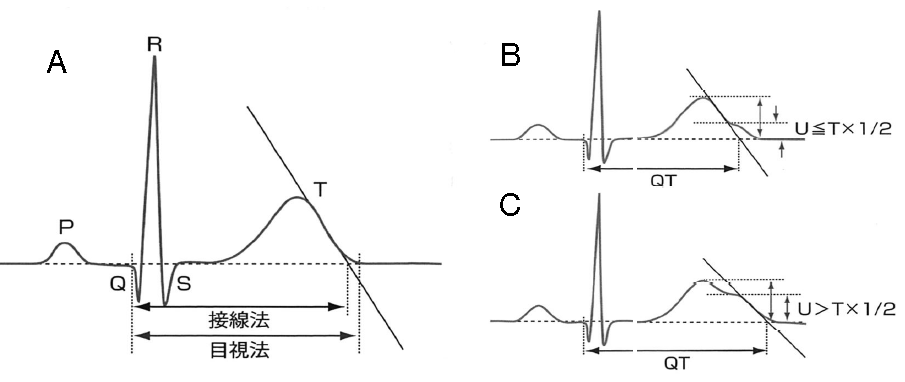
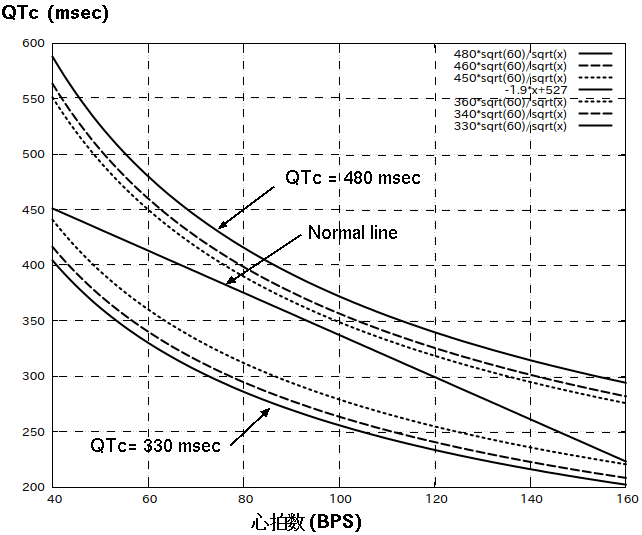
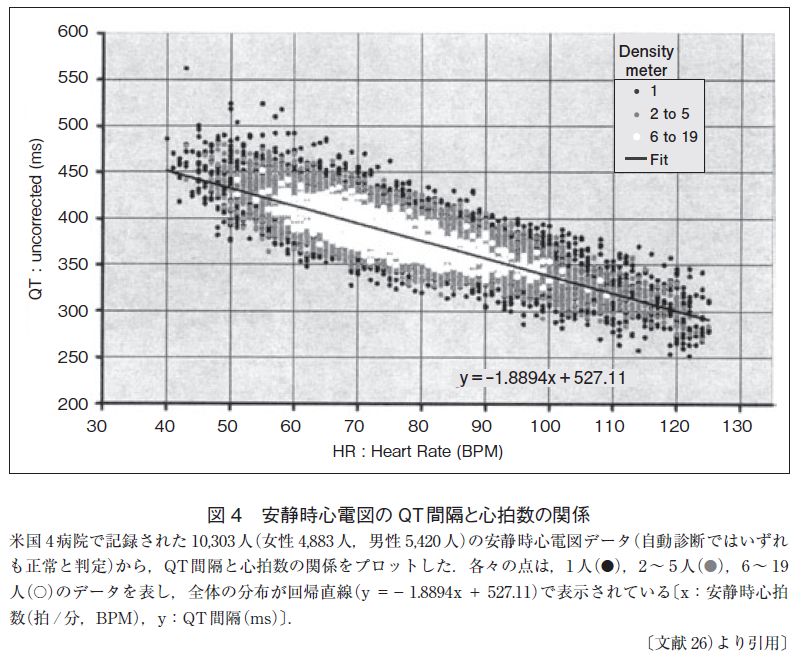 QTc���
Bazett: QTcB=QT/(RR)1/2
Friderica:QTcF=QT/(RR)1/3
Hodges: QTcH=QT+105(1/RR-1)
Bazett��Friderica��Hodges���������Ǥ�RR��ñ�̤�sec����Ѥ��롥
Framingham: QTcFr=QT+0.154(1000-RR)
RR��ñ�̤�msec����Ѥ��롥
QTc���
Bazett: QTcB=QT/(RR)1/2
Friderica:QTcF=QT/(RR)1/3
Hodges: QTcH=QT+105(1/RR-1)
Bazett��Friderica��Hodges���������Ǥ�RR��ñ�̤�sec����Ѥ��롥
Framingham: QTcFr=QT+0.154(1000-RR)
RR��ñ�̤�msec����Ѥ��롥
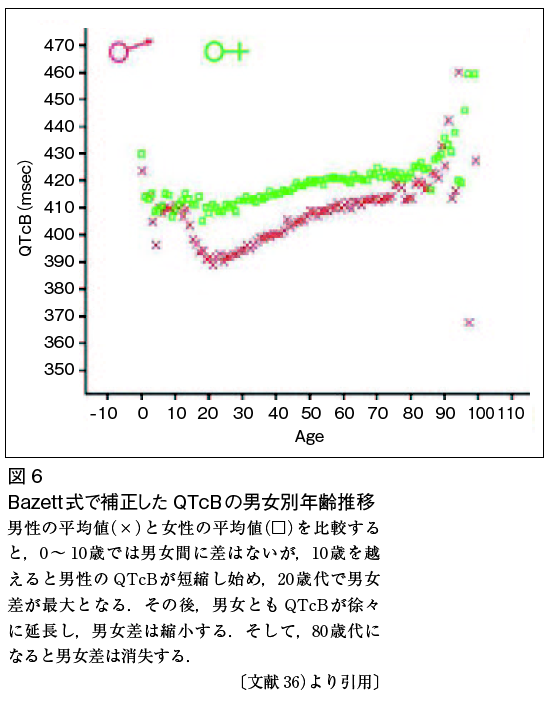
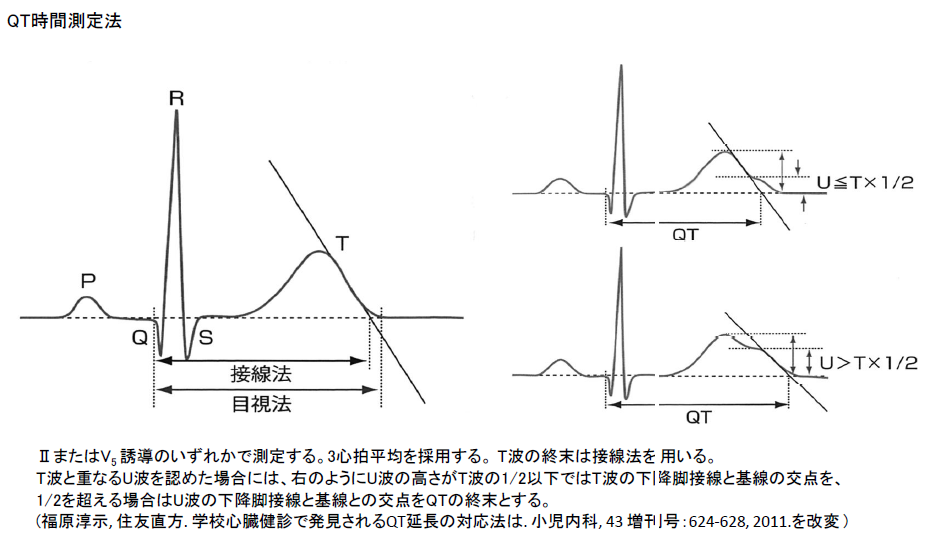
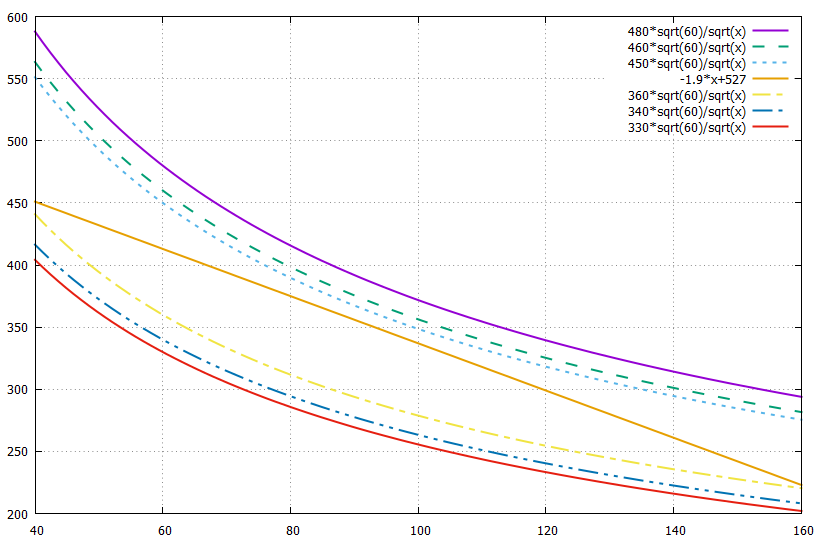
 lqt.gif
QT���֤�R-R�ֳ֤�1/2�ʾ�Ǥ����long QT, ���ʤ��QT��Ĺ�ɸ����Ȥ�����
�㥫�ꥦ���ɤ�U�Ȥ�T�Ȥβ�����ʬ��ͻ�礷�Ƥ��뤿���U�Ȥ�QT���֤�
�ޤ������褤��
��������̮��ȯ������U�Ȥ�QT���֤˴ޤ�ʤ��Τ������Ǥ��롥
lqt.gif
QT���֤�R-R�ֳ֤�1/2�ʾ�Ǥ����long QT, ���ʤ��QT��Ĺ�ɸ����Ȥ�����
�㥫�ꥦ���ɤ�U�Ȥ�T�Ȥβ�����ʬ��ͻ�礷�Ƥ��뤿���U�Ȥ�QT���֤�
�ޤ������褤��
��������̮��ȯ������U�Ȥ�QT���֤˴ޤ�ʤ��Τ������Ǥ��롥
 1.5 mEq/L����K���
U�Ȥξ��P�Ȥ���äƤ��롥
1.5 mEq/L����K���
U�Ȥξ��P�Ȥ���äƤ��롥
 Romano-Word syndrome
QT��Ĺ�ɸ����Dz��٤⼺��ȯ������Ƥ롥����T�Ȥ�����U�Ȥ������롥
Romano-Word syndrome
QT��Ĺ�ɸ����Dz��٤⼺��ȯ������Ƥ롥����T�Ȥ�����U�Ȥ������롥
 ��Ca���
ST�������Ȥϥե�åȤDZ�Ĺ���롤T�Ȥ��ȷ������
QT��Ĺ�ɸ����Dz��٤⼺��ȯ������Ƥ롥����T�Ȥ�����U�Ȥ������롥
��Ca���
ST�������Ȥϥե�åȤDZ�Ĺ���롤T�Ȥ��ȷ������
QT��Ĺ�ɸ����Dz��٤⼺��ȯ������Ƥ롥����T�Ȥ�����U�Ȥ������롥
 R on T����Torsades de Pointes
T�Ȥξ�ǿ����������̤˻�������Ƴ��ȯ����2��̮�Ǥ��롤���θ塤�ȥ륵�ǥݥ���ȯ����
�Ƕ��QT��Ĺ�ɸ���������������
QT��Ĺ�ɸ����ο��ſ��Ѳ�
R on T����Torsades de Pointes
T�Ȥξ�ǿ����������̤˻�������Ƴ��ȯ����2��̮�Ǥ��롤���θ塤�ȥ륵�ǥݥ���ȯ����
�Ƕ��QT��Ĺ�ɸ���������������
QT��Ĺ�ɸ����ο��ſ��Ѳ�
 prd.png #191
IMG_20170912_0005.pdf
final p.142��ꡧ
�ܹ���ĴΧ��II��P�Ȳ�������QRS�����Ǥ�0.12�ð��⡤��Ǥ�0.19�ð��⡥
����P��
P�Ȥ��ŵ�����0��75�롤Junctional P��-60��-80�롥p.91
P-mitrale(LAE): p.93
I�ޤ���II������0.12s�ʾ塤hump��ĺ���֤�0.04s�ʾ塥
ĺ���֤�0.04s�ʲ��ʤ�LAE�ȤϿ��ǤǤ��ʤ���
P-pulmonale(RAE): p.99
�⤵��2.5mm�ʾ塥����ʲ��ʤ�RAE�ǤϤʤ���
V1ͶƳ��P�Ⱦ��������ե�åȤˤʤ뤳�Ȥ����롥
�ŵ����������аܤǡ�RAE�ʤ顤LPH��¸�ߤ��ʤ���
��˼����Ƴ�ٱ�(IACD)��p.105
V1��2������P�ȤǤ��뤬���ͻ�ͶƳ������P�Ȥ���˼��P�Ȥˤʤ�ʤ����֡�
ex1 V1����Ⱦ�ι⤵��V6�ι⤵����礭����� -> RAE�β�ǽ�����⤤��
ex2 V1�θ�Ⱦ�δٱ���1mm�������������� -> LAE�β�ǽ�����⤤��
ξ��˼����(BAE)��p.117
ex1 IIͶƳ������P�ȡ�V1��2���ܤδٱ�
ex2 IIͶƳ����˼P�ȡ�V1��1���ܤγ���
final p.79
prd.png #191
IMG_20170912_0005.pdf
final p.142��ꡧ
�ܹ���ĴΧ��II��P�Ȳ�������QRS�����Ǥ�0.12�ð��⡤��Ǥ�0.19�ð��⡥
����P��
P�Ȥ��ŵ�����0��75�롤Junctional P��-60��-80�롥p.91
P-mitrale(LAE): p.93
I�ޤ���II������0.12s�ʾ塤hump��ĺ���֤�0.04s�ʾ塥
ĺ���֤�0.04s�ʲ��ʤ�LAE�ȤϿ��ǤǤ��ʤ���
P-pulmonale(RAE): p.99
�⤵��2.5mm�ʾ塥����ʲ��ʤ�RAE�ǤϤʤ���
V1ͶƳ��P�Ⱦ��������ե�åȤˤʤ뤳�Ȥ����롥
�ŵ����������аܤǡ�RAE�ʤ顤LPH��¸�ߤ��ʤ���
��˼����Ƴ�ٱ�(IACD)��p.105
V1��2������P�ȤǤ��뤬���ͻ�ͶƳ������P�Ȥ���˼��P�Ȥˤʤ�ʤ����֡�
ex1 V1����Ⱦ�ι⤵��V6�ι⤵����礭����� -> RAE�β�ǽ�����⤤��
ex2 V1�θ�Ⱦ�δٱ���1mm�������������� -> LAE�β�ǽ�����⤤��
ξ��˼����(BAE)��p.117
ex1 IIͶƳ������P�ȡ�V1��2���ܤδٱ�
ex2 IIͶƳ����˼P�ȡ�V1��1���ܤγ���
final p.79
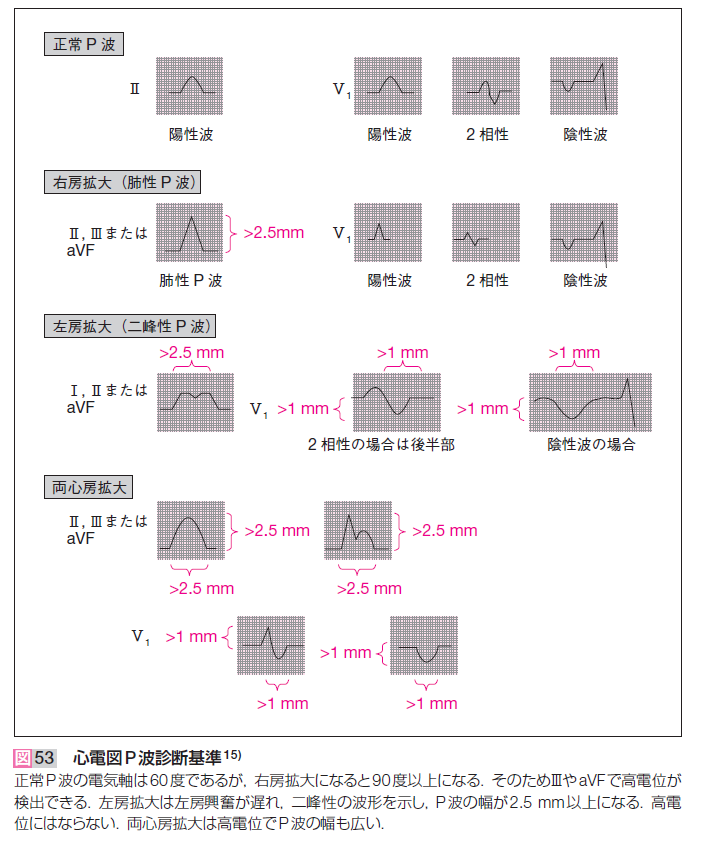
 ��ޤϿ������73�Ǥ��뤫�顤¥�����ܹ���ĴΧ�Ȥ�֡�
��ޤϿ������73�Ǥ��뤫�顤¥�����ܹ���ĴΧ�Ȥ�֡�
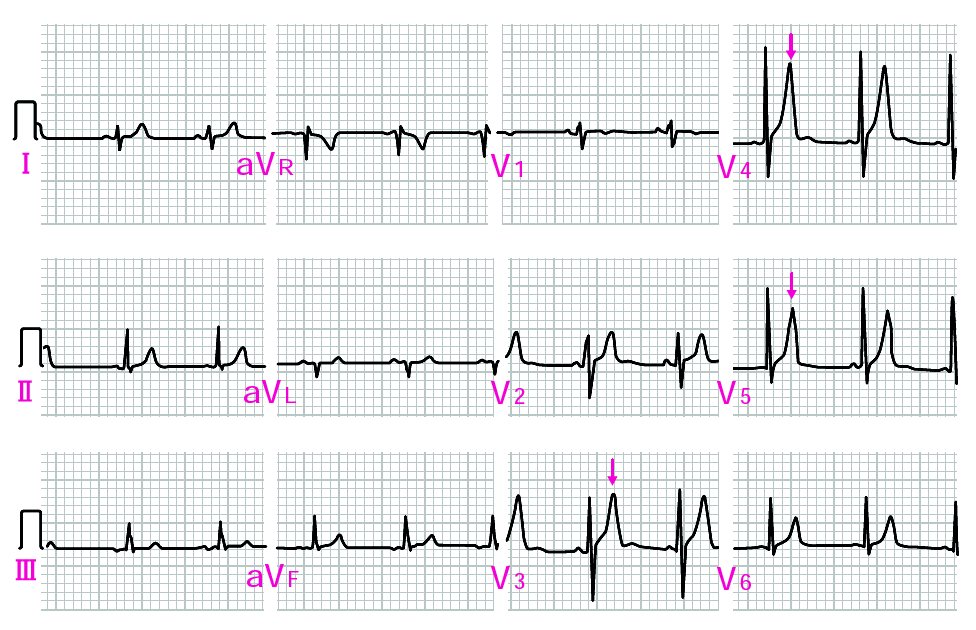 ����K+������ǻ�٤�8.2mEQ/L���������������Ԥο��ſޡ�
����K+������ǻ�٤�8.2mEQ/L���������������Ԥο��ſޡ�
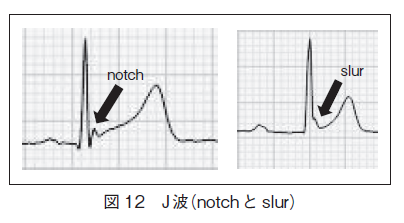 ̮����ʤ��STE�������ꡤ�������롥
�����ˤ����ꡤ��������AMI�����ȷ��롥
�������Ǥ�PR�������Ȥ��㲼�����뤬��BER�ˤϤʤ���12 Lead p.129, ECG 10-1.
50�Ͱʾ�ˤʤ��STE�ϸ�������AMI���θ���롥70�Ͱʾ��BER�ϵ��Ǥ��롥
̮����ʤ��STE�������ꡤ�������롥
�����ˤ����ꡤ��������AMI�����ȷ��롥
�������Ǥ�PR�������Ȥ��㲼�����뤬��BER�ˤϤʤ���12 Lead p.129, ECG 10-1.
50�Ͱʾ�ˤʤ��STE�ϸ�������AMI���θ���롥70�Ͱʾ��BER�ϵ��Ǥ��롥
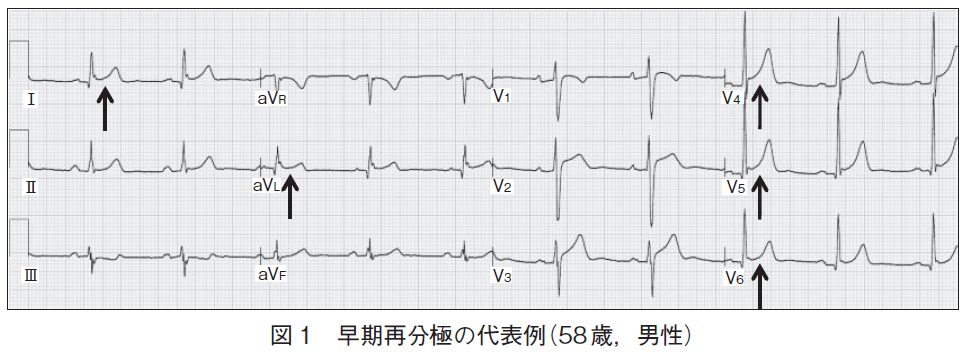 ��ŵ��34_368.pdf
BER(Benign Early Repolarisation)
��ŵ��34_368.pdf
BER(Benign Early Repolarisation)
 IMG_20180724_0006a.png
p.431. ����ư̮���ĺɤǤ���С������ޤȲ����ޤ��ĺɤˤʤ롥
15-4 V1�����V2��V6�ޤ�STE�ι��ɡ�������q�Ȥ����뤬�������ϰϤ���
I,aVL��STE���ߥ顼��III,aVF��STD��������III���Ǥ�Ĥ褤�������ˤ�
q�Ȥ����뤬�������ϰϤ���
����Ǥ�q�Ȥϰ۾�Q�ȤǤ��롥Ķ������STE��
15-5 V1��V4��STE�ǥɡ������V5��V6���о���T�ȵ�ž��I,aVL��STE��
III,aVF�Υߥ顼STD��VͶƳ��R�Ȥ��ݤ���Ƥ��롥
����Ǥ�V5��STE�ǹ��ɥѥ�����
15-6 V1��V6�ޤǤΰ۾�Q�Ȥ�STE��I,aVL��STE��ȿžT�ȡ�II,III,aVF��STD�Ⱦ����
T�ȡ�
����Ǥ�V1��r�Ȥ�¸�ߤ��뤫��QS�ȤǤϤʤ���rS�ȤǤ��롥
15-7 V1��V5�ޤǤ�STE��I,aVL��STE��II,III,aVF�Υߥ顼��
15-8 Junctional P, I,aVL,V1��V6�ޤǤξ����ST������STE��
IMG_20180724_0006a.png
p.431. ����ư̮���ĺɤǤ���С������ޤȲ����ޤ��ĺɤˤʤ롥
15-4 V1�����V2��V6�ޤ�STE�ι��ɡ�������q�Ȥ����뤬�������ϰϤ���
I,aVL��STE���ߥ顼��III,aVF��STD��������III���Ǥ�Ĥ褤�������ˤ�
q�Ȥ����뤬�������ϰϤ���
����Ǥ�q�Ȥϰ۾�Q�ȤǤ��롥Ķ������STE��
15-5 V1��V4��STE�ǥɡ������V5��V6���о���T�ȵ�ž��I,aVL��STE��
III,aVF�Υߥ顼STD��VͶƳ��R�Ȥ��ݤ���Ƥ��롥
����Ǥ�V5��STE�ǹ��ɥѥ�����
15-6 V1��V6�ޤǤΰ۾�Q�Ȥ�STE��I,aVL��STE��ȿžT�ȡ�II,III,aVF��STD�Ⱦ����
T�ȡ�
����Ǥ�V1��r�Ȥ�¸�ߤ��뤫��QS�ȤǤϤʤ���rS�ȤǤ��롥
15-7 V1��V5�ޤǤ�STE��I,aVL��STE��II,III,aVF�Υߥ顼��
15-8 Junctional P, I,aVL,V1��V6�ޤǤξ����ST������STE��
 #28
�� final p.28�ο�18�β���ϴְ�äƤ��롥
V4,V5,V6��¦�ɹ��ɤΰ۾�Q�ȤǤ��롥���ι��ɤ����ɤ˵ڤӡ�V1��V2�ι⤤
R�Ȥˤʤ롥V5,V6��S�Ȥ��ʤ����Ȥϱ��ӥ֥��å��䱦����������ꤹ��ڵ�Ǥ��롥
2018ǯ 7�� 12�� ������ 16:51:08 JST
final�β���ϴְ㤤�ǤϤʤ���������δ���T�ȤϤɤΤ褦����������Τ�
ʬ����ʤ���GE #28��V!-V3��Ω�ɤʴ���T�ȤǤ��롥
15-15 III��aVF�˶����۾�Q�Ȥ����뤬��STE�ʤɤ��Ѳ����ʤ���Q�Ȥ���°����R��
1/3�ʾ塤�ޤ���0.03sec�ʾ�Ǥ����ͭ�٤Ȥ��롥�ĵ������ɹ��ɡ�
15-16 V1��V6���Ŷ˴ְ㤤��CRBBB�˿�ȼ����IWMI��
II,III,aVF�ΰ۾�Q�ȡ�����̤�STE��
���ȥե����� iwmi
9-13 IACD��LAE���㡤II, III, aVF��Q�ȡ��о���T��ȿž��
II,III,aVF�Ϥ��о���ȿžT�ȡ�V1-6���������оΥ��ȥ쥤��T�ȡ�
�ͻ�Ͽ�ʿST��LVH����˼��١����ɹ���
����¦�ɤ˲ä��Ƹ��ɹ��ɤ���
11-22 II, III, aVF��Q�Ȥ�������V4��V6��Q�ȡ�V1��R�Ȥ��⤯����������
���ɡ�¦�ɤι��ɤ�Ϣ³��������ɤι��ɤ��ͤ����롥transition��V1��V2��
I��q�ȤϾ����礭���۾aVL��q�Ȥ�۾�ǹ��¦�ɹ��ɡ�
V1��R�Ȥ��⤯���������Τϡ����ɹ��ɤ����ä����Ȥ���
V1,V2��J�����㲼���Ƥ��ʤ����Ȥϡ����ɤ�ST�徺���ʤ����Ȥ���
���ɹ��ɤΰ۾�Q�Ȥ�III>aVF>II�ν�˾������ʤ뤬�����¦�ɹ��ɤ�
ȯ�������I�ǰ۾�Q�Ȥ������뤿��III�Ǥΰ������ⲽ���ä���롥
aVL��Q�Ȥθ����aVL=(i-III)/2������I��Q�Ȥ���III��Q�Ȥ���������
����˾�����Q�Ȥˤʤ롥
#28
�� final p.28�ο�18�β���ϴְ�äƤ��롥
V4,V5,V6��¦�ɹ��ɤΰ۾�Q�ȤǤ��롥���ι��ɤ����ɤ˵ڤӡ�V1��V2�ι⤤
R�Ȥˤʤ롥V5,V6��S�Ȥ��ʤ����Ȥϱ��ӥ֥��å��䱦����������ꤹ��ڵ�Ǥ��롥
2018ǯ 7�� 12�� ������ 16:51:08 JST
final�β���ϴְ㤤�ǤϤʤ���������δ���T�ȤϤɤΤ褦����������Τ�
ʬ����ʤ���GE #28��V!-V3��Ω�ɤʴ���T�ȤǤ��롥
15-15 III��aVF�˶����۾�Q�Ȥ����뤬��STE�ʤɤ��Ѳ����ʤ���Q�Ȥ���°����R��
1/3�ʾ塤�ޤ���0.03sec�ʾ�Ǥ����ͭ�٤Ȥ��롥�ĵ������ɹ��ɡ�
15-16 V1��V6���Ŷ˴ְ㤤��CRBBB�˿�ȼ����IWMI��
II,III,aVF�ΰ۾�Q�ȡ�����̤�STE��
���ȥե����� iwmi
9-13 IACD��LAE���㡤II, III, aVF��Q�ȡ��о���T��ȿž��
II,III,aVF�Ϥ��о���ȿžT�ȡ�V1-6���������оΥ��ȥ쥤��T�ȡ�
�ͻ�Ͽ�ʿST��LVH����˼��١����ɹ���
����¦�ɤ˲ä��Ƹ��ɹ��ɤ���
11-22 II, III, aVF��Q�Ȥ�������V4��V6��Q�ȡ�V1��R�Ȥ��⤯����������
���ɡ�¦�ɤι��ɤ�Ϣ³��������ɤι��ɤ��ͤ����롥transition��V1��V2��
I��q�ȤϾ����礭���۾aVL��q�Ȥ�۾�ǹ��¦�ɹ��ɡ�
V1��R�Ȥ��⤯���������Τϡ����ɹ��ɤ����ä����Ȥ���
V1,V2��J�����㲼���Ƥ��ʤ����Ȥϡ����ɤ�ST�徺���ʤ����Ȥ���
���ɹ��ɤΰ۾�Q�Ȥ�III>aVF>II�ν�˾������ʤ뤬�����¦�ɹ��ɤ�
ȯ�������I�ǰ۾�Q�Ȥ������뤿��III�Ǥΰ������ⲽ���ä���롥
aVL��Q�Ȥθ����aVL=(i-III)/2������I��Q�Ȥ���III��Q�Ȥ���������
����˾�����Q�Ȥˤʤ롥
 ECG 15-28
15-29 II,III,aVF��Q�Ȥ�V1V2��R�Ⱦ徺���Ť����ɸ��ɹ��ɡ�
ECG 15-28
15-29 II,III,aVF��Q�Ȥ�V1V2��R�Ⱦ徺���Ť����ɸ��ɹ��ɡ�
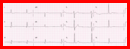 ECG 15-29
GE #57 V1��V3�ޤ�RS�ǹ⤤T�ȡ�V4��V6�˽��ä�R�ȤϾ�����V6��QS��STE��
�ߤ����Ȥ�̵���ȷ����������硩�ͻ����Ű̡�
���ɤ�AMI��V1��R�Ȥϸ��ɹ��ɤΤ��ᡤ�⤷���ɹ��ɤ�STE��ȯ������
�ޤǤδ֤Ǥ���С�V1��V3�ޤǤΥߥ顼STD��ȯ�����ʤ���V5��V6��STE��
������AMI����II,III,aVF���Ѳ��Ϥʤ����鱦��ư̮�����
���äơ��������ޤ��ĺɤˤ��¦�ɸ��ɹ��ɰʳ��˹ͤ����ʤ���
���ޤ�GE #57
���Ʊ�����ſޤΥȥ�ߥ�.
ECG 15-29
GE #57 V1��V3�ޤ�RS�ǹ⤤T�ȡ�V4��V6�˽��ä�R�ȤϾ�����V6��QS��STE��
�ߤ����Ȥ�̵���ȷ����������硩�ͻ����Ű̡�
���ɤ�AMI��V1��R�Ȥϸ��ɹ��ɤΤ��ᡤ�⤷���ɹ��ɤ�STE��ȯ������
�ޤǤδ֤Ǥ���С�V1��V3�ޤǤΥߥ顼STD��ȯ�����ʤ���V5��V6��STE��
������AMI����II,III,aVF���Ѳ��Ϥʤ����鱦��ư̮�����
���äơ��������ޤ��ĺɤˤ��¦�ɸ��ɹ��ɰʳ��˹ͤ����ʤ���
���ޤ�GE #57
���Ʊ�����ſޤΥȥ�ߥ�.
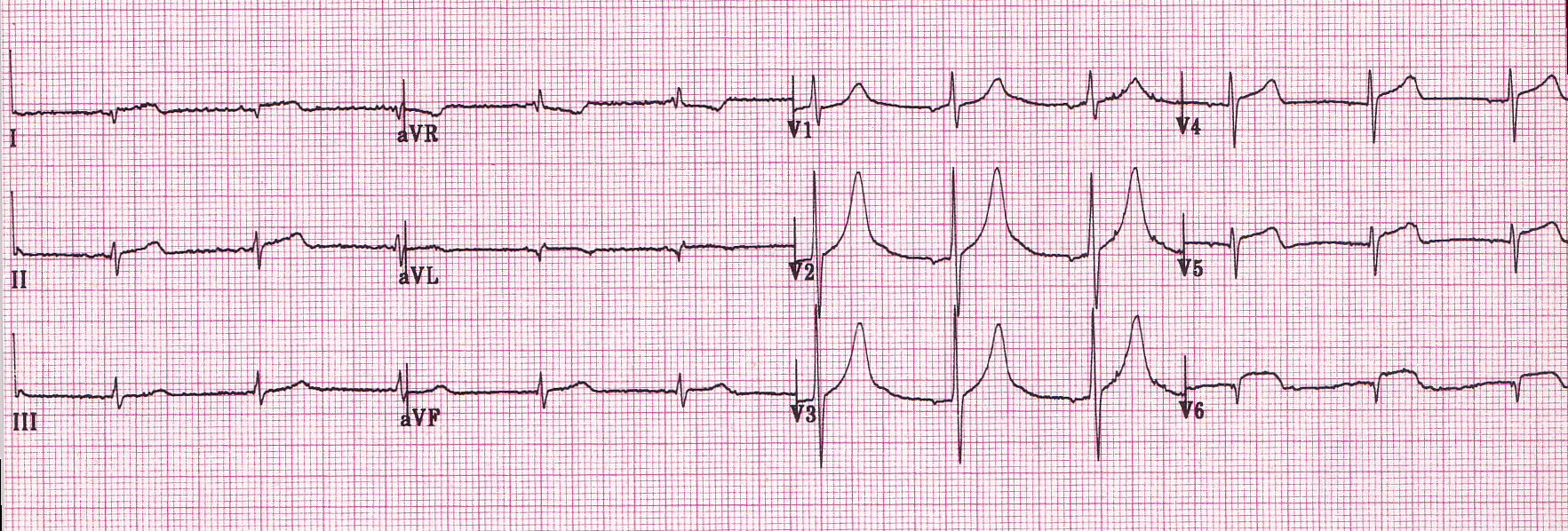
 15-22
���������ɡ�I��II��III��STE��aVR��STD��aVL�Ͽ�ʿ��V1��STD��V3-6�ޤǶ��٤�STE��
15-22
���������ɡ�I��II��III��STE��aVR��STD��aVL�Ͽ�ʿ��V1��STD��V3-6�ޤǶ��٤�STE��
 15-23
���������ɡ�I�Ϸ��٤�STE��II��III��STE��aVR��STD��aVL��ȿžT�ȡ���V1�����V2-6�ޤǶ��٤�STE��
15-23
���������ɡ�I�Ϸ��٤�STE��II��III��STE��aVR��STD��aVL��ȿžT�ȡ���V1�����V2-6�ޤǶ��٤�STE��
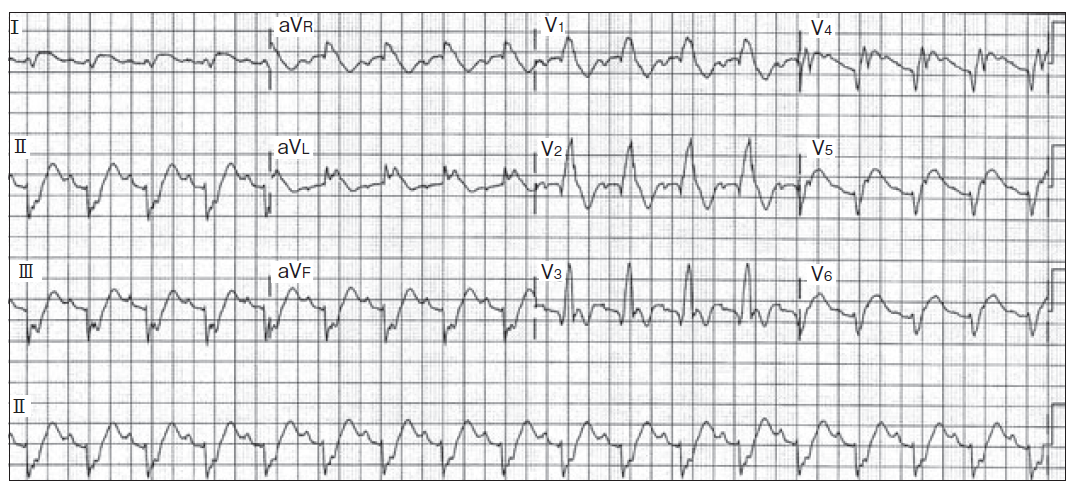
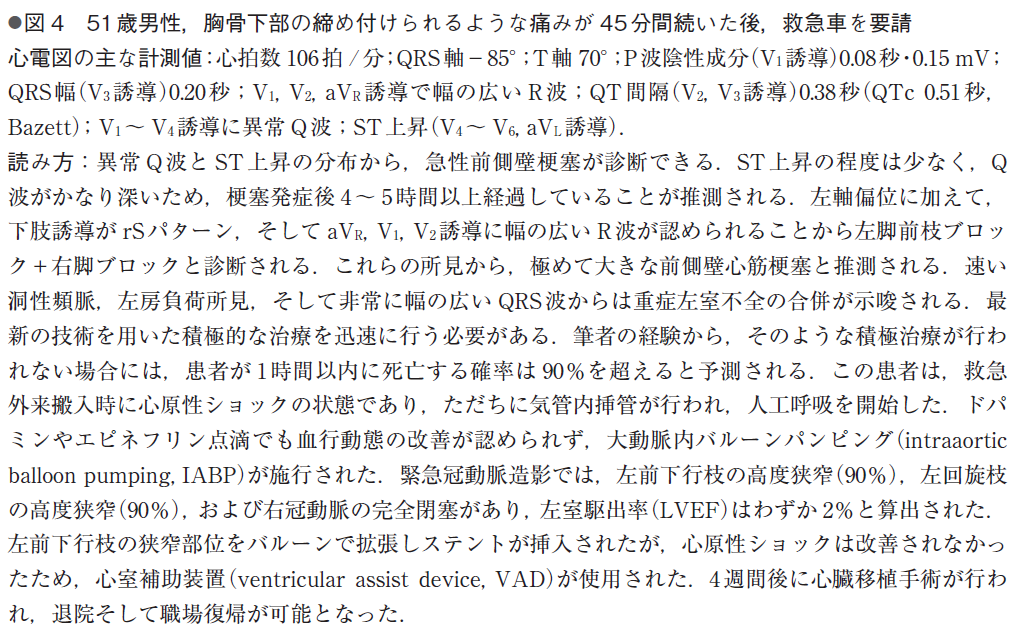
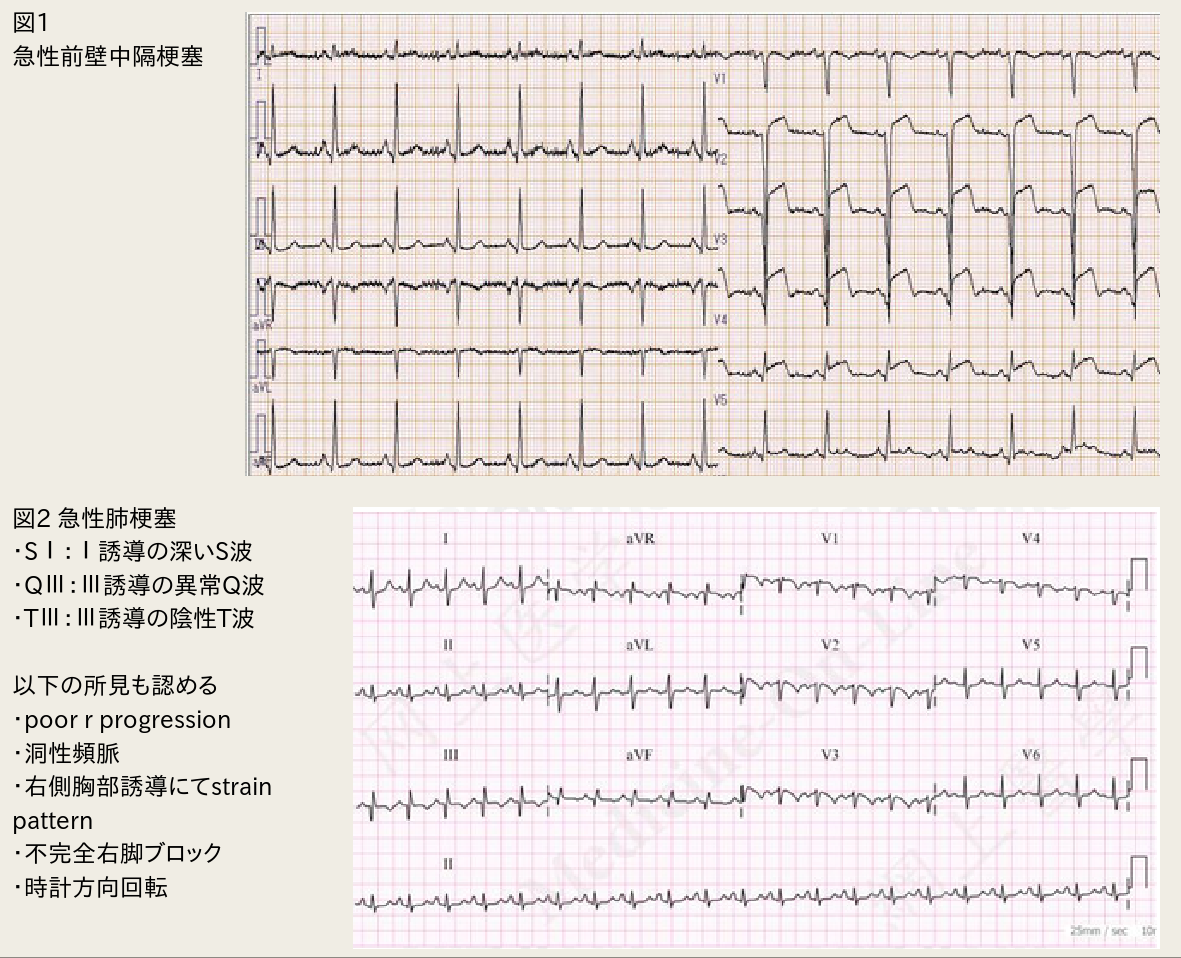 ���ޤ�LAFB�ˤ��PRP��ȯ�����Ƥ��뤬��V2��V5�ǤΥΥå���IVCD����
IVCD GE #243
���ޤ�LAFB�ˤ��PRP��ȯ�����Ƥ��뤬��V2��V5�ǤΥΥå���IVCD����
IVCD GE #243
 ���ɿ�����1
GE #328��ꡧ
���ɿ�����2
���ɿ�����
���ɿ�����1
GE #328��ꡧ
���ɿ�����2
���ɿ�����
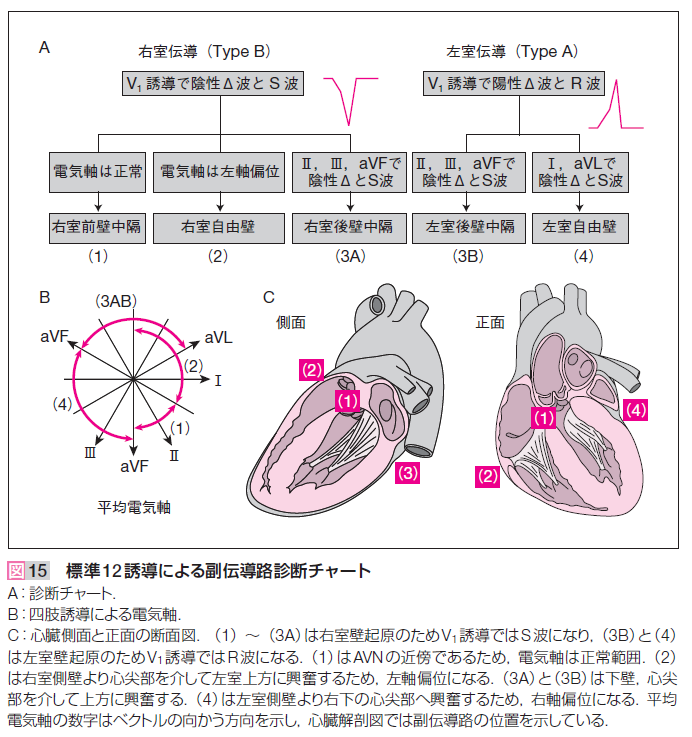 IMG_20170912_0002.pdf
IMG_20170912_0002.pdf��GE #190�������������ʤ�����
III��aVF�Υǥ륿�Ȥϥǥ륿�ȤǤϤʤ���
P-Rû�̤ǰ۾�Q�Ȥ�WPW�ɸ����ȴְ㤨�ʤ��褦�ˤ��ʤ���Фʤ�ʤ���
(12 Lead p.137���)
Type A:
V1�Ǿ�������ȡ����Ƥζ���ͶƳ��R�Ȥˤʤ롥����(Kent«)������Ƴϩ�����뤫��
���ӥ֥��å����˻��롥
Type B:
V1�Dz��������ȡ���¦����ͶƳ�Ͼ������R�Ȥˤʤ롥����������Ƴϩ�����뤫��
���ӥ֥��å����˻��롥
GE #186: �ַ�WPW��
Type C:
V1����V4�ޤǤϾ������V5, V6�ϲ�����S�ȡ����Ǥ��롥
Type B��II, III, aVF�α������ȤϿ��ڹ��ɤΰ۾�Q�Ȥȴְ㤨�䤹����
pseudoinfarct�Ȥ����Ƥ��롥Type A�ι⤤R�Ȥϸ��ɹ��ɤȴְ㤨�䤹����
IVCD�ȴְ㤦WPW��
GE #305 PQû�̡�IVCD��
���ǡ�WPW��V4-6��S�Ȥ�����Ǥ��ꡤIVCD������Ǥ��롥
��ʳ��Kent«���鿴�������ꡤ�չ�����AV node���䤹�뿴�������
antidromic�Ȥ�Ф�롥wide-complex tachycardia��VT�ȶ��̤Ǥ��ʤ���
����Ǥ��롥�ޤ�AF��Af�Ȥ�1:1�б������郎�ᤤ��
�դ�AV node����Kent«�˸������롼�פ�orthodromic�Ȥ�Ф�롥
������Ƴ�Ǥ��뤫��narrow-complex tachycardia�Ǥ��ꡤ�����٤��㤤��
AV node���ٱ䤬Ư������Ǥ��롥������٤���
����̮ƶ����˹�ۤ���¦�����Ԥ�������������֤˰��֤��롥
���Τ���ˡ�����̮ƶĴΧ��WPW����Ƴϩ�Ϻ�����������ն�ȹͤ����롥
wpw2.png
IMG_20170912_0002.pdf
IMG_20170912_0002.pdf��GE #190�������������ʤ�����
III��aVF�Υǥ륿�Ȥϥǥ륿�ȤǤϤʤ���
P-Rû�̤ǰ۾�Q�Ȥ�WPW�ɸ����ȴְ㤨�ʤ��褦�ˤ��ʤ���Фʤ�ʤ���
(12 Lead p.137���)
Type A:
V1�Ǿ�������ȡ����Ƥζ���ͶƳ��R�Ȥˤʤ롥����(Kent«)������Ƴϩ�����뤫��
���ӥ֥��å����˻��롥
Type B:
V1�Dz��������ȡ���¦����ͶƳ�Ͼ������R�Ȥˤʤ롥����������Ƴϩ�����뤫��
���ӥ֥��å����˻��롥
GE #186: �ַ�WPW��
Type C:
V1����V4�ޤǤϾ������V5, V6�ϲ�����S�ȡ����Ǥ��롥
Type B��II, III, aVF�α������ȤϿ��ڹ��ɤΰ۾�Q�Ȥȴְ㤨�䤹����
pseudoinfarct�Ȥ����Ƥ��롥Type A�ι⤤R�Ȥϸ��ɹ��ɤȴְ㤨�䤹����
IVCD�ȴְ㤦WPW��
GE #305 PQû�̡�IVCD��
���ǡ�WPW��V4-6��S�Ȥ�����Ǥ��ꡤIVCD������Ǥ��롥
��ʳ��Kent«���鿴�������ꡤ�չ�����AV node���䤹�뿴�������
antidromic�Ȥ�Ф�롥wide-complex tachycardia��VT�ȶ��̤Ǥ��ʤ���
����Ǥ��롥�ޤ�AF��Af�Ȥ�1:1�б������郎�ᤤ��
�դ�AV node����Kent«�˸������롼�פ�orthodromic�Ȥ�Ф�롥
������Ƴ�Ǥ��뤫��narrow-complex tachycardia�Ǥ��ꡤ�����٤��㤤��
AV node���ٱ䤬Ư������Ǥ��롥������٤���
����̮ƶ����˹�ۤ���¦�����Ԥ�������������֤˰��֤��롥
���Τ���ˡ�����̮ƶĴΧ��WPW����Ƴϩ�Ϻ�����������ն�ȹͤ����롥
wpw2.png
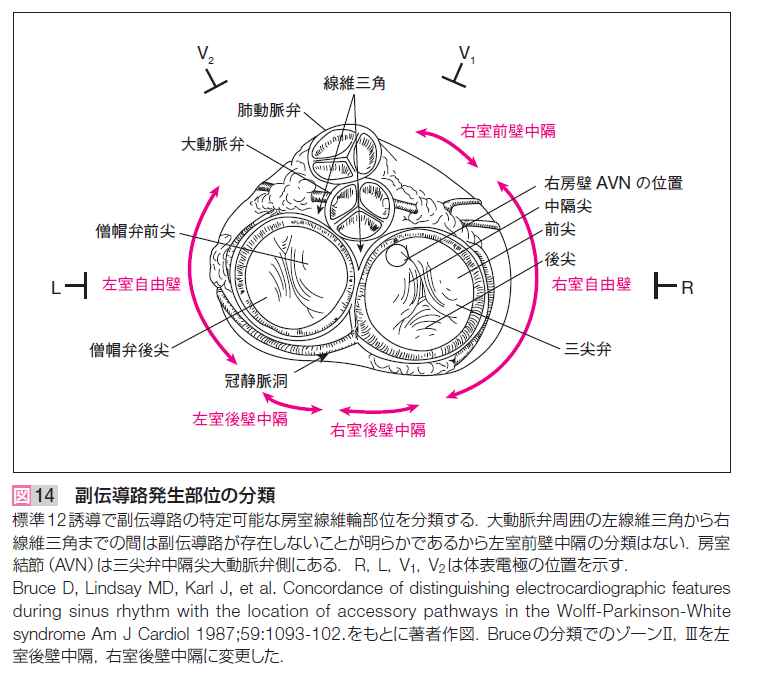 ����̮ƶĴΧ�ˤ��WPW�ȷ�
2018ǯ12��22��(ECG4.doc)���
����� 80��P�� 118, QRS�� 77, T�� 85
wpw3.pdf
����̮ƶĴΧ�ˤ��WPW�ȷ�
2018ǯ12��22��(ECG4.doc)���
����� 80��P�� 118, QRS�� 77, T�� 85
wpw3.pdf
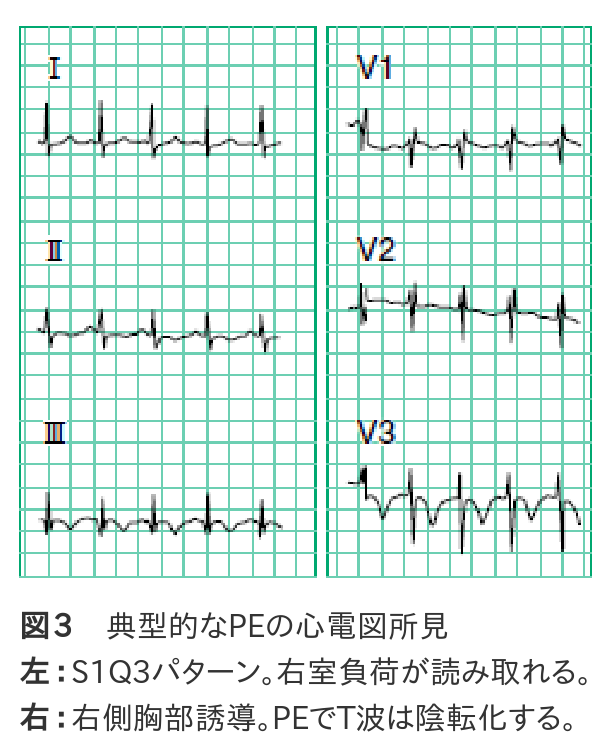 ����PE�ο��ſ긫�Ǥϡ�������S1Q3�α�����٥ѥ�����ʿ�3���ˤ�ͭ̾�Ǥ�����
�ߤ��������٤�30��ʲ��Ǥ���������ž��٤ȤϤ��ޤ���ؤ��ޤ���
�¤ϡ�������ⱦ¦����ͶƳ��V1-3�ˤ�T�Ȥ��Ѳ��Τۤ���ͽ���褯ȿ�Ǥ��ޤ��ʿ�3���ˡ�
��������ǰ�ʤ��顤����������ˤˤߤ�����긫�ǤϤ���ޤ���
McGinn-White��pattern�Ȥ�S1Q3T3�ο��ſޤ���
II��III�α���T�Ȥϲ��ɤε���긫��Ʊ����
V1��V3�α���T�Ȥ�������������T�Ȥ�����Ǥ���Τ�
���餫�˰۾�Ǥ��롥
T�٥��ȥ뤬�����˸������긫�Ȥ����Ƥ��뤬��
�������ڤγ�ĥ�������ȼ��������¦���ڤ������ʬ��
�ˤ��۾�ȹͤ��롥
PE�Ǥϱ�����ĥ���뤬����������ˤϤʤ�ʤ������Τ���V1��R�ȤϾ�������
V1��rSR'�ϱ�������Ǥⶦ�̤���긫�Ǥ��롥V6��S�Ȥơ��������ޤ����
���ӥ֥��å��ǤϤʤ���S1��S�Ȥ�����������
BB p.76, fig7.19 �ٹ��ɡ�S1Q3T3��I��rS�ˤ�뱦���а̡�V1��qR�ޤ���rR'��V6��RS�����ײ�ž��
����PE�ο��ſ긫�Ǥϡ�������S1Q3�α�����٥ѥ�����ʿ�3���ˤ�ͭ̾�Ǥ�����
�ߤ��������٤�30��ʲ��Ǥ���������ž��٤ȤϤ��ޤ���ؤ��ޤ���
�¤ϡ�������ⱦ¦����ͶƳ��V1-3�ˤ�T�Ȥ��Ѳ��Τۤ���ͽ���褯ȿ�Ǥ��ޤ��ʿ�3���ˡ�
��������ǰ�ʤ��顤����������ˤˤߤ�����긫�ǤϤ���ޤ���
McGinn-White��pattern�Ȥ�S1Q3T3�ο��ſޤ���
II��III�α���T�Ȥϲ��ɤε���긫��Ʊ����
V1��V3�α���T�Ȥ�������������T�Ȥ�����Ǥ���Τ�
���餫�˰۾�Ǥ��롥
T�٥��ȥ뤬�����˸������긫�Ȥ����Ƥ��뤬��
�������ڤγ�ĥ�������ȼ��������¦���ڤ������ʬ��
�ˤ��۾�ȹͤ��롥
PE�Ǥϱ�����ĥ���뤬����������ˤϤʤ�ʤ������Τ���V1��R�ȤϾ�������
V1��rSR'�ϱ�������Ǥⶦ�̤���긫�Ǥ��롥V6��S�Ȥơ��������ޤ����
���ӥ֥��å��ǤϤʤ���S1��S�Ȥ�����������
BB p.76, fig7.19 �ٹ��ɡ�S1Q3T3��I��rS�ˤ�뱦���а̡�V1��qR�ޤ���rR'��V6��RS�����ײ�ž��
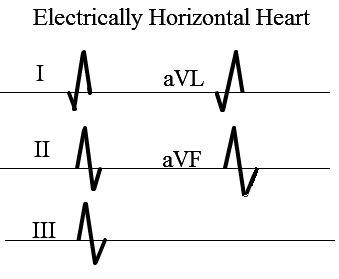 I��aVF��II��aVF�ϻ��Ƥ��롥
S1S2S3�����꼴�ˤʤ롥
I��aVF��II��aVF�ϻ��Ƥ��롥
S1S2S3�����꼴�ˤʤ롥
 ��¡��ȿ����������ž�����С�
V1��V6��R�Ȥ����ˤǤ롥
EMS 12 Lead
Prominent R Wave in Lead V1: Electrocardiographic Differential Diagnosis.
Mattu, Brady, et al.
Am J Emerg Med 2001;19:504-513.
Right bundle branch block
Left ventricular ectopy
Right ventricular hypertrophy
Acute right ventricular dilation
Wolff-Parkinson-White syndrome Type A
Posterior myocardial infarction
Hypertrophic cardiomyopathy
Progressive muscular dystrophy
Dextrocardia
Misplaced precordial leads
Normal variant
��¡��ȿ����������ž�����С�
V1��V6��R�Ȥ����ˤǤ롥
EMS 12 Lead
Prominent R Wave in Lead V1: Electrocardiographic Differential Diagnosis.
Mattu, Brady, et al.
Am J Emerg Med 2001;19:504-513.
Right bundle branch block
Left ventricular ectopy
Right ventricular hypertrophy
Acute right ventricular dilation
Wolff-Parkinson-White syndrome Type A
Posterior myocardial infarction
Hypertrophic cardiomyopathy
Progressive muscular dystrophy
Dextrocardia
Misplaced precordial leads
Normal variant
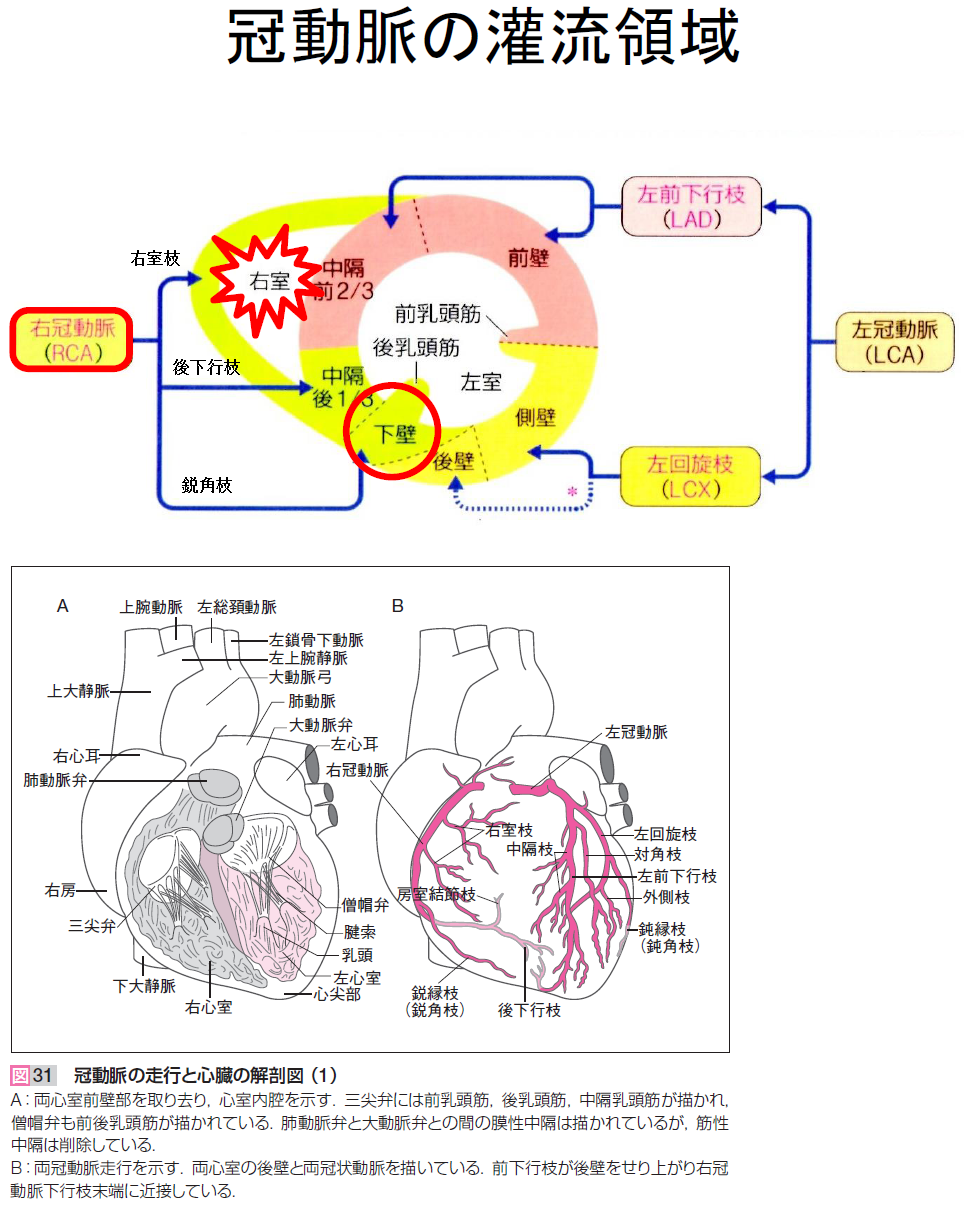
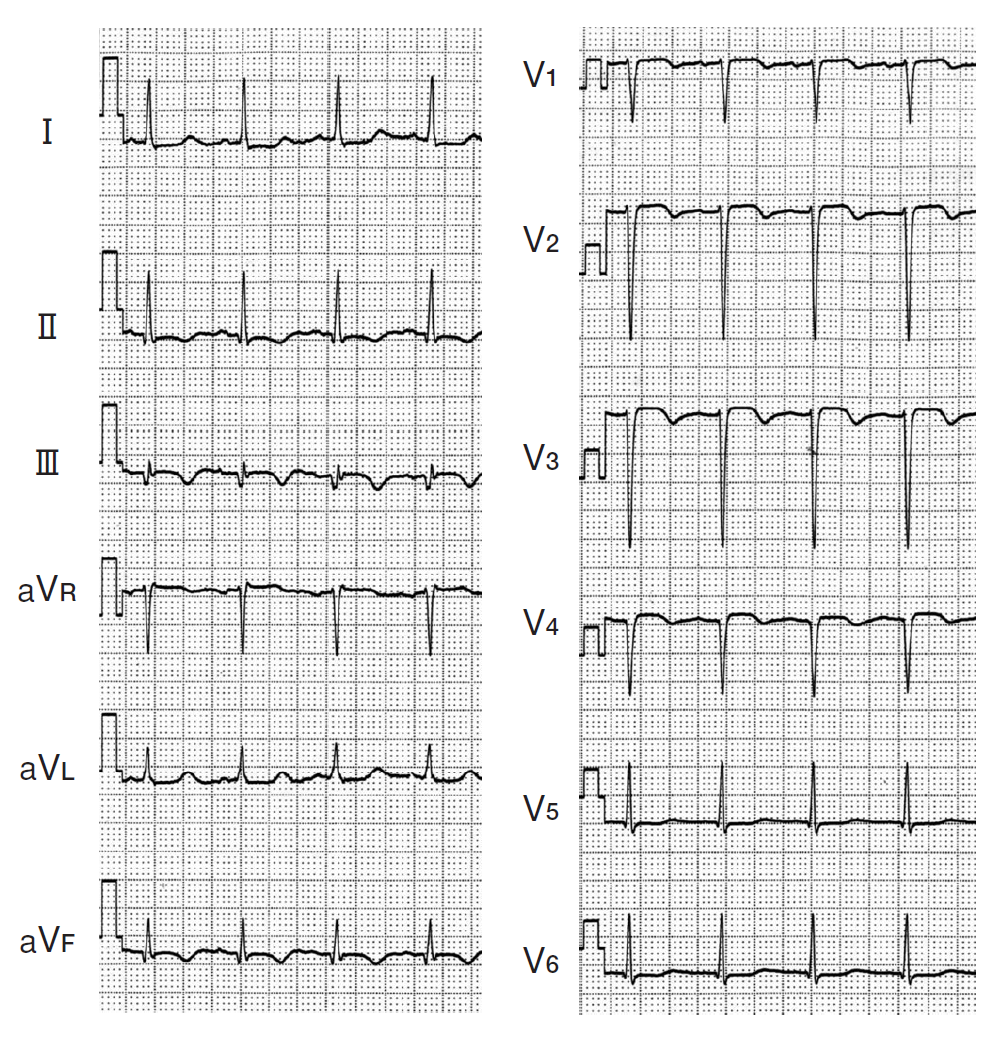 II, III, aVF�ξ�����q�ȡ�����T�Ȥ����ա�
II, III, aVF�ξ�����q�ȡ�����T�Ȥ����ա�
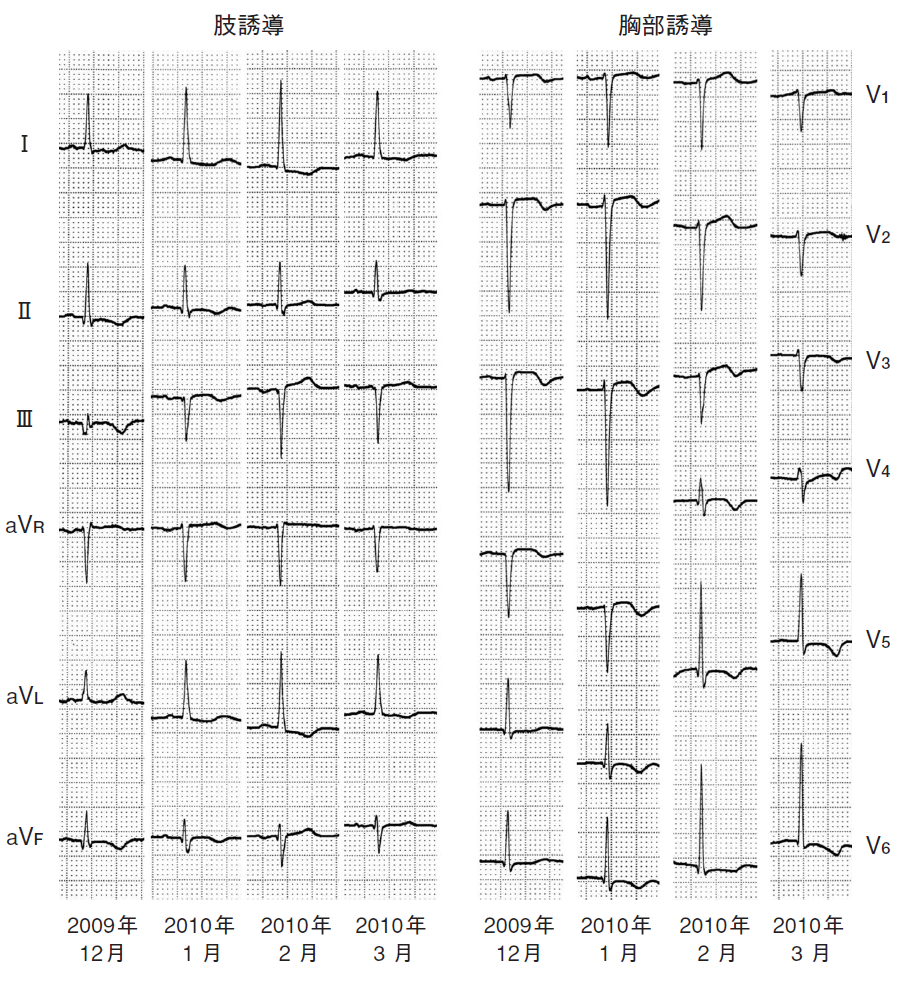
 2:1��AFĴΧ����Phase 3�κ��ӥ֥��å������ѹ���Ƴ��3Ϣȯ³�������θ�1:1��AF��PSVT�ˤʤäƤ��롥
3Ϣȯ��QRS���������ʤ���ͳ�Ϻ��ӥ֥��å������δ֤˲������줿����Ǥ��롥
aberrant.pdf
abe1.pdf
abe2.pdf
�� retrograde concealed conduction �չ����Ը�����Ƴ
�ӥ֥��å��ζ�ʳ��Ƴ��¾¦�����Ť���Ȥ���ϰ��̿��ڤ���Ƴ�ˤʤ롥
���ο��ڶ�ʳ���չ����˻ɷ���Ƴ�Ϥ�ʳ�����뤿�ᡤ�Ƥӵӥ֥��å���
��³���뤳�Ȥ��̣���롥SVT�ΰ���Ū�ʽ긫�Ǥ��롥
�� IKur��IKs��æʬ�˽�λ�夹������K����ͥ���Ĥ��뤬��
IKr��K����ͥ�γ������֤����Ф餯��³���롥
��K��ɤˤʤ�ȡ����λ�³�������̤����夹�롥�������ä�LQT����K��ɤˤ�
���դ�ɬ�פǤ��롥
cf. Channel.pdf.
�� concealed conduction �Ը�����Ƴ
PVC�θ塤����ƶĴΧ����»�����硤PVC���չ�����AV Node��ɷ㤷��
�Ա����ˤʤ뤿�����ĴΧ����Ƴ����������뤿��Ǥ��롥
2:1��AFĴΧ����Phase 3�κ��ӥ֥��å������ѹ���Ƴ��3Ϣȯ³�������θ�1:1��AF��PSVT�ˤʤäƤ��롥
3Ϣȯ��QRS���������ʤ���ͳ�Ϻ��ӥ֥��å������δ֤˲������줿����Ǥ��롥
aberrant.pdf
abe1.pdf
abe2.pdf
�� retrograde concealed conduction �չ����Ը�����Ƴ
�ӥ֥��å��ζ�ʳ��Ƴ��¾¦�����Ť���Ȥ���ϰ��̿��ڤ���Ƴ�ˤʤ롥
���ο��ڶ�ʳ���չ����˻ɷ���Ƴ�Ϥ�ʳ�����뤿�ᡤ�Ƥӵӥ֥��å���
��³���뤳�Ȥ��̣���롥SVT�ΰ���Ū�ʽ긫�Ǥ��롥
�� IKur��IKs��æʬ�˽�λ�夹������K����ͥ���Ĥ��뤬��
IKr��K����ͥ�γ������֤����Ф餯��³���롥
��K��ɤˤʤ�ȡ����λ�³�������̤����夹�롥�������ä�LQT����K��ɤˤ�
���դ�ɬ�פǤ��롥
cf. Channel.pdf.
�� concealed conduction �Ը�����Ƴ
PVC�θ塤����ƶĴΧ����»�����硤PVC���չ�����AV Node��ɷ㤷��
�Ա����ˤʤ뤿�����ĴΧ����Ƴ����������뤿��Ǥ��롥
 Iipes & Jelife
Cardiac Electrophysiology Frim Cell to Bedside
Figure 80-6
Figure 80-4
Iipes & Jelife
Cardiac Electrophysiology Frim Cell to Bedside
Figure 80-6
Figure 80-4
 wakaru3.1pdf p.41��ꡥ
wakaru3.1pdf p.41��ꡥ



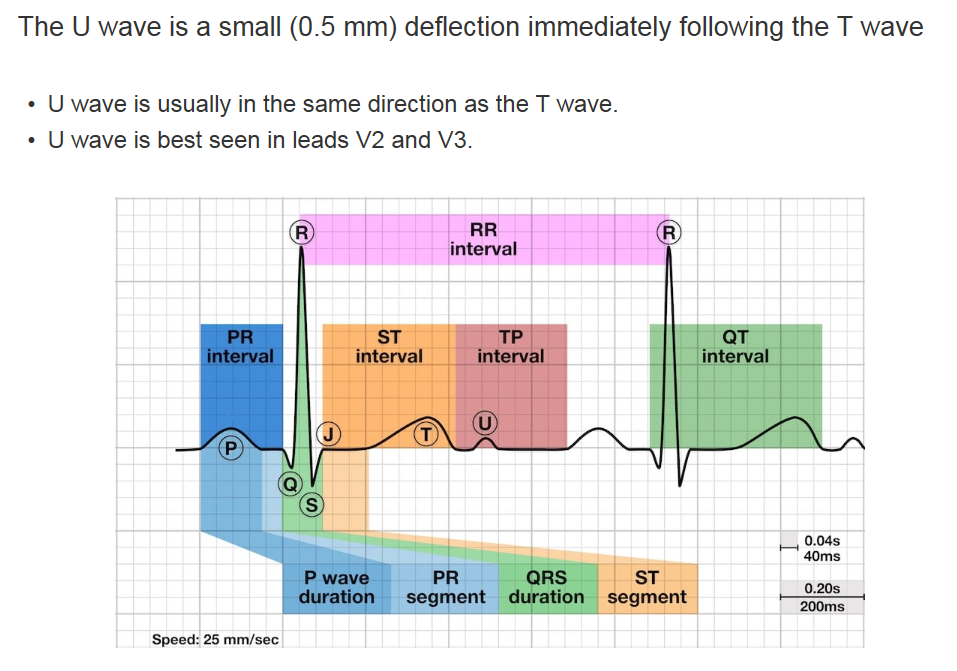 U�Ȥ�ȯ�������������Ǥ��뤬��Purkinje fiber���ٱ�����ʬ�ˡ�
M-cell���ٱ�����ʬ�ˡ�
�����ɤ�ʪ��Ū��ư�������Ƥ��롥
U�Ȥ�ȯ�������������Ǥ��뤬��Purkinje fiber���ٱ�����ʬ�ˡ�
M-cell���ٱ�����ʬ�ˡ�
�����ɤ�ʪ��Ū��ư�������Ƥ��롥
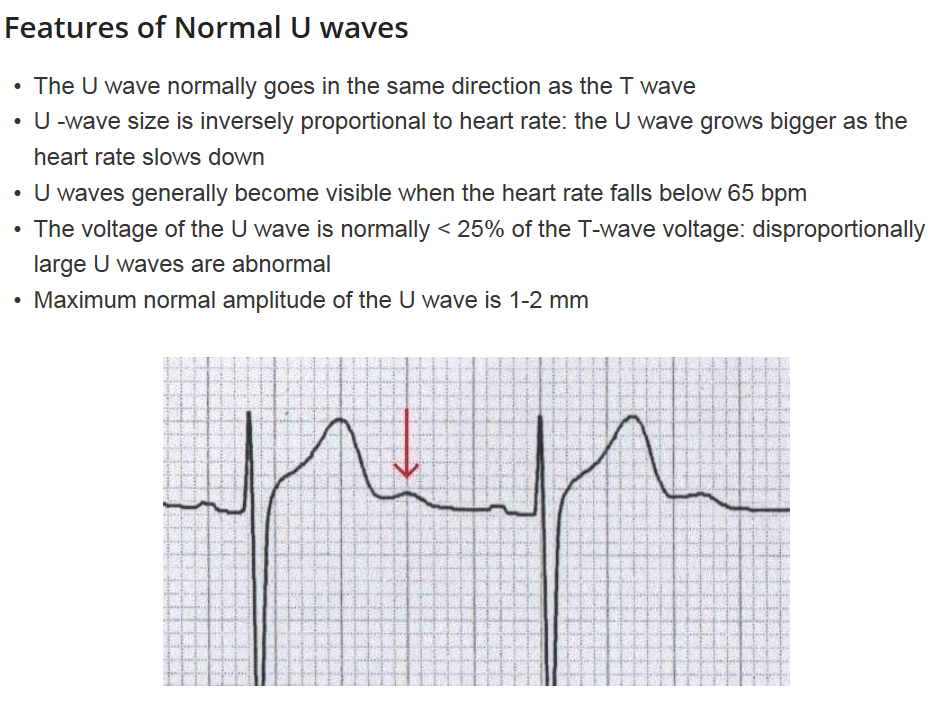 �۾�U�ȤȤϡ�
�۾�ˤ�������U�� (Prominent U waves)
>1-2mm �ޤ��ϡ� T�Ȥ� 25�۾�ι⤵��
������
����̮�����٤���K���
������¾����Ca��ɡ���Mg��ɡ����β���Ǿ��ж�ʡ��������硤���������ھ�
���������ˤ�
��Digoxin, Phenothiazines (thioiazine),
��Ia ������̮�� (quinidine, procainamide),
III ������̮�� (sotalol, amiodarone)
��žU�� (iInverted U waves)
������
����ư̮��������찵���ۼ�������ŷ�������������ھɡ���þ�����
��Prinzmetal angina(�۷�������)
U wave ��ư̮����
uwave.pdf
�۾�U�ȤȤϡ�
�۾�ˤ�������U�� (Prominent U waves)
>1-2mm �ޤ��ϡ� T�Ȥ� 25�۾�ι⤵��
������
����̮�����٤���K���
������¾����Ca��ɡ���Mg��ɡ����β���Ǿ��ж�ʡ��������硤���������ھ�
���������ˤ�
��Digoxin, Phenothiazines (thioiazine),
��Ia ������̮�� (quinidine, procainamide),
III ������̮�� (sotalol, amiodarone)
��žU�� (iInverted U waves)
������
����ư̮��������찵���ۼ�������ŷ�������������ھɡ���þ�����
��Prinzmetal angina(�۷�������)
U wave ��ư̮����
uwave.pdf
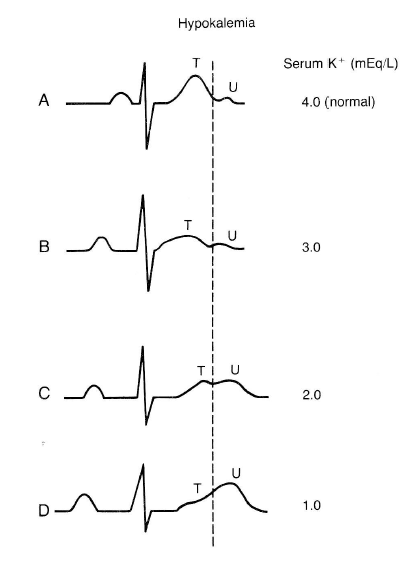 ��K��ɤˤʤ��U�Ȥ��и���PR�ֳ֤ϱ�Ĺ���롥
�̾����K��ɤ�U�Ȥ�ȯ�����뤬������ʳ���Ǿ�����ȯ�����롥
��K��ɤˤʤ��U�Ȥ��и���PR�ֳ֤ϱ�Ĺ���롥
�̾����K��ɤ�U�Ȥ�ȯ�����뤬������ʳ���Ǿ�����ȯ�����롥
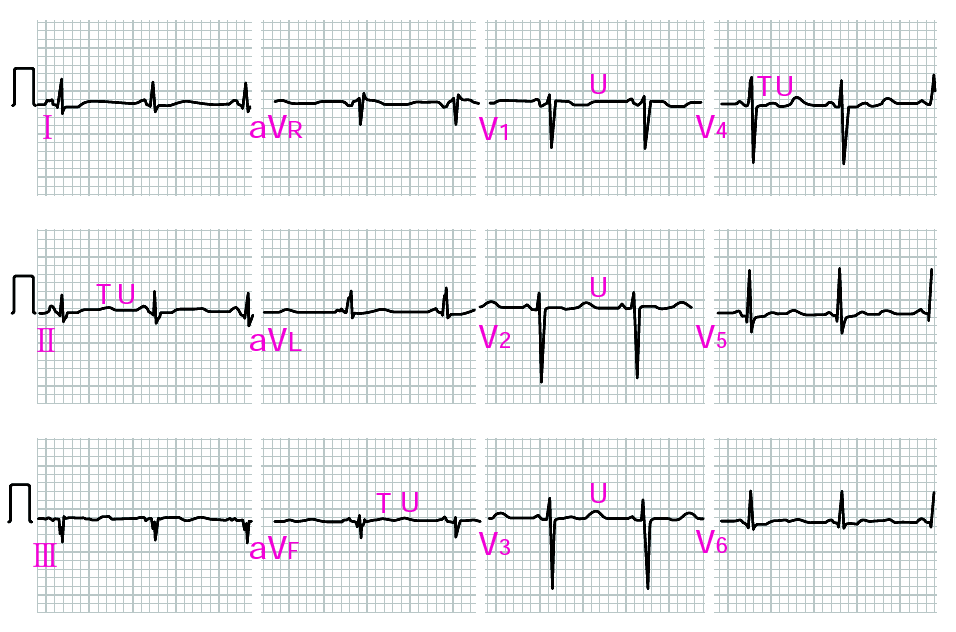 ����K+ǻ�٤�1.4mEq/L���㲼������ȯ������ɥ��ƥ��Ԥο��ſޡ�
Utah ECG Uwave
The U wave is the only remaining enigma of the ECG, and probably not for long. The origin of the U wave is still in question, although most authorities correlate the U wave with electrophysiologic events called "afterdepolarizations" in the ventricles. These afterdepolarizations can be the source of arrhythmias caused by "triggered automaticity" including torsade de pointes. The normal U wave has the same polarity as the T wave and is usually less than one-third the amplitude of the T wave. U waves are usually best seen in the right precordial leads especially V2 and V3. The normal U wave is asymmetric with the ascending limb moving more rapidly than the descending limb (just the opposite of the normal T wave).
����K+ǻ�٤�1.4mEq/L���㲼������ȯ������ɥ��ƥ��Ԥο��ſޡ�
Utah ECG Uwave
The U wave is the only remaining enigma of the ECG, and probably not for long. The origin of the U wave is still in question, although most authorities correlate the U wave with electrophysiologic events called "afterdepolarizations" in the ventricles. These afterdepolarizations can be the source of arrhythmias caused by "triggered automaticity" including torsade de pointes. The normal U wave has the same polarity as the T wave and is usually less than one-third the amplitude of the T wave. U waves are usually best seen in the right precordial leads especially V2 and V3. The normal U wave is asymmetric with the ascending limb moving more rapidly than the descending limb (just the opposite of the normal T wave).
Giant U waves: an important clinical clue The patient U wave Book�����Ѥ���U�ȵ��� Google: Hypothesis 2: delayed repolarization ���Ǥ�����줿������ uwave/uwave1.png
uwave/uwave2.png
uwave/uwave3.png
uwave/uwave4.png
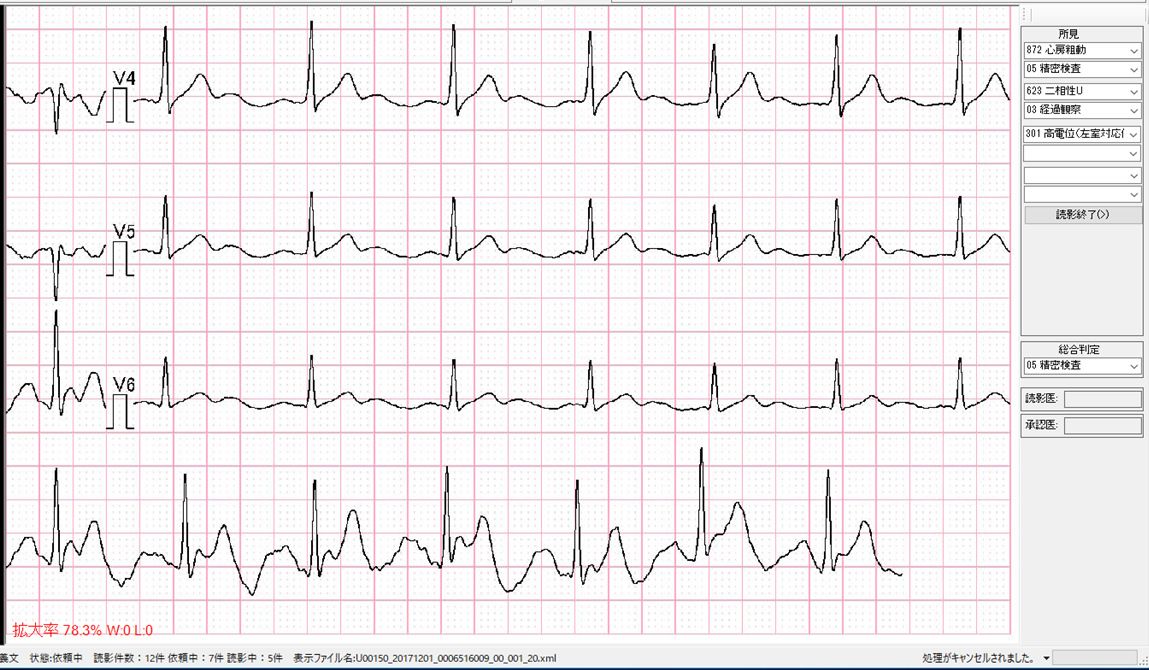
 35_195.pdf��ꡥJ�ȤϥΥå��ͤǤ��롥����ľ��������T�ȤˤʤäƤ��ꡤ
��ʿ��ʬ���ʤ���0:00�Ǥ�J�ȤϾ�������2:00���礭����Ĺ���Ƥ��롥
3:00�Ǥ�T�Ȥν�λ����R�Ȥ�ȯ�������줬R on T�Ǥ��ꡤvf�˰ܹԤ��롥
���͡�final p.76 Ito�ˤ���ʬ�ˤ�Brugada 2�����롥
35_195.pdf��ꡥJ�ȤϥΥå��ͤǤ��롥����ľ��������T�ȤˤʤäƤ��ꡤ
��ʿ��ʬ���ʤ���0:00�Ǥ�J�ȤϾ�������2:00���礭����Ĺ���Ƥ��롥
3:00�Ǥ�T�Ȥν�λ����R�Ȥ�ȯ�������줬R on T�Ǥ��ꡤvf�˰ܹԤ��롥
���͡�final p.76 Ito�ˤ���ʬ�ˤ�Brugada 2�����롥
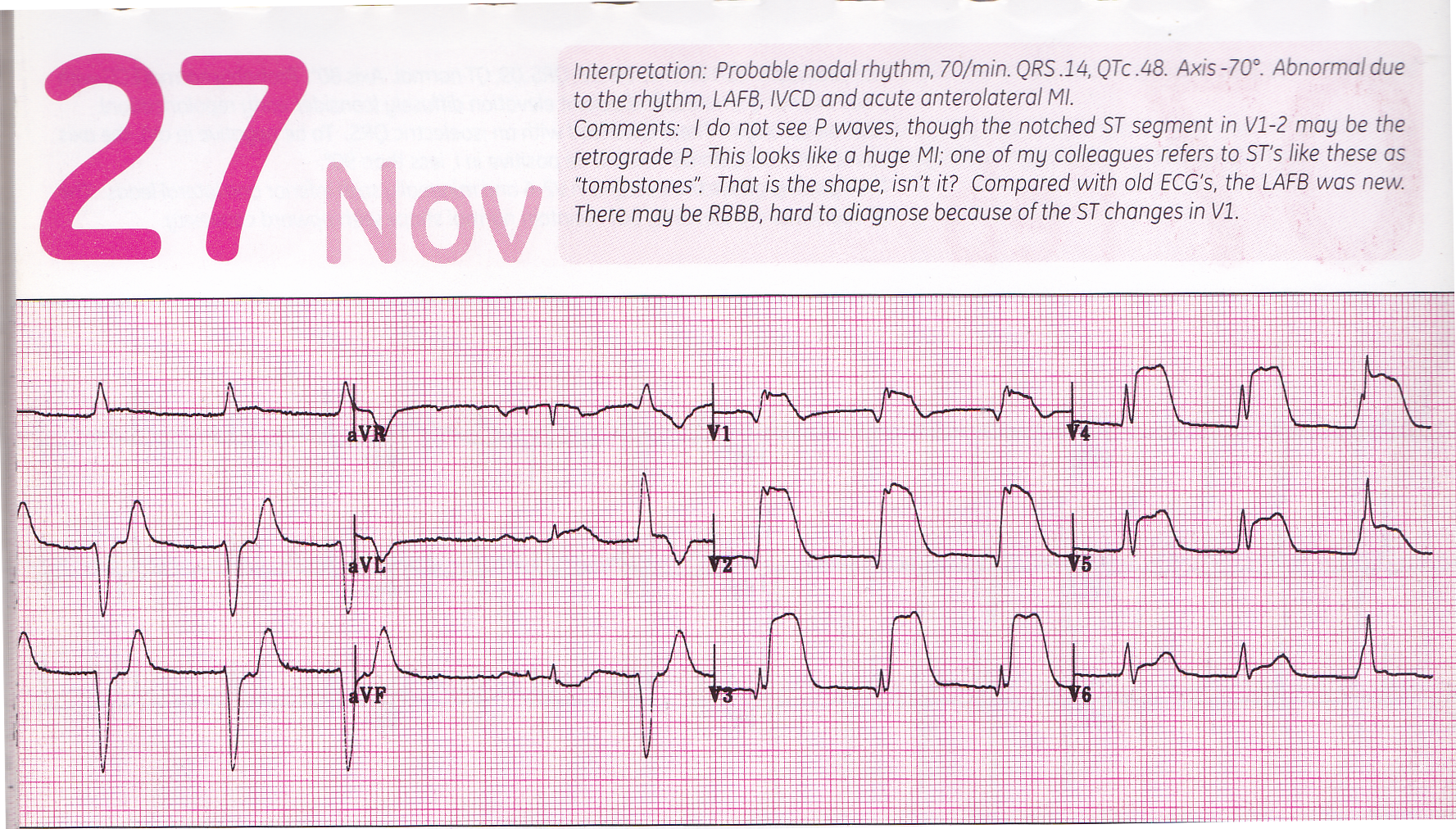 GE #312 (tombstone) IMG_20180625_0001-a.png
GE #312 (tombstone) IMG_20180625_0001-a.png
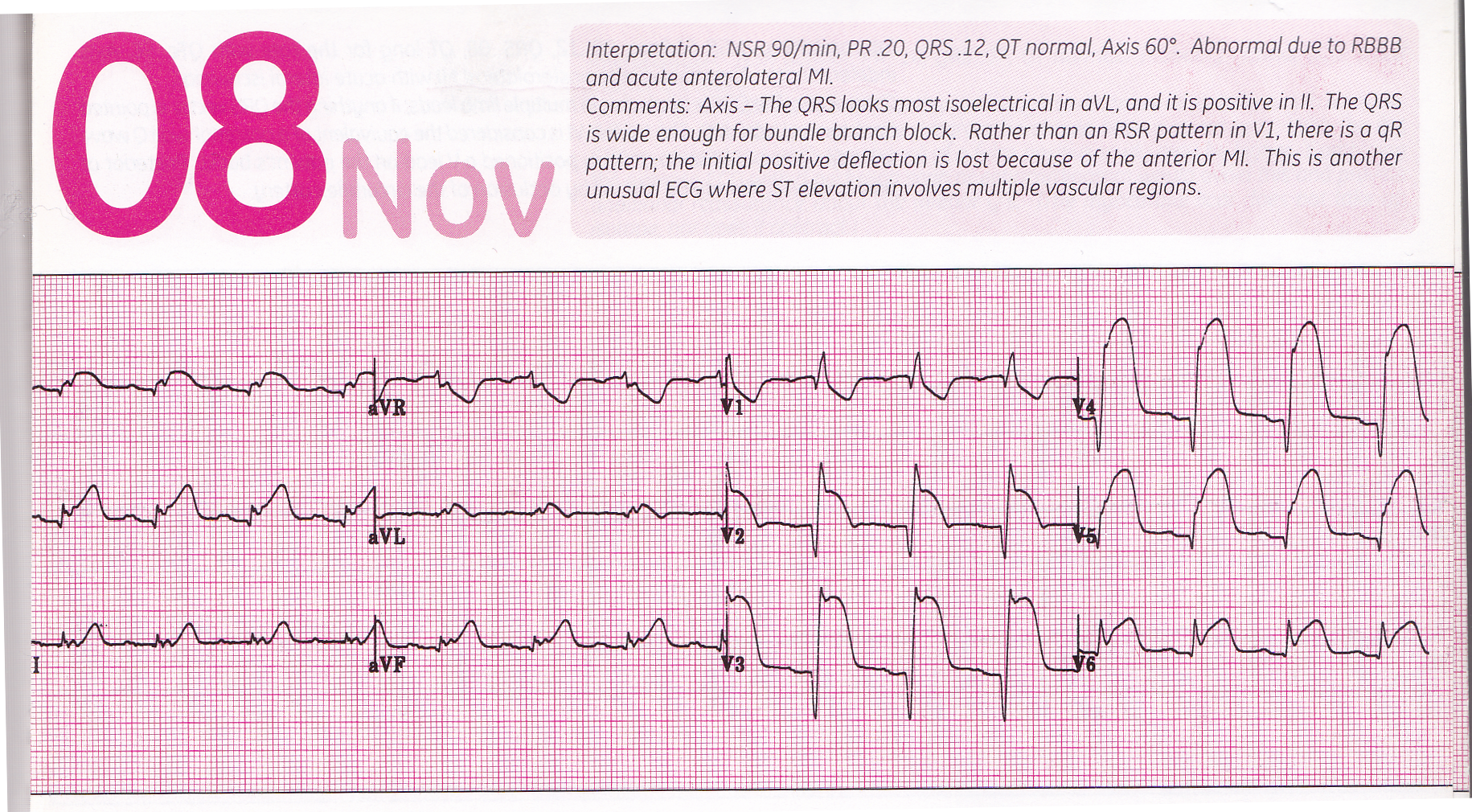
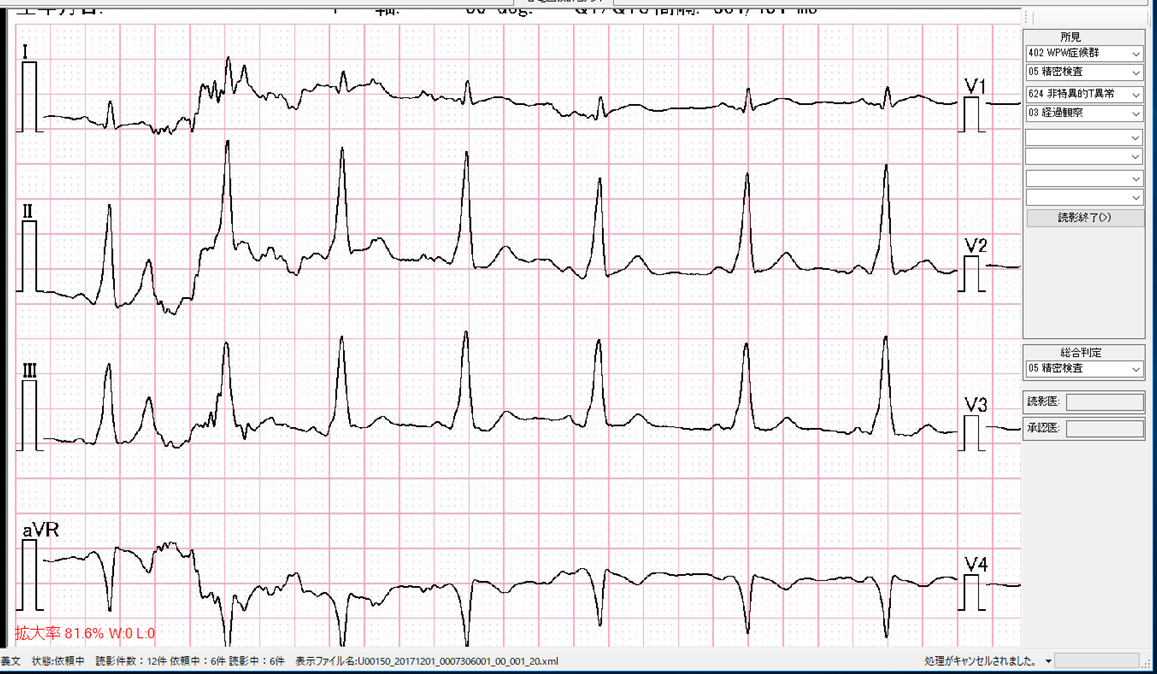 uwave/delta2.png
uwave/delta2.png
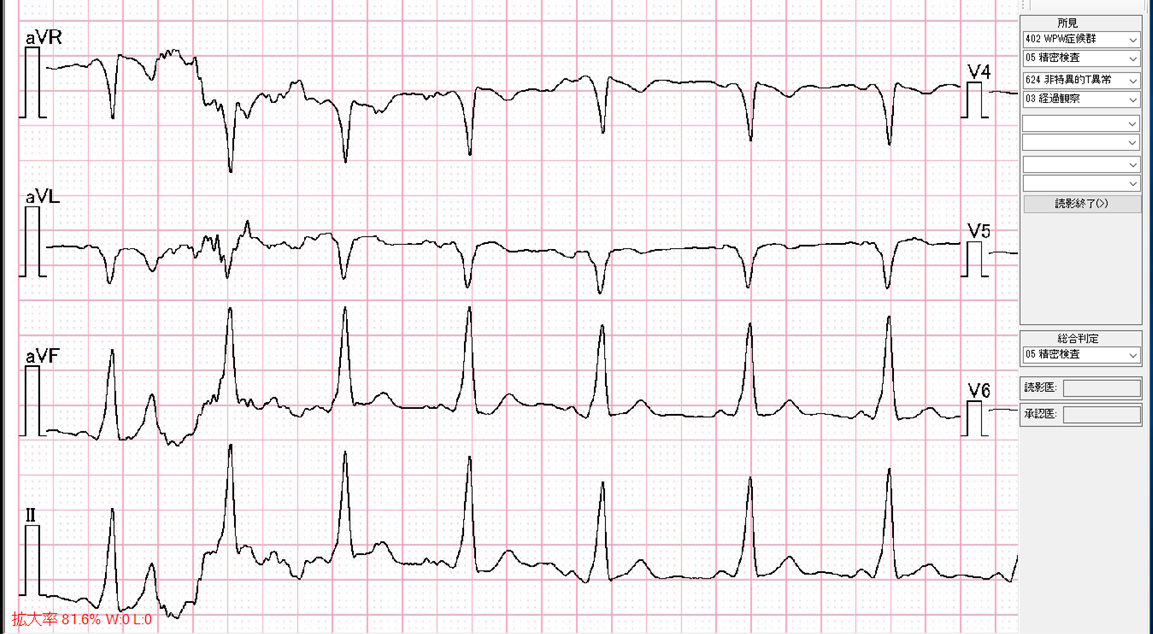 uwave/delta3.png
uwave/delta3.png
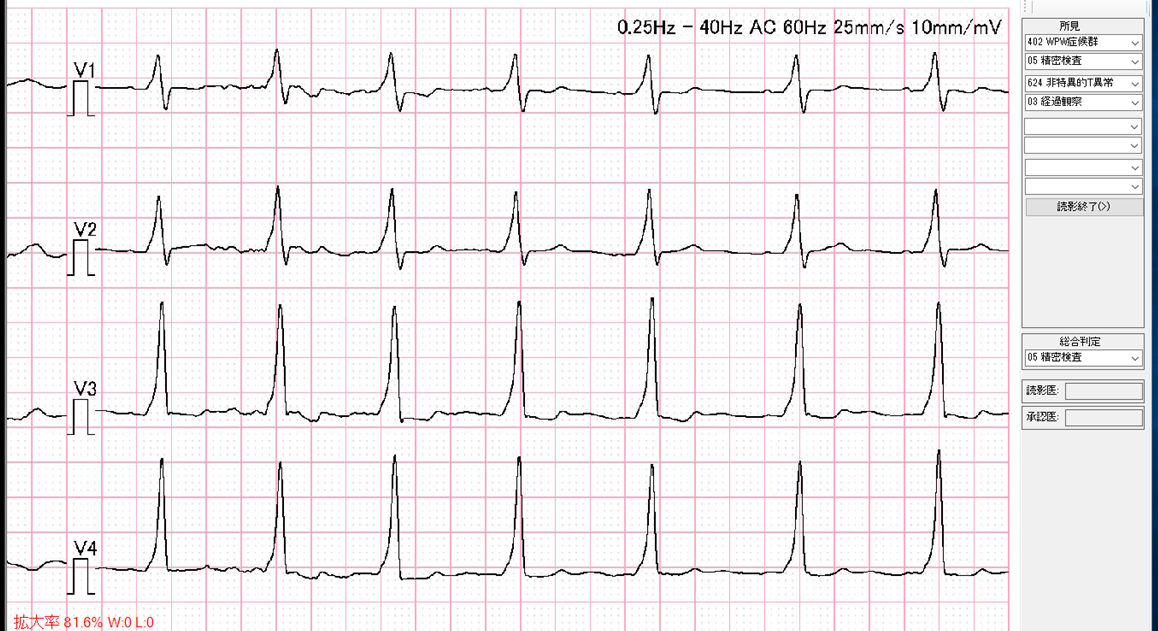 uwave/delta4.png
uwave/delta4.png
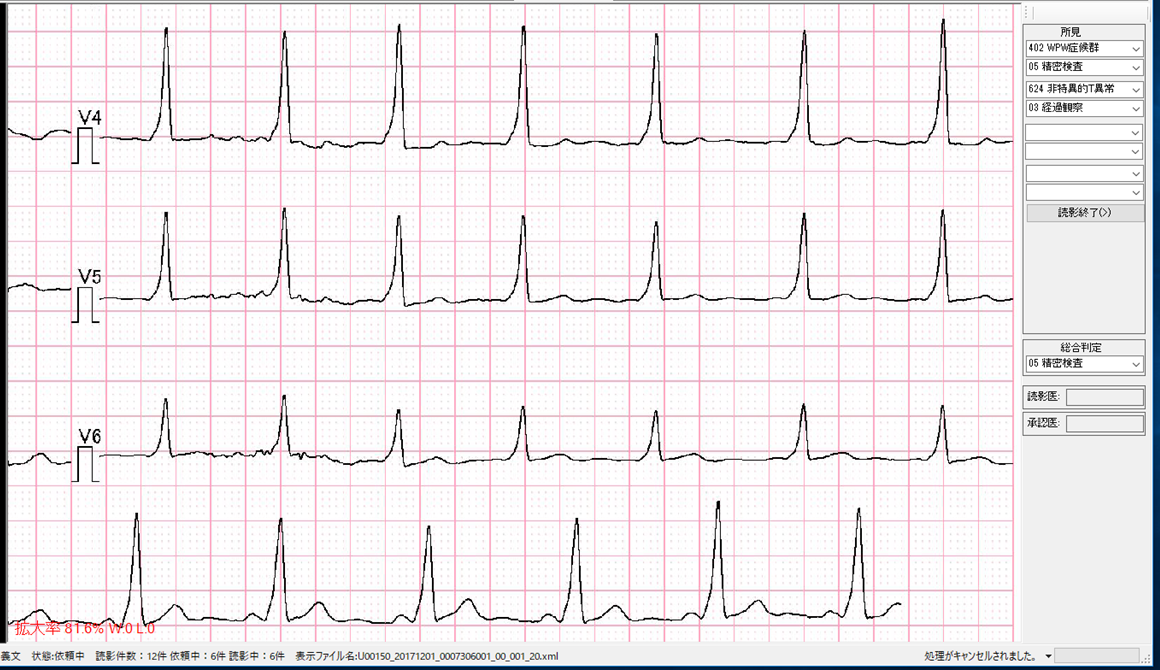
 final p.18���
final p.18���
 final p.136���
final p.136���